| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 16, Number 6, June 2024, pages 310-318
Mapping the Grounds for Mortalities in Acute Myeloid Leukemia Through Registry Analyses: A Retrospective Cohort Study of Children, Adolescents, and Young Adults Patients
Anas Elgenidya, s, Mohammed Al-Mahdi Al-Kurdib, s, Hoda Atef Abdelsattar Ibrahimc , Eman F. Gadd, Ahmed K. Awade, Rebecca Caruanaf, Sheriseane Diaconof, Aya Sherifg, Tasneem Elattarh, Islam E. Al-Ghaname, Asmaa M. Eldmatya, Tareq M. Abubasheeri, Ahmed M. Afifij, Amira Elhoufeyk, l, Hamad Ghaleb Dailahm, Amira M. Osmann, Mohamed Ezzato, Doaa Ali Gamalp, Rady Elmonierq, Ahmed El-Sayed Hammouro, Maged T. Abougabalr, Khaled Saadd, t
aFaculty of Medicine, Cairo University, Cairo, Egypt
bFaculty of Medicine, University of Aleppo, Aleppo, Syrian Arab Republic
cDepartment of Pediatrics, Faculty of Medicine, Cairo University, Cairo 12613, Egypt
dDepartment of Pediatrics, Assiut University, Assiut 71516, Egypt
eFaculty of Medicine Ain-Shams University, Cairo, Egypt
fMater dei Hospital, Msida, Malta
gFaculty of Medicine, Beni Suef University, Beni Suef, Egypt
hFaculty of Clinical Pharmacy, Al Azhar University, Cairo, Egypt
iFaculty of Medicine, Al-Quds University, Palestine
jDepartment of Surgery, University of Toledo Medical Center, Toledo, OH, USA
kDepartment of Community Health Nursing, Alddrab University College, Jazan University, Jazan 45142, Saudi Arabia
lDepartment of Community Health Nursing, Faculty of Nursing, Assiut University, Assiut, Egypt
mResearch and Scientific Studies Unit, College of Nursing, Jazan University, Jazan, Saudi Arabia
nDepartment of Pediatric Oncology, South Egypt Cancer Institute, Assiut University, Assiut, Egypt
oDepartment of Pediatrics, Faculty of Medicine, Al Azhar University, Cairo, Egypt
pDepartment of Clinical Oncology, Faculty of Medicine, Assiut University, Assiut, Egypt
qDepartment of Internal Medicine, Faculty of Medicine, Al-Azhar University, New Damietta, Egypt
rDepartment of Pediatrics, Zagazig University, Zagazig, Egypt
sThese authors contributed equally to this article.
tCorresponding Author: Khaled Saad, Department of Pediatrics, Assiut University Children’s Hospital, Assiut University Campus, Assiut 71111, Egypt
Manuscript submitted May 14, 2024, accepted May 31, 2024, published online June 30, 2024
Short title: Mortalities in AML Through Registry Analyses
doi: https://doi.org/10.14740/jocmr5205
| Abstract | ▴Top |
Background: Our objective was to identify non-malignant factors that contribute to mortality in children, adolescents and young adults, aiming to improve patient follow-up and reduce mortality rates to achieve better survival outcomes.
Methods: We analyzed 8,239 acute myeloid leukemia (AML) cases diagnosed between 2000 and 2019 in the USA. Using version 8.4.0.1 of the Surveillance, Epidemiology, and End Results (SEER)*Stat software, we calculated the standardized mortality ratios (SMRs) and 95% confidence intervals (CIs) for each cause of death.
Results: Out of the 3,165 deaths observed in the study population, the majority (2,245;70.9%) were attributed to AML itself, followed by non-AML cancers (573; 18.1%) and non-cancerous causes (347; 10.9%).
Conclusions: Patients with AML are at a higher risk of developing other types of cancer and granulocyte deficiencies, which increases the risk of death from non-cancerous causes such as infections. Moreover, treatment for AML carries the risk of cardiac problems. AML is commoner in males than females.
Keywords: Acute myeloid leukemia; Non-cancerous mortality cause; SEER database; Children; Standardized mortality ratios
| Introduction | ▴Top |
Acute myeloid leukemia (AML), also called acute nonlymphocytic leukemia, is a hematogenous malignancy caused by genetic and epigenetic mutations of myeloid stem cells leading to rapid proliferation and accumulation of undifferentiated myeloblasts in the bone marrow and, thus, impaired hematopoiesis [1, 2]. AML is grouped based on the World Health Organization (WHO) classification of hematolymphoid tumors into two main classes: AML with defining genetic abnormalities and AML defined by differentiation [3]. It is the most frequent type of leukemia in adulthood, and its incidence is directly proportional, and the prognosis is reversibly proportional with age. This correlation is due to prolonged exposure to mutations effects and carcinogens factors with aging [1, 2, 4]. Therefore, about 75% of AML cases in the USA are 65 years or older [1]. The median age at AML diagnosis is 68 [2]. According to the American Cancer Society statistics in 2020, estimated new cases and deaths of AML are 19,940 and 11,180, respectively [4]. AML counts 15-20% of leukemias in children and 33% in adolescents and young adults (AYA) [5]. Causes of death can be classified into three main groups: index-cancer, non-index-cancer, and non-cancer [6]. AML is an emergent oncologic case because there is a possibility of early death due to hematologic complications related to both leukemia itself and chemotherapy, such as infections, hemorrhage, and hyperleukocytosis. Infectious complications have a significant role in AML prognosis and mortality because of immune system dysfunction caused by the accumulation of immature immune cells and cytotoxic effects of chemotherapy that make patients more likely to be infected [7, 8]. Chemotherapy-related malnutrition is associated with hospital mortality in which 30% of AML patients in intensive care unit (ICU) are malnourished [9]. AML prognosis is better with younger age. More than half of patients younger than 40 will have overall survival (OS) for 5 years or more after diagnosis [10]. OS is also related to other conditions, making it different between patients. Subtypes of AML and their morphologic and cytogenic features are crucial factors that affect OS. In addition, sex and socioeconomic status are involved in OS variation. Acute promyelocytic leukemia (APL), inv(16), t(8;21), t(15;17), trisomy 21, younger age at diagnosis, female sex, and higher socioeconomic status are positive and hopeful factors [11]. Two studies demonstrated that prognosis of AML has improved over the past 30 years owing to modified chemotherapeutic and treatment strategies for new and relapsed AML, enhanced supportive care and prevention of patients from infections. This improvement obviously seems to be in children and AYA with 5-year survival of 60-75% in comparison with 56.3% during 2003 - 2010. However, children have better survival than AYA [4, 7]. Despite that, no adequate studies discuss the causes of death according to childhood and AYA age. Our sample specifically consisted of AML patients in the age groups of children and AYA due to the limited literature available for this specific age range. It is worth noting that older age groups often experience non-cancer causes of death at a higher rate, whereas the occurrence of such causes is relatively lower in younger age groups. Thus, discussing the increased percentage of non-cancer causes of death in this age range is an important gap that needs to be addressed. Additionally, conducting follow-up studies on these non-cancer causes in young patients can prove to be cost-effective. Therefore, we aimed to determine the non-cancer causes of death in children and AYA for contribution in decreasing mortality and improving survival as a better follow-up of patients.
| Materials and Methods | ▴Top |
Methods
In this retrospective cohort study, we used the most recent Surveillance, Epidemiology, and End Results (SEER)*Stat software 8.4.0.1 version to access SEER 17 plus data, Nov 2021 Sub (2000 - 2019) for standardized mortality ratio (SMR) (Fig. 1). Data were analyzed from February 2023 to March 2023. Since this study was based on anonymized data extracted from the publicly available SEER 17 registry of the National Cancer Institute (NCI), institutional review board approval was not required. This retrospective study followed the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” guidelines [12]. This study was conducted in accordance with the ethical guidelines outlined by the World Medical Association’s Declaration of Helsinki. Approval for all procedures was obtained from the Ethical Committee of Al-Azhar University Faculty of Medicine, Cairo, Egypt (2024/4).
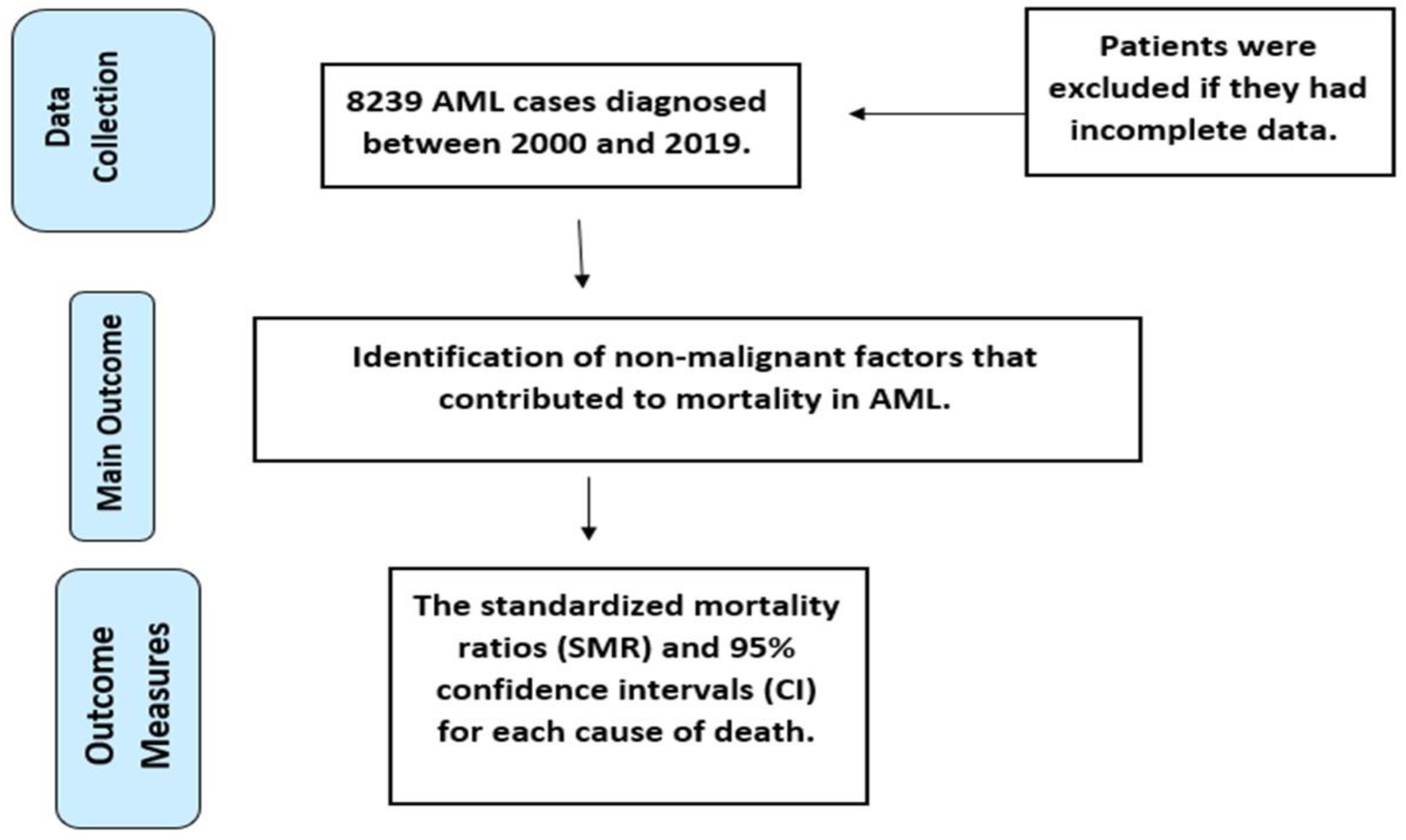 Click for large image | Figure 1. Flow chart of the study. |
Selection of the study cohort
Inclusion criteria
Using the SEER database, we included: 1) USA patients with histologically proven AML in our study: AML is typically diagnosed through the examination of bone marrow or blood samples, where the presence of immature cells, known as blasts, is observed. Histological analysis, involving the microscopic examination of tissue samples, is commonly used to confirm the diagnosis of AML. 2) From January 1, 2000, to December 31, 2019 (Connecticut, Iowa, New Mexico, Utah, Hawaii, metropolitan areas of Detroit, San Francisco-Oakland, Atlanta, and 13 counties of the Seattle-Puget Sound region, Los Angeles, San Jose-Monterey, the rest of the state of Georgia, and Alaska natives). 3) Patients with age between children 0 - 14 years and young adult 15 - 39 years for black or white male and female at the time of their AML diagnosis. 4) The site recode WHO International Classification of Diseases for Oncology, third edition variable to select AML. 5) The following morphology codes were employed to the results to be specific: 9840, 9861, 9865-9867, 9869, 9871-9874, 9895-9897, 9898, 9910-9911, and 9920 for AML. The codes are based on previous SEER-based studies.
Exclusion criteria
In SEER software, we selected only patients with specific criteria so the patient was excluded if he did not have a diagnosis that matches the specified ICD-O-3 morphology codes for AML. Additionally, we excluded patients who were diagnosed by death certificate/autopsy only or who had no reported survival time.
Outcomes
For included patients with AML, we analyzed non-cancer causes of death with concern for the following variables: age (children below 15 years old and young adults ranging from 15 years old to 40 years old), sex, and race, each according to latency periods (< 3 years, 3 - 5 years, and > 5 years following AML diagnosis). We defined the causes of death using the International Classification of Diseases 10th Revision (ICD-10)-WHO codes. Aleukemic refers to a state where there is a lack of abnormal white blood cells in the peripheral blood, even though leukemia is present. Sub-leukemic refers to a condition where the leukemic cells are present in the bone marrow but are not yet evident in the peripheral blood. Instances of septicemia and pneumonia were segregated from other infections as the SEER defined the causes of death using the ICD-10-WHO codes.
Statistical analysis
SEER*Stat is a statistical software which calculates raw data of cancer statistics. We calculated the SMRs with their 95% confidence intervals (CIs) for each cause of death using the SEER*Stat software version 8.4.0.1. All statistical tests that we performed were two-sided. A significantly increased risk is considered when the observed deaths from a particular cause after AML diagnosis were greater than the expected deaths from the same cause in the general population with a P value less than 0.05 (P < 0.05).
The SMR (O/E) ratio involves the comparison of the observed deaths (O) among patients diagnosed with AML over a defined period, against the expected deaths (E) in a demographic that shares age adjustments, over the same duration [13, 14]. So, the control group is the general population that share the same age, sex, race and died from the same cause of death over the same period of time.
| Results | ▴Top |
In this study, we analyzed data from 8,239 patients diagnosed with AML. The majority of these patients were between the ages of 15 and 39 (6,045; 73.3%), slightly more than half were male (4,201; 50.9%), and most were white (6,199; 75.2%). Over time, the number of AML cases showed a notable increase: 1,920 cases were recorded between 2000 and 2004, which rose to 2,169 cases between 2010 and 2014, before slightly declining to 2,103 cases between 2015 and 2019. Over the follow-up period, 3,165 patients (38.4%) died. Notably, most deaths occurred within the first 3 years after diagnosis (2,731; 86.2% of deaths). Death rates were decreasing with time, 238 (7.5%) patients between 3 and 5 years and 196 (6.1%) patients in more than 5 years. Details of the characteristics of the total study population and patients who died in each time interval are shown in Table 1.
 Click to view | Table 1. Characteristics of the AML Patients Included |
The primary cause of death was AML itself, accounting for 2,245 fatalities (70.9%). Non-AML cancers were the second leading cause, responsible for 573 deaths (18.1%), followed by non-cancer causes, which resulted in 347 deaths (10.9%). The mortality can be divided over time into three groups. In the first 3 years, there were 2,731 deaths, with 73.3% due to AML, 17.5% due to non-AML cancers, and 9.0% due to non-cancer causes. Between 3 and 5 years, 238 patients died, with 64.2% due to AML, 21.4% due to non-AML cancers, and 14.2% due to non-cancer causes. In the group of more than 5 years, 196 patients died, with 44.8% attributed to AML, 21.4% to non-AML cancers, and 33.6% to non-cancer causes.
The most common non-AML cancers were aleukemic or sub-leukemic conditions with 187 patients (32.6%) with SMR 3,352 (95% CI: 2,889.30 - 3,869.10) followed by lymphocytic leukemia with 45 patients (7.8%) with SMR 290.98 (95% CI: 212.24 - 389.35) followed by acute lymphocytic leukemia with 41 patients (7.1%) with SMR 291.41 (95% CI: 209.12 - 395.34) and chronic myeloid leukemia with 25 patients (4.3%) with SMR 913.11 (95% CI: 590.91 - 1,347.92). Other cancers were observed as well with increased SMR such as brain, breast, digestive system, and colon and rectum.
Non-cancer causes of death represented 10.9% of the total deaths (347 deaths). Other infectious and parasitic diseases including HIV represented the most dominant non-cancer cause of mortality (41; 11.8%) (SMR = 33.66; 95% CI: 24.16 - 45.67), followed by cardiovascular diseases with 31 deaths (8.9%) (SMR = 4.48; 95% CI: 3.05 - 6.36), septicemia with 16 deaths (4.6%) (SMR = 28.90; 95% CI 16.52 - 46.93), and pneumonia and influenza with 16 deaths (4.6%) (SMR = 25.98; 95% CI: 14.85 - 42.2). Table 2 shows the observed death events with the SMRs for each cause of mortality during the follow-up period and each time interval after diagnosis.
 Click to view | Table 2. SMRs for Each Cause of Death Following AML Diagnosis in All Patients |
When examining age-specific data, out of 706 deaths in children (up to 15 years), 71.3% were due to AML, 16.8% to non-AML cancers, and 11.7% to non-cancer causes. Among 2,459 deaths in young adults (15 - 39 years), 70.8% were due to AML, 18.4% to non-AML cancers, and 10.7% to non-cancer causes. Gender-specific data revealed higher mortality rates among males, with 1,682 deaths compared to 1,483 in females. For both genders, the leading cause of death was AML (69.6% in males and 72.2% in females). Non-AML cancers caused 20.2% of male deaths and 15.7% of female deaths, while non-cancer causes accounted for 10.0% of deaths in males and 12.0% in females. Overall, the study highlights that AML remains the predominant cause of death in these patients, particularly within the first 3 years following diagnosis.
| Discussion | ▴Top |
To our knowledge, this is the first large population-based study to investigate the causes of death in children and AYA patients with AML up to 40 years of age. AML, neoplastic proliferation of blast cells that are derived from myeloid marrow cells, progresses rapidly. Death occurs in approximately 2 months if left untreated, while 45% will survive the diagnosis for 5 years or more [10]. With a total of 8,239 AML patients included in this study, 3,165 (38.4%) patients died due to different causes classified into three main groups: index-cancer, non-index-cancer, and non-cancer. Our results showed that most AML patients died during the first 3 years following AML diagnosis (2,731; 86.2%), while as implied in our study, death rates gradually declined throughout the follow-up periods. Many factors play a significant role in prognosis and mortality [15-17]. Diagnosis of AML is frequently delayed, resulting in aggressive initial chemotherapy that contributes to elevated mortality rates because it may induce toxicity, which some patients may struggle to withstand. The risk of infections and bleeding is notably increased during this period. In addition, the greatest risk of relapse is observed within the initial years following diagnosis. Furthermore, AML displays a broad spectrum of genetic subtypes, with certain subtypes exhibiting more favorable responses to treatment. Responses to treatment and disease progression exhibit significant variability among patients, with some achieving remission and long-term survival, while others encounter obstacles. Xie et al conducted [11] a SEER-based study to evaluate the survival patterns in individuals diagnosed with AML at ages 0 - 24 years in the USA and England between 1995 and 2014. They reported that males, being diagnosed at ages 15 to 24, AML patterns, multiple primaries, and a higher degree of regional deprivation were associated with higher mortality risk. Mortality reduced in both countries over the years by about 20% during the study period. The risk of mortality among patients diagnosed at 15 - 24 years was 1.51 (95% CI: 1.35 - 1.69) times as high in the USA and 1.38 (1.18 - 1.62) times as high in England, compared to the hazard risk of mortality among children diagnosed at ages 0 - 9 years in the same country. The most deaths in our study population were attributed to AML itself in all follow-up periods (2,245; 70.9%). AML represents a critical oncologic scenario due to the hematologic complications stemming from both the leukemia itself and the administered chemotherapy resulting in the buildup of immature immune cells and therapy-related cytotoxic effects. These factors cause compromised immune system functionality, rendering patients more susceptible to infections. Furthermore, the presence of chemotherapy-induced malnutrition has been linked to increased hospital mortality [7, 8]. Non-AML cancers rank second (573; 18.1%), with aleukemic and sub-leukemic cancers being the most common causes (187; 32.6%). People with AML have an increased risk of developing other cancers. A SEER-based study conducted by Ghimire and Shah [18] showed that adult patients with AML are at a significantly higher risk of secondary primary malignancies (SPMs). Among 5,091 individuals, a total of 148 patients were diagnosed with 160 second primary malignancies, yielding an observed/expected (O/E) ratio of 1.17, with a 95% CI of 0.99 - 1.36, and an excess risk of 15.47 per 10,000 population. The study findings also included the median time-to-first SPM following the initial diagnosis of AML being 37.5 months. Furthermore, the researchers highlighted that the likelihood of specific SPMs is influenced by the patient’s age and the latency period. In 2014, a study [19] found that people younger than 60 years of age and who have AML are three times more likely to develop another cancer compared to similar people who do not have AML. They explained that as the treatment of AML becomes more successful, people with AML live longer, increasing the likelihood of developing a second cancer. Older research [20] conducted from 1970 to 1996 followed 501 patients with AML from when they were children, and it was found that these patients have 10 times increased risk of second cancers when compared with the general population. In the existing literature, there have been documented cases of AML progressing to CML. While the exact mechanism is not fully understood, some cases have been attributed to therapy-related factors [21]. Non-cancer conditions resulted in death in the rest patients (347; 10.9%). Other infectious and parasitic diseases, including HIV group has the highest proportion (41; 11.8%). Patients with AML have qualitative and quantitative granulocyte deficits predisposing them to bacterial and fungal infections with associated morbidity and mortality [22]. Chemotherapy regimens further drive granulocyte deficits and result in prolonged periods of severe neutropenia and disrupt mucosal barriers, further elevating infection risk. In addition to the previous group, 32 (9%) of deaths could be attributed to infection, including septicemia, pneumonia, and influenza.
Like many epidemiological studies based on the SEER program, this study encounters certain constraints. Many patient-related clinical parameters such as body mass, tobacco use, alcohol consumption, and medication regimens or therapy-related AML which could potentially elucidate mortality trends and associated etiologies, were not accessible within the SEER database. The identification of AML patients was conducted utilizing morphological coding within the SEER software, a methodology derived from prior SEER-based research endeavors. Furthermore, instances of septicemia and pneumonia were segregated from other infections due to the presence of distinct coding mechanisms.
Conclusion
AML is a neoplastic proliferation of blast cells, it progresses rapidly, and death occurs within 2 months if left untreated. Patients diagnosed with AML have an increased risk of developing other cancers. They also have granulocyte deficiencies leading to an increased risk of dying from non-cancerous causes such as infections. They also have an added risk of developing cardiac problems directly due to the treatment they receive for AML. AML is commoner in males than females.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
All authors do not have a potential conflict of interest.
Informed Consent
All data were collected from the SEER database, which is anonymized. The study’s execution did not need informed consent requirements.
Author Contributions
AE, KS, MAA, HAAI, EFG, AKA, RC, SD, AS, TE, IEA, AME, TMA, AMA, and AE designed the study and analyzed the data. HGD, AMO, ME, RE, AEH and DAG drafted the manuscript. All authors were involved in the critical analysis of the final version of the manuscript. All authors approved the manuscript as submitted and agree to be accountable for all aspects of the work.
Data Availability
The datasets generated and analyzed during the current study are available in the SEER*Stat Database: Incidence - SEER Research Plus Data, 17 Registries, Using SEER*Stat software 8.4.0.1 (http://www.seer.cancer.gov/seerstat/).
Abbreviations
AML: acute myeloid leukemia; AYA: adolescents and young adults; CI: confidence interval; ICD-10: International Classification of Diseases 10th Revision; ICU: intensive care unit; NCI: National Cancer Institute; OS: overall survival; SEER: Surveillance, Epidemiology, and End Results; SMRs: standardized mortality ratios; STROBE: Strengthening the Reporting of Observational Studies in Epidemiology; WHO: World Health Organization
| References | ▴Top |
- Shallis RM, Wang R, Davidoff A, Ma X, Zeidan AM. Epidemiology of acute myeloid leukemia: Recent progress and enduring challenges. Blood Rev. 2019;36:70-87.
doi pubmed - Zahran AM, Shibl A, Rayan A, Mohamed M, Osman AMM, Saad K, Mahmoud KH, et al. Increase in polymorphonuclear myeloid-derived suppressor cells and regulatory T-cells in children with B-cell acute lymphoblastic leukemia. Sci Rep. 2021;11(1):15039.
doi pubmed pmc - Khoury JD, Solary E, Abla O, Akkari Y, Alaggio R, Apperley JF, Bejar R, et al. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36(7):1703-1719.
doi pubmed pmc - Creutzig U, Kutny MA, Barr R, Schlenk RF, Ribeiro RC. Acute myelogenous leukemia in adolescents and young adults. Pediatr Blood Cancer. 2018;65(9):e27089.
doi pubmed pmc - Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30.
doi pubmed - Chen L, Zheng Y, Yu K, Chen S, Wang W, Gale RP, Liu ZX, et al. Changing causes of death in persons with haematological cancers 1975-2016. Leukemia. 2022;36(7):1850-1860.
doi pubmed pmc - Hahn A, Giri S, Yaghmour G, Martin MG. Early mortality in acute myeloid leukemia. Leuk Res. 2015;39(5):505-509.
doi pubmed - Torres-Flores J, Espinoza-Zamora R, Garcia-Mendez J, Cervera-Ceballos E, Sosa-Espinoza A, Zapata-Canto N. Treatment-related mortality from infectious complications in an acute leukemia clinic. J Hematol. 2020;9(4):123-131.
doi pubmed pmc - Van de Louw A, Zhu X, Frankenfield D. Obesity and malnutrition in critically ill patients with acute myeloid leukemia: Prevalence and impact on mortality. Nutrition. 2020;79-80:110956.
doi pubmed - Survival | Acute myeloid leukaemia | Cancer Research UK [Internet]. [cited May 25, 2023]. Available from: https://www.cancerresearchuk.org/about-cancer/acute-myeloid-leukaemia-aml/survival.
- Xie S, Hossain MJ. Survival differences in childhood and young adult acute myeloid leukemia: A cross-national study using US and England data. Cancer Epidemiol. 2018;54:19-24.
doi pubmed pmc - Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31-S34.
doi pubmed pmc - Elgenidy A, Afifi AM, Jalal PK. Survival and causes of death among patients with intrahepatic cholangiocarcinoma in the United States from 2000 to 2018. Cancer Epidemiol Biomarkers Prev. 2022;31(12):2169-2176.
doi pubmed - Yi M, Li A, Zhou L, Chu Q, Song Y, Wu K. The global burden and attributable risk factor analysis of acute myeloid leukemia in 195 countries and territories from 1990 to 2017: estimates based on the global burden of disease study 2017. J Hematol Oncol. 2020;13(1):72.
doi pubmed pmc - Sorror ML, Storer BE, Fathi AT, Gerds AT, Medeiros BC, Shami P, Brunner AM, et al. Development and validation of a novel acute myeloid leukemia-composite model to estimate risks of mortality. JAMA Oncol. 2017;3(12):1675-1682.
doi pubmed pmc - Newell LF, Cook RJ. Advances in acute myeloid leukemia. BMJ. 2021;375:n2026.
doi pubmed - Foster J, Blonquist TM, El-Jawahri A, Fathi AT, Amrein PC, Sadrzadeh H, et al. The end of life for patients with acute myeloid leukemia (AML)- a single center experience. Blood [Internet]. 2015;126(23):3318.
doi - Ghimire KB, Shah BK. Second primary malignancies in adult acute myeloid leukemia—A US population-based study. Anticancer Res. 2014;34(7):3855-3859.
pubmed - Shah BK, Ghimire KB. Second primary malignancies in chronic myeloid leukemia. Indian J Hematol Blood Transfus. 2014;30(4):236-240.
doi pubmed pmc - Baker KS, DeFor TE, Burns LJ, Ramsay NK, Neglia JP, Robison LL. New malignancies after blood or marrow stem-cell transplantation in children and adults: incidence and risk factors. J Clin Oncol. 2003;21(7):1352-1358.
doi pubmed - Cheng J, Liao Y, Bin T, J OU, Chen S, Chen X, Zou W. Secondary chronic myeloid leukemia following acute myeloid leukemia treated with autologous hematopoietic stem cell transplantation: a case report. Curr Med Res Opin. 2020;36(11):1807-1812.
doi pubmed - Taveras Alam S, Lopez E, Dongarwar D, Pandey R, Torrejon Guzman N, Tarallo MC. Acute myeloid leukemia place of death: change over two decades. Blood. 2022;140(Supplement 1):11011-11012.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


