| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Case Report
Volume 15, Number 7, July 2023, pages 384-389
Histopathological Findings of Ectopic Pregnancy in Contraceptive-Wearing Woman
Takuma Hayashia, b, c, f , Kenji Sanob, c, d, Ikuo Konishia, b, c, e
aDepartment of Cancer Medicine, National Hospital Organization Kyoto Medical Centre, Kyoto, Japan
bFirst-Track Medical R&D, The Japan Agency for Medical Research and Development (AMED), Tokyo, Japan
cClinical Research, PRUM-iBio Study Group, National Hospital Organization Tokyo Headquarter, Tokyo, Japan
dDepartment of Clinical Laboratory, Shinshu University Hospital, Nagano, Japan
eDepartment of Obstetrics and Gynecology, Kyoto University Graduate School of Medicine, Kyoto, Japan
fCorresponding Author: Takuma Hayashi, National Hospital Organization Kyoto Medical Centre, Mukaihatake-cho, Fushimi-ku, Kyoto Kyoto, Japan
Manuscript submitted April 25, 2023, accepted June 22, 2023, published online July 12, 2023
Short title: Pathological Findings of Ectopic Pregnancy
doi: https://doi.org/10.14740/jocmr4924
| Abstract | ▴Top |
In normal pregnancy, the egg is fertilized in the fallopian tube. It later moves into the uterus, where it implants into the uterine endometrium. Therefore, implantation of the fertilized egg into the endometrium is not observed in many women using contraceptives. However, if the fallopian tubes are diseased or abnormal, the fertilized egg cannot travel to the endometrium. Thus, the fertilized egg is implanted in tissues other than the uterus, resulting in an ectopic pregnancy. In most cases of ectopic pregnancy, the fertilized egg is implanted into the left or right fallopian tube or in tissues other than the fallopian tubes such as the ovary. With laparoscopic surgery, the scars are small, and the pain and physical burden are also much lesser than those with open surgery; thus, the patient can be rehabilitated immediately. Laparoscopic surgery is preferred for the termination of ectopic pregnancies because the patients recovered quickly physically after surgery and can be discharged in a short period. This paper presents our experience in treating a 37-year-old woman who had a tubal pregnancy despite using a contraceptive. Contrast-enhanced magnetic resonance imaging showed a gestational sac within the right fallopian tube. Laparoscopic surgery was performed to resect the right fallopian tube. Pathological examination suggested that the ectopic pregnancy occurred at the organogenesis stage 9 weeks after fertilization. The pathological findings revealed subpopulations of cells from the ectoderm that were separated from other cells and more specifically formed spinal and ovarian structures. The implantation of the fertilized egg into the endometrium is not observed in many women using contraceptives. However, in rare cases, ectopic pregnancy occurs in women using contraceptives; thus, caution is necessary in diagnosis and treatment. This report presents valuable surgical pathological findings from such a rare case of ectopic pregnancy to understand the differentiation into each tissue during organogenesis.
Keywords: Ectopic pregnancy; hCG; Histopathological finding; Contraceptive; Fallopian tube
| Introduction | ▴Top |
Ectopic pregnancy refers to the implantation of a fertilized egg in tissues other than the endometrium. It is classified into four types depending on the implantation site of the fertilized egg: fallopian tube pregnancy, interstitial pregnancy, cervical pregnancy, and ovarian pregnancy. Among them, fallopian tube pregnancy is the most common, accounting for more than 95% of all ectopic pregnancy cases [1]. Of fallopian tubal pregnancies, the ampulla is the most common site of implantation (80%), followed by the isthmus (12%), fimbria (5%), cornua (2%), and others (1%) [2]. Studies have shown that ectopic pregnancies occur in approximately 0.5-2% of all pregnancies [3]. In particular, women who have pelvic organ inflammation, abdominal surgery, or a history of ectopic pregnancy have increased risk of ectopic pregnancy [4]. In recent years, the incidence of ectopic pregnancy has been increasing, given the increase in the number of women suffering from sexually transmitted diseases such as chlamydia and those undergoing infertility treatments (in vitro fertilization/embryo transfer) [5].
Fallopian tube pregnancy is frequently associated with pelvic inflammatory disease, which may lead to fallopian tube stenosis. This condition prevents the fertilized egg from moving toward the uterus, causing it to attach to the tube itself. The symptoms of fallopian tube pregnancy include abdominal pain and vaginal bleeding. The first diagnostic step is to confirm the pregnancy with human chorionic gonadotropin (hCG) testing; next, transvaginal ultrasound is performed to determine the location of the pregnancy and fetal heartbeat [6, 7] (Supplementary Material 1, www.jocmr.org) [8]. Uncomplicated ectopic pregnancies often resolve spontaneously and are usually difficult to diagnose. Since an ectopic pregnancy presents with symptoms similar to those of a normal pregnancy, such as morning sickness, abdominal pain, and abnormal vaginal bleeding, there are no subjective symptoms suggestive of an ectopic pregnancy. In addition, many women are unaware that they are pregnant and misidentify abnormal vaginal bleeding as menstruation. Women who have irregular menstruation or irregular vaginal bleeding on a regular basis may have hidden diseases other than ectopic pregnancy. Laparoscopy or laparotomy can also be performed to visually confirm an ectopic pregnancy. These procedures are generally performed for women presenting signs of an acute abdomen and hypovolemic shock.
Patients with unruptured ectopic pregnancy are typically hemodynamically stable with low, declining β-hCG concentrations (< 3,000 IU/L) [6] (Supplementary Material 1, www.jocmr.org) [8]. Fetuses from ectopic pregnancies may survive for several weeks. Exceptionally, there are recorded cases of ectopic pregnancies (abdominal pregnancy) with live birth. However, in many cases, they will eventually die because no tissue outside the uterus can provide their blood supply. In many cases, the structures containing the fetus rupture after about 6 to 16 weeks, long before the fetus can survive, however, unruptured ampullary ectopic pregnancy at 16-week period of gestation with live fetus [7]. Complicated cases may involve tubal abortion or rupture, which can lead to intra-abdominal bleeding and shock. Tissue rupture in an ectopic pregnancy can cause severe bleeding and can be life-threatening to the mother. The later the rupture, the greater the blood loss and the higher the risk of death. However, if the ectopic pregnancy is treated before it ruptures, the risk of death is decreased. Although uncomplicated cases are treated conservatively (e.g., methotrexate or expectant management), complicated cases require surgical removal. In cases of abdominal pain in women of reproductive age, ruptured ectopic pregnancy should be ruled out.
Properly used contraceptives mostly prevent pregnancy by suppressing ovulation rather than preventing normal pregnancy implantation. However, ectopic pregnancy should be suspected in women using contraceptives, showing signs of pregnancy, such as elevated hCG levels, as seen in this case. Accurate diagnosis and treatment are very important in such cases. This study showcases valuable surgical histopathological findings from cases of ectopic pregnancy for understanding the differentiation into each tissue during the stage of organogenesis.
This study involves human participants and was approved by an Ethics Committee(s) and Institutional Board(s). The experiments with human tumor tissues derived from patients with high-grade serous ovarian cancer were conducted at Shinshu University and National Hospital Organization Kyoto Medical Center in accordance with institutional guidelines (i.e., IRB approval no. M192, H31-cancer-2) [9].
| Case Report | ▴Top |
Investigations
In July 2022, a 37-year-old woman had an intrauterine device (IUD; FD-1, Fuji Latex Ltd., Tochigi, Japan) inserted in her uterus. She experienced menstruation in September 2022 and no menstruation for 7 weeks thereafter. In November 2022, she visited a nearby obstetrics and gynecology clinic. Clinical presentation of ectopic pregnancy occurs at a mean of 7.2 weeks after the last normal menstrual period, with a range of 4 to 8 weeks [10]. Later presentations are more common in communities deprived of modern diagnostic ability. At that time, her urine hCG concentration was used, and it was thought that she might be pregnant. However, ectopic pregnancy was suspected because ultrasound imaging did not reveal a GS in the uterus. She did not experience intra-abdominal bleeding. Ectopic pregnancy should be suspected if the hCG level is ≥ 2,000 IU/L and no GS is observed in the uterus (Supplementary Material 1, www.jocmr.org) [11, 12].
Methods
Blood test
To check the patient’s pregnancy status and physical condition, hCG, blood glucose level, serum ferritin level, irregular antibodies (index marker for pregnancy status and pregnancy maintenance), presence or absence of various infectious diseases (human immunodeficiency virus 1/2 (HIV 1/2) antigen, hepatitis B type virus (HBV) antigen, hepatitis C type virus (HCV) antibody, treponema pallidum (TP) antibody, etc.) were measured, using blood collected from patients at the clinical laboratory department of general medical institutions.
Magnetic resonance imaging (MRI) examination
To determine the patient’s pregnancy status and the location of the gestational sac (GS), a contrast-enhanced MRI examination was performed (Vantage Centurian: Vantage Galan 3T MRT-3020, Canon Medical Systems, Inc., Ohtawara, Tochigi, Japan). According to the rules of Japanese general medical institutions, non-contrast MRI examinations for pregnant women are always performed in one stage, and after image evaluation, contrast-enhanced MRI examinations are performed only when it is determined that contrast-enhanced examinations are unavoidable for diagnosis.
Laparoscopic surgery
To resect the left fallopian tube where GS was noted, laparoscopic surgery was performed for the patient with the ectopic pregnancy (ENDOEYE FLEX 3D, Olympus Corporation, Shinjuku, Tokyo, Japan).
Results
Blood testing of serum α-hCG levels and other indices
Changes in serum hCG over 48 h can be used to define the hCG ratio, which is calculated as follows: hCG ratio = hCG at 48 h/hCG at 0 h [13]. An hCG ratio of 0.87 (i.e., a 13% decrease in hCG over 48 h) has 93% sensitivity and 97% specificity for predicting a failing pregnancy of unknown location [13]. Unfortunately, there is no single method to characterize the pattern of serum hCG change over 48 h in women classified with a pregnancy of unknown location who are subsequently diagnosed with an ectopic pregnancy [13]. When the patient first came to our general hospital, her blood test results showed a serum hCG level of 9,316. Forty-eight hours later, her serum hCG level was 3,773. Her hCG ratio after 48 h was 0.405 (a 59.5% reduction in serum hCG).
Her blood sugar level, serum iron level, and irregular antibodies were 106 mg/dL, 46 g/dL, and negative, respectively. She was tested for HIV 1/2, HBV, HCV, and TP to confirm the presence or absence of viral infections. Her results were as follows: HIV 1/2 (0.05 S/CO), HBV (HB antigen quantitative: < 0.02 IU/mL), HCV (HCV antibody: 0.1 S/CO), and TP qualitative antibody level (0.08 S/CO). However, in vivo inflammation was indicated because her C-reactive protein was high (0.29 mg/dL).
Findings from MRI examination
Plain pelvic MRI and contrast-enhanced MRI were performed as the patient did not wish to continue her pregnancy. Ectopic pregnancy was suspected because MRI showed a cystic lesion with ring-shaped diffusion restriction and contrast enhancement in the right fallopian tube (Fig. 1a, b). No structures suggestive of a GS were observed in the cavity of the uterus. Mild endometrial thickening was observed. A small amount of intraperitoneal fluid was noted, but bloody ascites was negative, in other words, no intra-abdominal bleeding is observed. Contrast-enhanced MRI study revealed that the bilateral ovaries were not normal. The IUD was located in the isthmus of the uterus (Supplementary Material 2, www.jocmr.org). Scarring from the previous cesarean section was noted. Pregnancy in the right fallopian tube was suspected due to various findings on MRI examination (Fig. 1a, b; Supplementary Material 2, www.jocmr.org). A cyst was observed on the dorsal side of the left ovary, suggesting the development of an ovarian or paraovarian cyst, a lesion resembling a cyst was noted in the right ovary (Supplementary Material 2, www.jocmr.org).
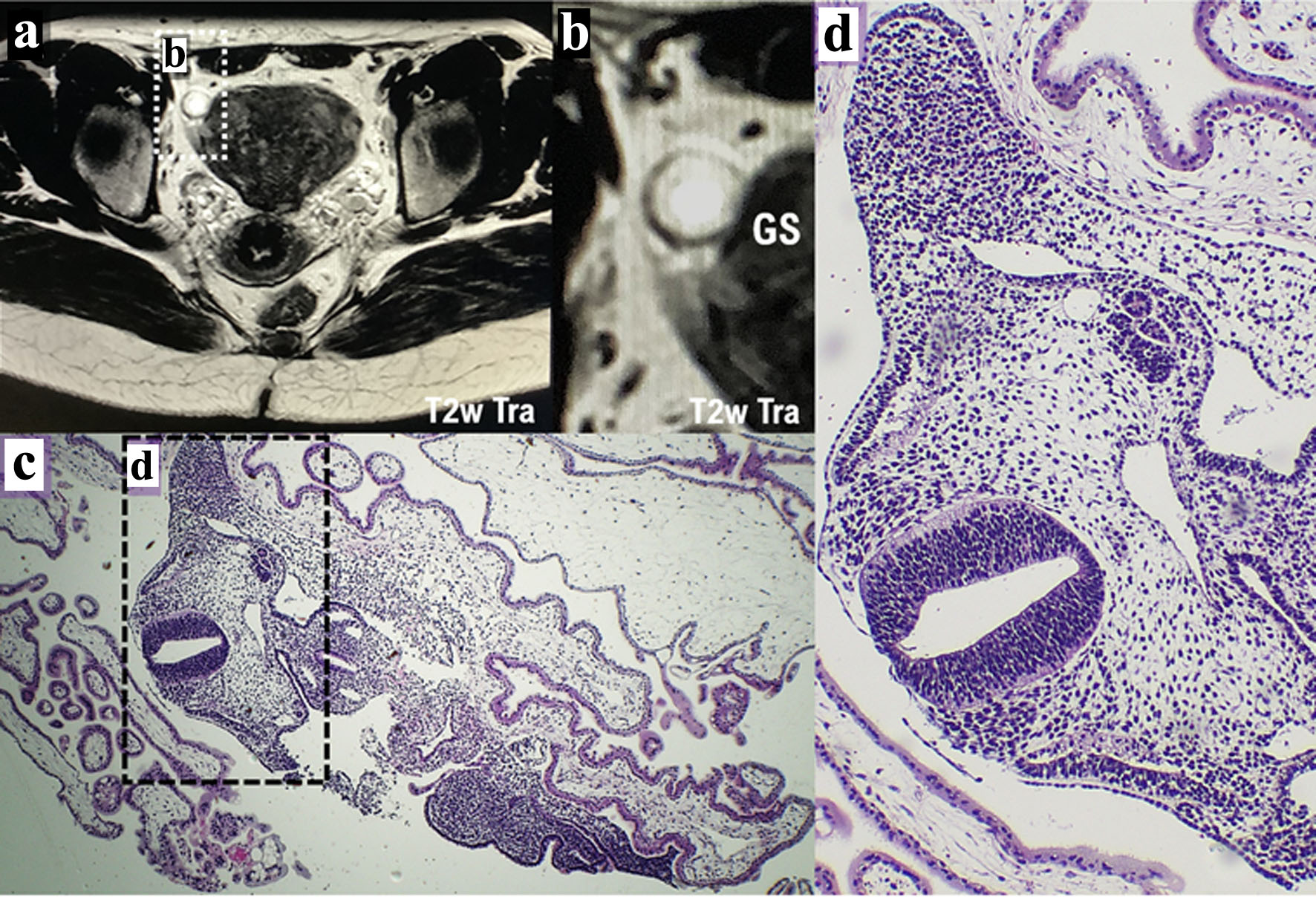 Click for large image | Figure 1. Diagnosis of ectopic pregnancy by contrast-enhanced MRI and histopathological examination. (a) The result described from contrast-enhanced MRI examination (T2w Tra) shows the possibility of ectopic pregnancy. The white dotted area shown in a is presented as panel b. (b) The GS in the right fallopian tube is indicated by a white spherical structure. Ectopic pregnancy was suspected because MRI showed a cystic lesion with ring-shaped diffusion restriction and contrast enhancement in the right fallopian tube. (c) A specimen of the resected right fallopian tube was used for pathological diagnosis. The black dotted area shown in panel c is presented as panel d. (d) Histopathological examination reveals the histology of the developing fetus during the growth period. GS: gestational sac; MRI: magnetic resonance imaging. |
Tissue findings
Villi, trophoblasts, and embryos were observed in the fallopian tubes. Nucleated erythrocytes were observed in the blood vessels of the villi. Ectopic pregnancy was confirmed based on these tissue findings. Fetal malformations or malignancies were not suspected.
Findings by pathological diagnosis
A specimen of the resected right fallopian tube was used for pathological diagnosis (Figs. 1c, d, 2, Supplementary Material 3, www.jocmr.org). Villus-like structures and hemorrhages were observed. Based on the pathological examination findings, ectopic pregnancy occurred during the organogenesis period around the ninth week after fertilization (Figs. 1c, d, 2). There is no difference in the structure of the reproductive tract between males and females during the early stages of development. The Wolffian and Mullerian tubes are formed early in development (Supplementary Material 1, www.jocmr.org) [14, 15]. In females, the left and right Mullerian ducts fuse to form the uterus and the upper part of the vagina as the fetus develops. The unfused tissue becomes the fallopian tube, and the Wolffian ducts degenerate. If union is incomplete, the structure of the uterus and vagina will be malformed. On the other hand, in males, the Mullerian ducts degenerate, and Wolffian ducts develop into the vas deferens. The initial stage of oviduct formation in the upper part of the Mullerian duct outside the left and right genital ridges is recognized. The Mullerian ducts appear to atrophy. This fetus is most likely a girl (Fig. 2).
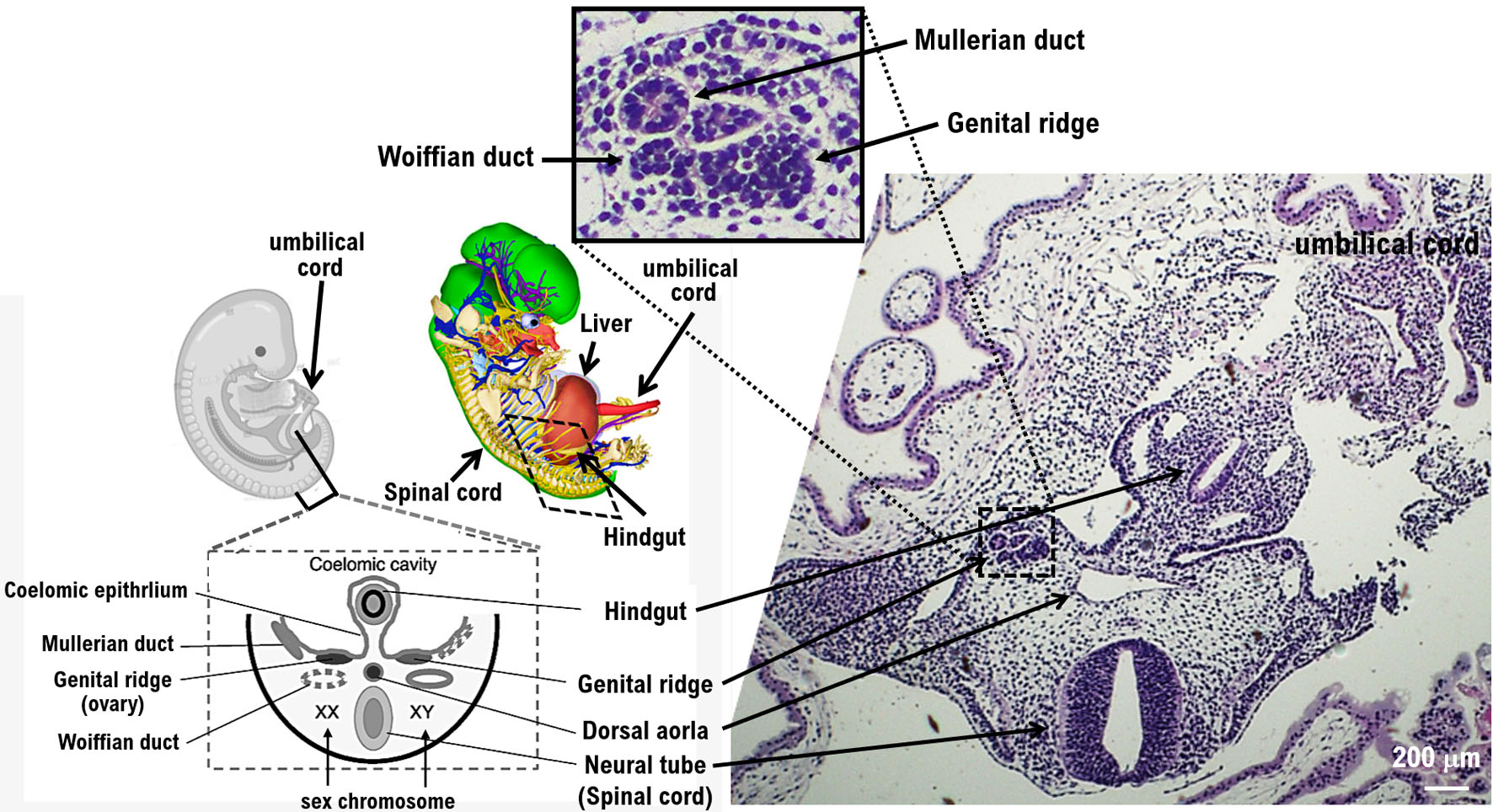 Click for large image | Figure 2. Structure of various tissues of the growing fetus via histopathological examination. Histopathological examination reveals the structure of various tissues of the growing fetus after the ninth week of pregnancy. The images show the development of the neural tube (spinal cord), hindgut, and dorsal aorta. Pathological examination shows the development of the genital ridge. The genital ridge (or gonadal ridge) is the precursor to the gonads. Initially, the genital ridge consists mainly of mesenchyme and cells of underlying mesonephric origin. Once oogonia enter this area, they attempt to associate with these somatic cells. Pathological results suggest that the fetus may be female. |
The pathological examination showed the development of the genital ridge (Figs. 1c, d, 2, Supplementary Material 3, www.jocmr.org). The genital ridge (or gonadal ridge) is the precursor to the gonads. Initially, the genital ridge consists mainly of mesenchyme and cells of underlying mesonephric origin. Once oogonia enter this area, they attempt to associate with these somatic cells. The pathological results suggested that the fetus may be female. Development proceeds, and the oogonia become fully surrounded by a layer of cells (pre-granulosa cells). That is, the genital ridge is formed from the mesenchyme and coelomic epithelium at about 4 weeks of gestation and will ultimately provide somatic cells to the follicle (Figs. 1c, d, 2, Supplementary Material 3, www.jocmr.org).
| Discussion | ▴Top |
An ectopic pregnancy is when the fertilized egg implants somewhere other than the endometrium. Fallopian tubal pregnancies are the most common and account for approximately 95% of ectopic pregnancies [1]. The risk factors for ectopic pregnancy are thought to include pelvic inflammation and fertility treatments. The case we report here is the development of an unruptured fallopian tubal pregnancy in a woman using a contraceptive. In a fallopian tubal pregnancy, a tubal abortion or tubal rupture may occur, and the patient may die from shock due to excessive bleeding. Therefore, early diagnosis and treatment of fallopian tubal pregnancy are important. If the fallopian tube pregnancy is small and unruptured, drug therapy may be considered in addition to surgical treatment. Administration of methotrexate (MTX) (Supplementary Material 1, www.jocmr.org) [16], a kind of anticancer drug, is considered [17]. In many cases, surgical treatment is performed to remove the fetus and a portion of the affected organs from the implantation site. In addition, surgical treatment is performed in cases where MTX treatment is ineffective. Combination therapy with gefitinib, an epidermal growth factor receptor tyrosine kinase inhibitor, and MTX was suggested to be more effective than MTX alone. However, a recent clinical trial did not show the greater efficacy of combination therapy than MTX alone [18]. In addition, higher incidences of diarrhea and rash were observed with combination therapy than MTX alone [18].
Conclusion
The implantation of the fertilized egg into the endometrium is not observed in many women using contraceptives. However, in rare cases, ectopic pregnancy occurs in women using contraceptives; thus, caution is necessary in diagnosis and treatment. Laparoscopic surgery is performed as surgical treatment for many ectopic pregnancies worldwide. Recently, laparoscopic surgery has also been safely performed for ectopic pregnancies at rare sites. Emergency surgery has also been performed quickly and safely for cases of ectopic pregnancy with massive bleeding. Laparoscopic surgery is considered to be useful even for patients with unstable hemodynamics if there is sufficient cooperation with a general managing physician and the medical system of the facility is well established.
| Supplementary Material | ▴Top |
Suppl 1. Measurement of serum hCG concentration. Transvaginal ultrasound imaging. Wolffian and Mullerian ducts. Methotrexate.
Suppl 2. Clinical findings described by contrast-enhanced MRI imaging examinations.
Suppl 3. Clinical findings described by histopathological imaging examinations.
Acknowledgments
We thank all medical staff for clinical research at Kyoto University Hospital and the National Hospital Organization Kyoto Medical Center.
Financial Disclosure
This clinical research was performed with research funding from the following: Japan Society for Promoting Science for TH (Grant No. 19K09840), START-program Japan Science and Technology Agency for TH (Grant No. STSC20001), and the National Hospital Organization Multicenter clinical study for TH (Grant No. 2019-Cancer in general-02), and The Japan Agency for Medical Research and Development (AMED) (Grant No. 22ym0126802j0001), Tokyo, Japan.
Conflict of Interest
The authors state no competing interest.
Informed Consent
We have obtained informed consent from people participating in clinical studies.
Author Contributions
All authors had full access to the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Conceptualization: TH and IK. Writing-original draft: TH and IK. Writing-review and editing: IK. Visualization: TH and IK. Supervision: TH and IK. Funding acquisition: TH and IK.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Serin AN, Birge O. Non-tubal ectopic pregnancy: incidence and diagnosis. Non-tubal ectopic pregnancy. Edited by Julio Elito Jr. https://www.intechopen.com/chapters/69498.
- Sepilian VP, Wood E. Ectopic pregnancy. Section of Drugs & Diseases > Obstetrics & Gynecology. Medscape. 2022. https://emedicine.medscape.com/article/2041923-overview.
- Committee on Practice Bulletins-Gynecology. ACOG Practice Bulletin No. 191: tubal ectopic pregnancy. Obstet Gynecol. 2018;131(2):e65-e77.
doi pubmed - Hocking JS, Geisler WM, Kong FYS. Update on the epidemiology, screening, and management of chlamydia trachomatis infection. Infect Dis Clin North Am. 2023;37(2):267-288.
doi pubmed - Patil M. Ectopic pregnancy after infertility treatment. J Hum Reprod Sci. 2012;5(2):154-165.
doi pubmed pmc - Webster K, Eadon H, Fishburn S, Kumar G, Guideline C. Ectopic pregnancy and miscarriage: diagnosis and initial management: summary of updated NICE guidance. BMJ. 2019;367:l6283.
doi pubmed - Mhaskar R, Harish M, Jaiprakash T. Unruptured ampullary ectopic pregnancy at 16-week period of gestation with live fetus. J Obstet Gynaecol India. 2014;64(1):73-74.
doi pubmed pmc - Soundravally R, Krishna Latha T, Soundara Raghavan S, Ananthanarayanan PH, Srilatha K. Diagnostic significance of total creatine kinase and its isoform in tubal ectopic pregnancy. J Obstet Gynaecol Res. 2013;39(12):1587-1591.
doi pubmed - Hayashi T, Konishi I. Molecular histopathology for establishing diagnostic method and clinical therapy for ovarian carcinoma. J Clin Med Res. 2023;15(2):68-75.
doi pubmed pmc - Cecchino GN, Araujo Junior E, Elito Junior J. Methotrexate for ectopic pregnancy: when and how. Arch Gynecol Obstet. 2014;290(3):417-423.
doi pubmed - Dubbewar A, Srivastava A, Hiremath RN, Ghodke S, Chourey N, Sreenivas A. A rare case of spontaneous heterotopic pregnancy with intrauterine gestational trophoblastic neoplasia and tubal ectopic pregnancy at a remote secondary care hospital. J Family Med Prim Care. 2022;11(7):3996-3998.
doi pubmed pmc - Peker N, Aydeniz EG, Gundogan S, Sendag F. Laparoscopic management of heterotopic istmocornual pregnancy: a different technique. J Minim Invasive Gynecol. 2017;24(1):8-9.
doi pubmed - Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update. 2014;20(2):250-261.
doi pubmed - Hashimoto R. Development of the human Mullerian duct in the sexually undifferentiated stage. Anat Rec A Discov Mol Cell Evol Biol. 2003;272(2):514-519.
doi pubmed - Wrobel KH. The genus Acipenser as a model for vertebrate urogenital development: the mullerian duct. Anat Embryol (Berl). 2003;206(4):255-271.
doi pubmed - Neycheva S, Naseva E, Batalov Z, Karalilova R, Batalov A. Adherence to biological therapies in patients with rheumatoid arthritis: a retrospective cohort study. Rheumatol Int. 2023;43(7):1287-1296.
doi pubmed - Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72(9):1707-1714.
pubmed - Horne AW, Tong S, Moakes CA, Middleton LJ, Duncan WC, Mol BW, Whitaker LHR, et al. Combination of gefitinib and methotrexate to treat tubal ectopic pregnancy (GEM3): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2023;401(10377):655-663.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


