| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Case Report
Volume 16, Number 5, May 2024, pages 264-271
Recurring ST-Elevation Myocardial Infarction With No-Reflow Caused by Hypercoagulable State: A Behcet Disease Case Report
Ahmed Hegazi Abdelsamiea, b , Nayef Al-Asiria
aCardiac Center, Mouwasat Hospital Al-Jubail Industrial City, Jubail, Saudi Arabia
bCorresponding Author: Ahmed Hegazi Abdelsamie, Cardiac Center, Mouwasat Hospital Al-Jubail Industrial City, Jubail, Saudi Arabia
Manuscript submitted February 16, 2024, accepted April 25, 2024, published online May 29, 2024
Short title: Recurring STEMI With No-Reflow in a BD Case
doi: https://doi.org/10.14740/jocmr5132
| Abstract | ▴Top |
Acute myocardial infarction (AMI) in young patients is an important issue because of its impact on health and social life. The mechanisms and disease courses of ST-elevation myocardial infarction (STEMI) in young individuals may differ from those in the elderly. Behcet disease (BD) is a multisystem autoimmune disorder of unknown etiology. Cardiac involvement is rare, yet it was reported to affect 6% of patients, with 17% of the cases presenting as the first manifestation. We present the case of a 33-year-old male heavy smoker with negative medical history, who presented with acute inferior myocardial infarction. His coronary angiography showed huge thrombosis in proximal right coronary artery. He was treated with primary coronary intervention and implantation of drug-eluting stent, with subsequent intervention and implantation of two more drug-eluting stents due to acute stent thrombosis within 48 h. Rheumatologic assessment revealed the history of four different attacks of oral ulcers and one attack of genital ulcer. His workup showed positive human leukocyte antigen (HLA) allele (B51) which is strongly associated with BD. AMI in young adults due to arterial thrombosis can be attributed to hypercoagulable state related to early manifestation of BD. Increased knowledge of AMI in young adults and its presentation in BD is necessary to reduce morbidity and mortality. Corticosteroids and colchicine may improve cardiac manifestations in BD.
Keywords: Acute myocardial infarction; ST-elevation myocardial infarction; Pericarditis; Behcet disease
| Introduction | ▴Top |
Acute myocardial infarction (AMI) in young patients is an important issue because of its impact on health and social life [1]. The mechanisms of ST-elevation myocardial infarction (STEMI) in young individuals may have a different course from those in the elderly. Cigarette smoking is considered one of the strongest risk factors associated with coronary artery disease (CAD) in young adults. Moreover, a family history of premature CAD is frequently encountered as an important risk factor in youth [2]. This could be attributed to genetic disorders related to lipid metabolism and coagulation pathways [3]. Behcet disease (BD) is a multisystem vasculitis of unknown etiology characterized by mucocutaneous, ocular, arthritic, and vascular manifestations. It was reported that 1-6% of BD patients suffer from cardiac involvement. Another study reported that cardiac manifestations were the first feature in 32.7% of their patients [4].
The cardiac abnormalities include pericarditis, myocarditis, endocarditis with valvular regurgitation, intracardiac thrombosis, coronary arteritis with or without myocardial infarction, and aneurysms of the coronary arteries or sinus of Valsalva. Data regarding the clinical spectrum, prevalence, and outcome of cardiac lesions in BD are lacking [4].
| Case Report | ▴Top |
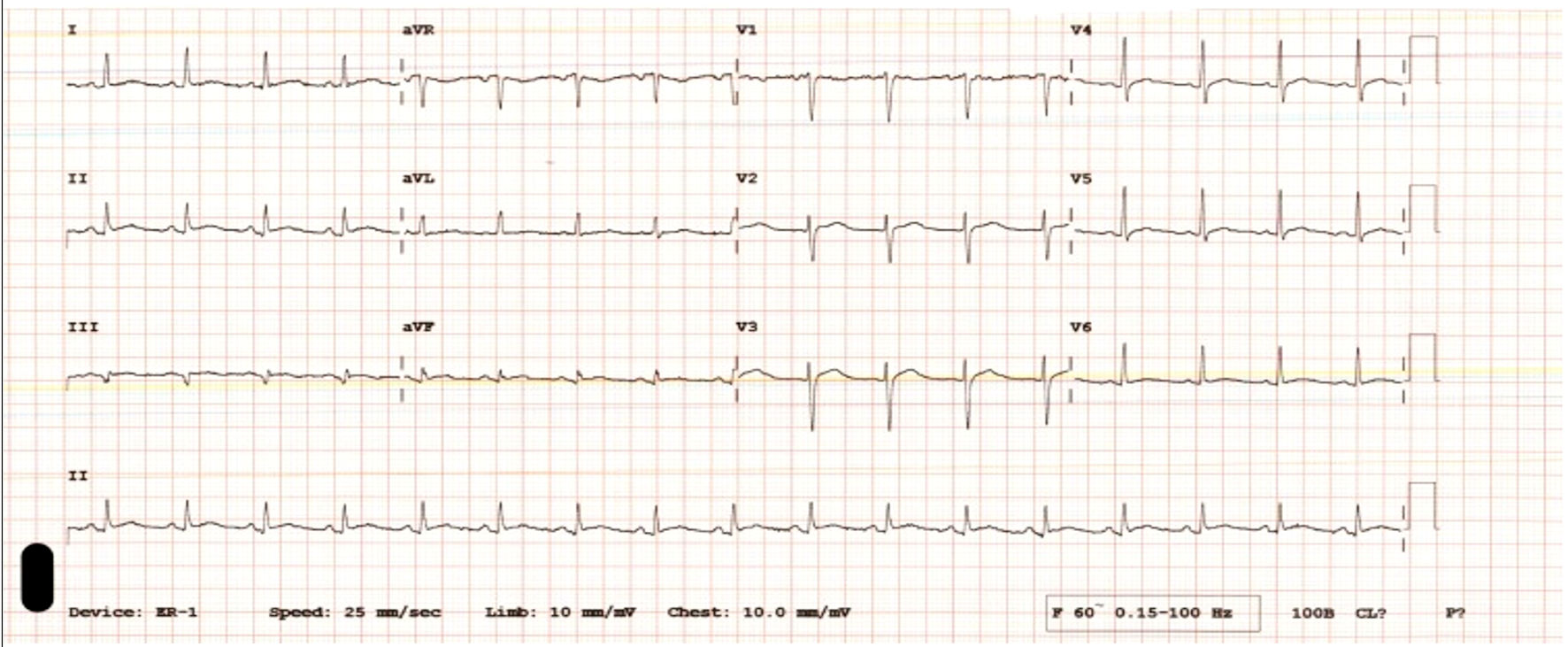
A 33-year-old male heavy smoker, with no significant medical history, suffered sudden onset progressive chest pain associated with nausea and sweating and was brought to the Emergency Room 1 h later. His daughter was recently diagnosed with Kawasaki disease. On physical examination, his vital signs were as follows: pulse 86 beats per minute, blood pressure 113/74 mm Hg, and oxygen saturation was 98% on room air. Immediate electrocardiogram (ECG) revealed normal sinus rhythm with ST segment elevation in leads II, III and aVF with reciprocal changes in leads I and aVL (Fig. 1).
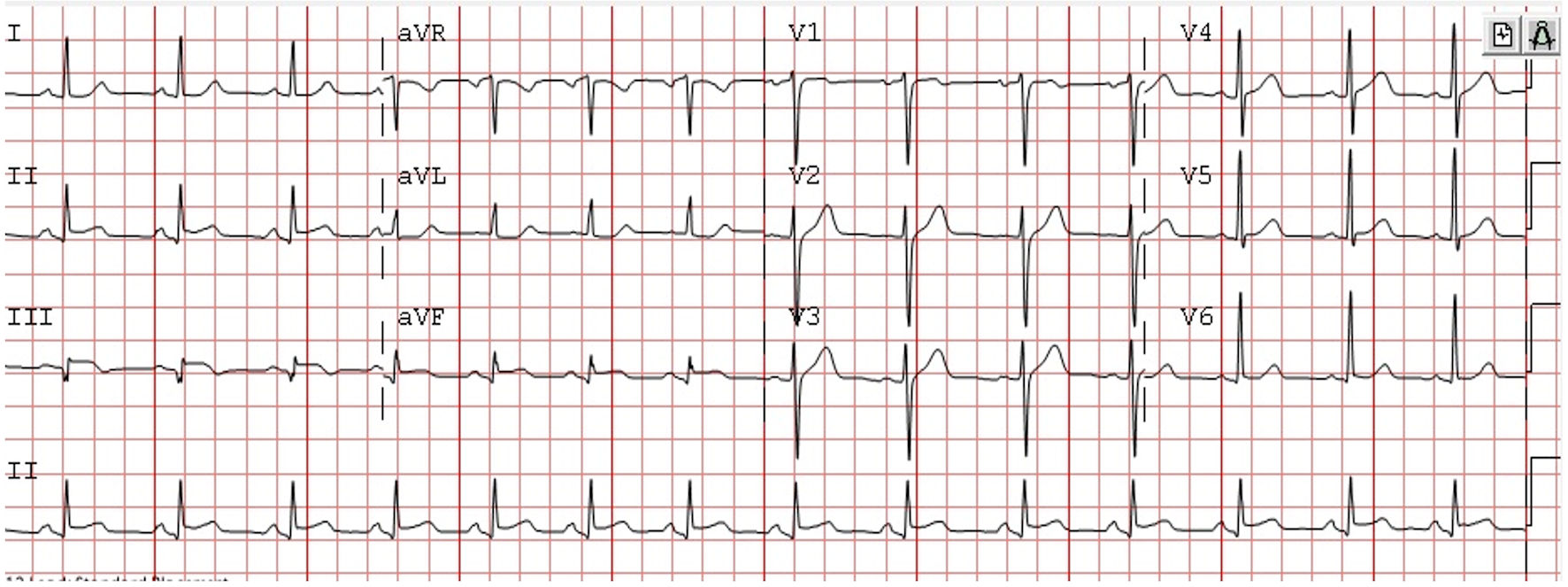 Click for large image | Figure 1. Electrocardiogram on admission demonstrating inferior ST elevation myocardial infarction. |
The loading doses of oral aspirin 300 mg, ticagrelor 180 mg and intravenous (IV) heparin 8,000 IU were administrated, and the patient was transferred to catheterization lab for percutaneous coronary intervention (PCI).
Coronary angiography (CAG) was done through right radial artery access (Fig. 2a, b). It showed the average size of the left main coronary artery with no significant lesion. The left anterior descending artery was type III, ectatic in its proximal part, associated with slow flow, but no significant lesion. The left circumflex artery was dominant, giving obtuse marginal branch which showed mild ostio-proximal ectasia and slow flow, but no significant lesion was observed. The right coronary artery (RCA) was non-dominant, mildly ectatic from proximal segment followed by total occlusion with huge thrombus burden. IV tirofiban bolus dose was given, then maintenance infusion was initiated. Aspiration of the thrombus using Merit device 6 French was performed followed by implantation of 3.5 × 23 mm XIENCE Skypoint drug-eluting stent. Post dilatation using non-compliant balloons of 4.0 × 12 mm and 4.5 × 10 mm was performed with excellent final results of Thrombolysis In Myocardial Infarction (TIMI) III flow (Fig. 2c, d).
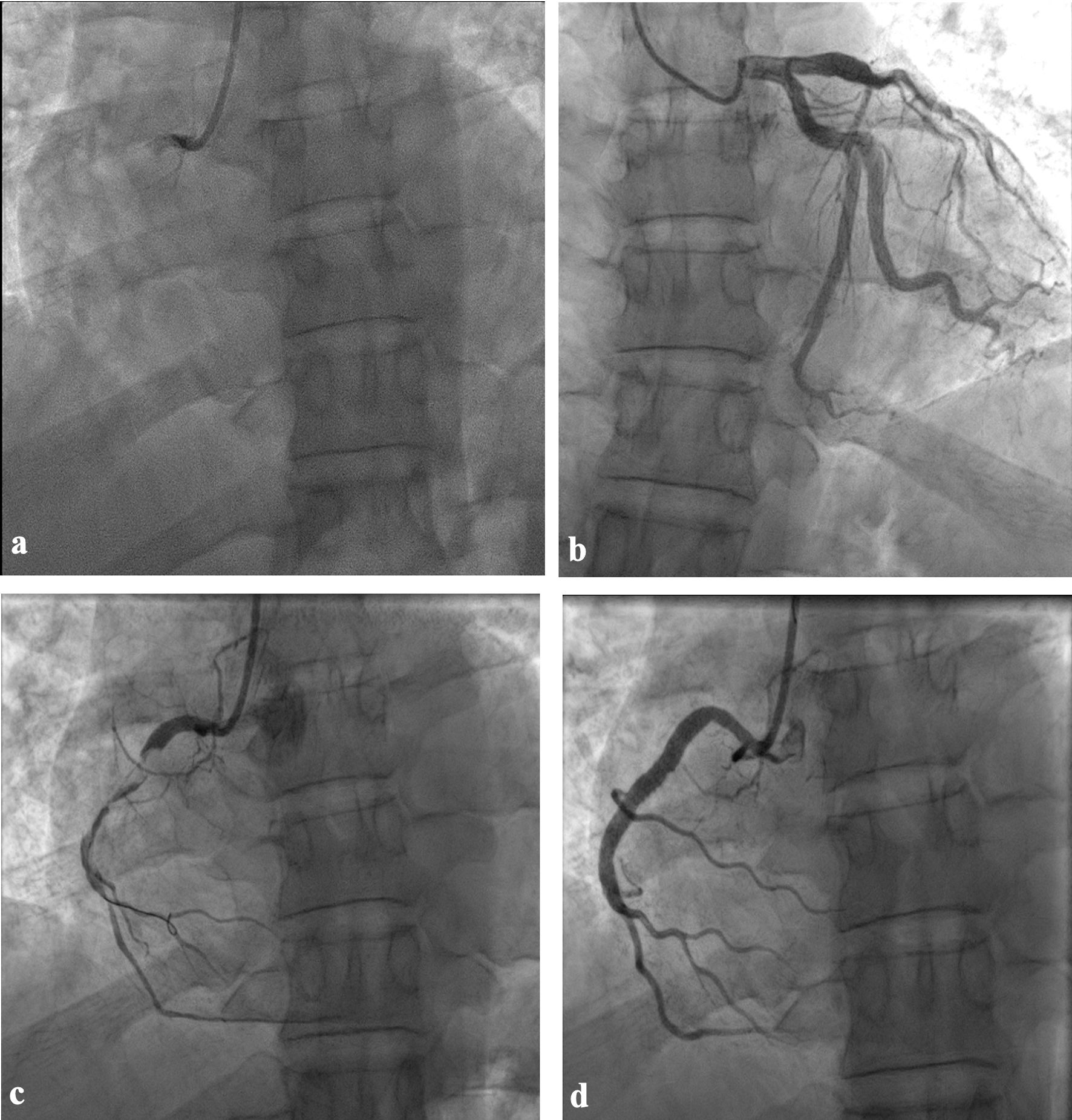 Click for large image | Figure 2. Coronary angiography and angioplasty. (a) Right coronary proximal total occlusion. (b) Left system ectasia in left anterior descending and first obtuse marginal arteries. (c) After thrombus aspiration attempt. (d) Final result after stent implantation. |
The patient was transferred to the Coronary Care Unit for close monitoring; he was kept on 24-h IV infusion of tirofiban, planned for re-look CAG with intravascular ultrasound (IVUS) guidance.
Eighteen hours later, the patient suffered from new onset severe pleuritic chest pain, with new widespread ST elevation more prominent in inferior leads II, III and aVF, and ST depression in aVR (Fig. 3). Echocardiogram showed mild pericardial effusion.
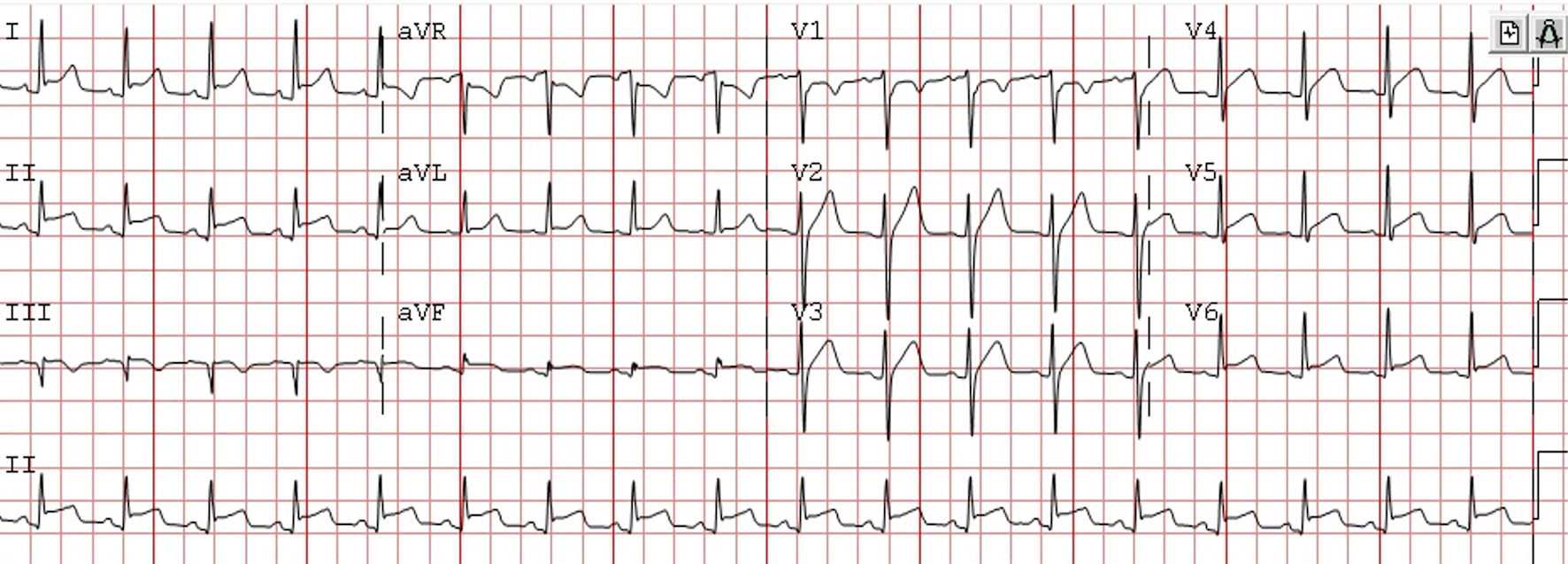 Click for large image | Figure 3. Electrocardiogram after 18 h in coronary care unit (CCU) demonstrating new widespread ST elevation more prominent in inferior leads II, III and aVF with ST depression in aVR. |
He was taken immediately to the catheterization laboratory (Cath Lab) for CAG through right radial artery access. It showed totally occluded RCA (100%) with TIMI 0 from proximal segment with acute stent thrombosis.
Aspiration thrombectomy was performed with large thrombotic material removed. Balloon angioplasty was done, but unfortunately it did not help to improve flow (Fig. 4a). Therefore, IVUS was performed to evaluate the mid-segment RCA stent. It showed that the stent was expanded well with no edge dissection, yet heavy calcified thrombi were recognized. We implanted a 3.5 × 28 mm XIENCE Skypoint drug-eluting stent from ostium to mid-segment overlapped with previous stent. Then it was optimized with non-compliant balloon of 4.0 × 15 mm with ostial flaring (Fig. 4b). Then the flow got compromised, so, multiple boluses of intracoronary adenosine, nitroglycerin, and epinephrine boluses were all given, but it showed minimal flow improvement (Fig. 4c, d). There was distal RCA thrombus shift. We opted for direct stenting to that area using a 2.25 × 15 mm XIENCE Skypoint drug-eluting stent to secure the flow distally. Post dilatation was done with a 2.75 × 15 mm non-compliant balloon (Fig. 4e). It was complicated with no-reflow. Another trial of aspiration thrombectomy was performed and distal bed vasodilator therapy delivered through a micro catheter for multiple times. IVUS was used to rule out any mechanical complication. It revealed good stent expansion and apposition with no edge dissections. However, it showed heavy in-stent thrombus formation (Fig. 5). Intracoronary adenosine, nitroglycerin and epinephrine all failed to improve no-reflow (Fig. 4f). However, the patient remained pain free with stable vital signs, and no significant ECG changes were observed. We opted to stop at this stage and to switch him to more potent therapy from ticagrelor to prasugrel, aspirin and tirofiban infusion continued for another 24 h. Rheumatologic assessment revealed the history of four different attacks of oral ulcers and one attack of genital ulcer over the past year.
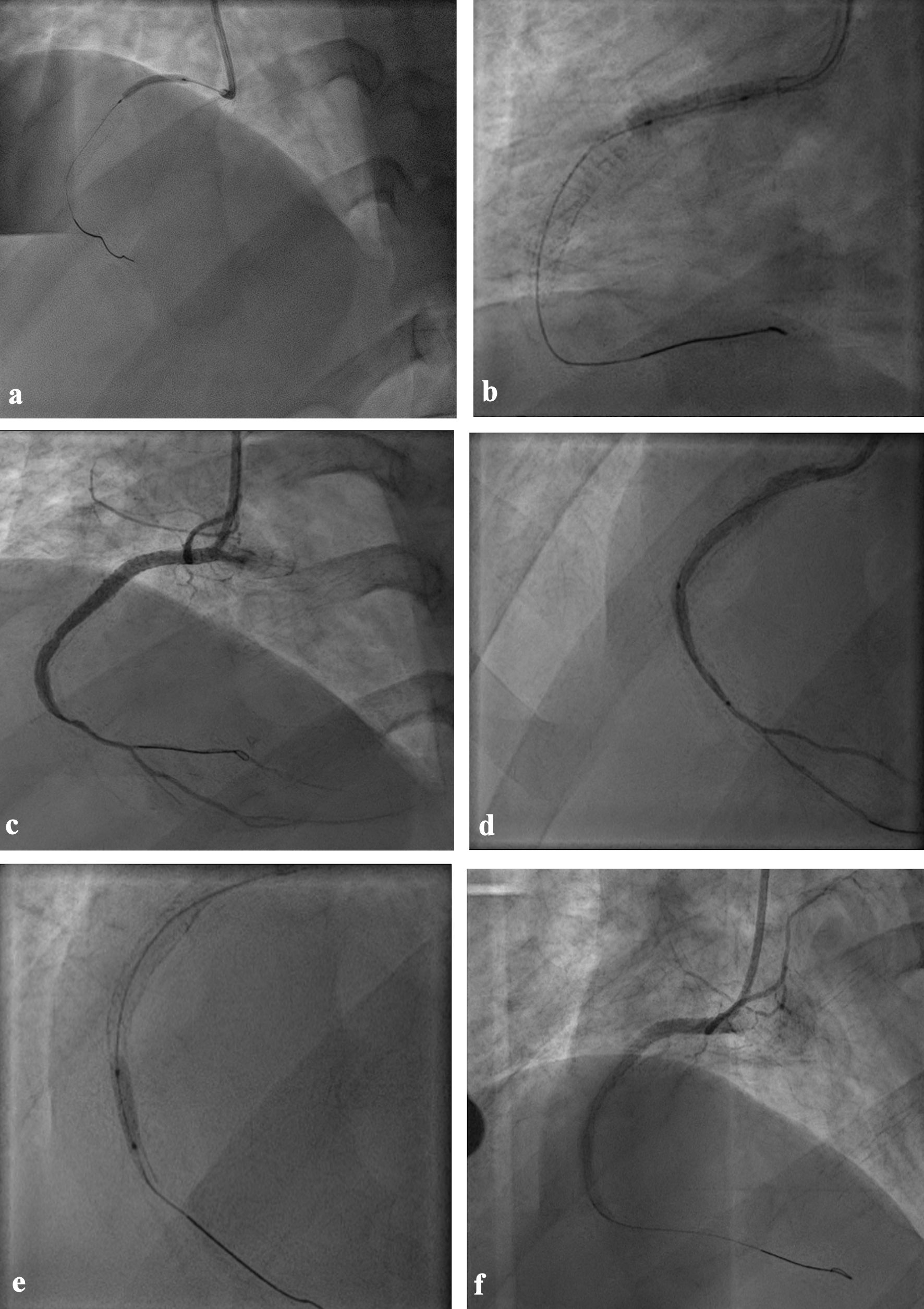 Click for large image | Figure 4. The second angioplasty (a) Balloon angioplasty after aspiration thrombectomy. (b) Stent implantation from ostium to mid-segment overlapping with the previous stent. (c) After injection of intracoronary adrenaline, adenosine and epinephrine. (d) Distal direct stent implantation. (e) Post dilatation using non-compliant balloon. (f) Final result after aspiration thrombectomy, vasodilator therapy and IVUS guidance to exclude mechanical complications showing distal no-reflow. IVUS: intravascular ultrasound. |
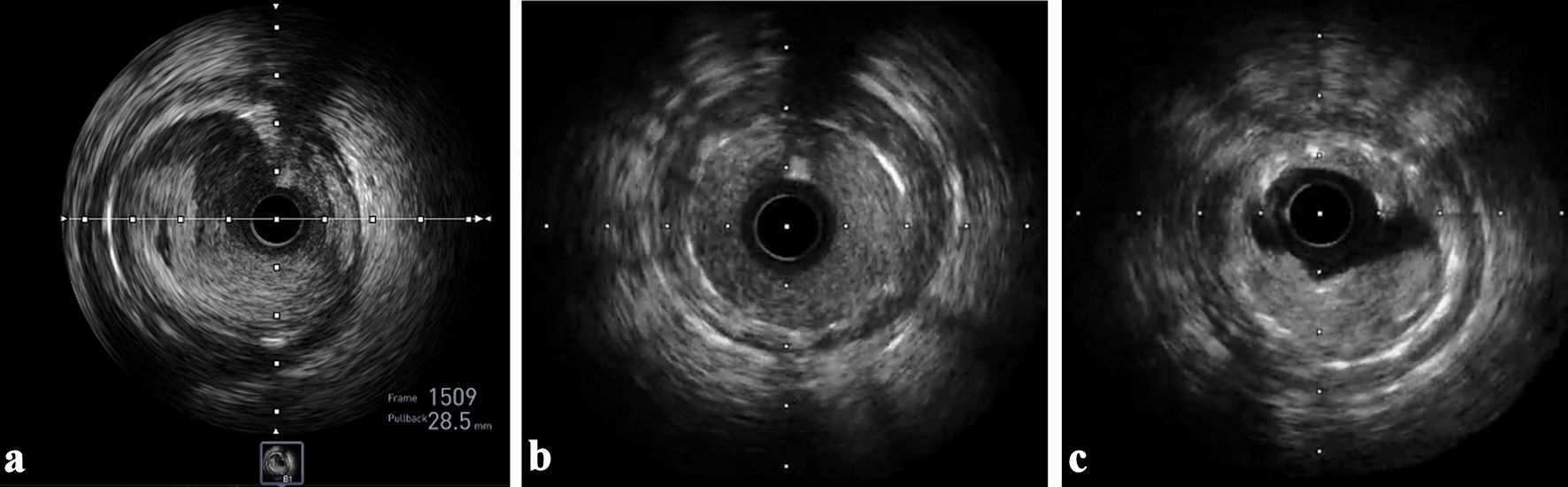 Click for large image | Figure 5. IVUS images. (a) Well opposed struts in proximal stent edge with no dissection. (b) Well opposed struts in distal stent edge with no dissection. (c) Acute in-stent thrombosis. IVUS: intravascular ultrasound. |
Twenty-four hours later, the patient complained of stitching chest pain, worse on leaning backward. ECG showed persistent widespread ST elevation. The echo-Doppler study showed mild pericardial effusion, and the inflammatory marker C-reactive protein (CRP) was high. The patient was diagnosed with post-myocardial infarction Dressler syndrome. Colchicine 500 mg two times and aspirin 600 mg three times daily were started. The patient was discharged home 2 days later with recommendation to follow up at the Outpatient Department (OPD) clinic after 1 week.
His laboratory investigations were shown in Table 1.
 Click to view | Table 1. Inpatient Laboratory Investigations |
Four days later the patient presented at the OPD with residual pleuritic chest pain. Follow-up ECG showed resolution of the widespread ST elevation (Fig. 6). Echocardiogram study showed mild pericardial effusion.
 Click for large image | Figure 6. Electrocardiogram 4 days after discharge showing resolved wide-spread ST elevation. |
The patient was reassured and advised to continue on the same medical treatment and advised to follow up after 2 weeks. Moreover, due to unexplained acute stent thrombosis and after exclusion of mechanical complications, hypercoagulable state was suspected. Laboratory tests were taken, and the sample was sent to the Biocentia Lab in Germany for exclusion of hereditary and autoimmune diseases (cytoplasmic anti-neutrophil cytoplasmic antibody (c-ANCA), perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA), lupus anticoagulant, protein C, S, anti-thrombin III activity, prothrombin mutation, beta 2 glycoprotein, human leukocyte antigen (HLA)-B51 and factor V gene mutation).
Two weeks later, the patient complained of minimal pleuritic chest pain. No dynamic changes were detected in ECG, yet echocardiogram showed more progression of the pericardial effusion (Fig. 7a). There was moderate pericardial effusion more at the apex. Therefore, oral aspirin dose was modified to 1 g every 6 h, prednisolone 30 mg tablet daily was added, and we kept him on prasugrel 10 mg tablet daily. After 4 days, the patient presented with minimal pleuritic chest pain. Echocardiogram showed regression of the pericardial effusion to mild (Fig. 7b). The patient was reassured and advised to come back to the clinic after 2 weeks.
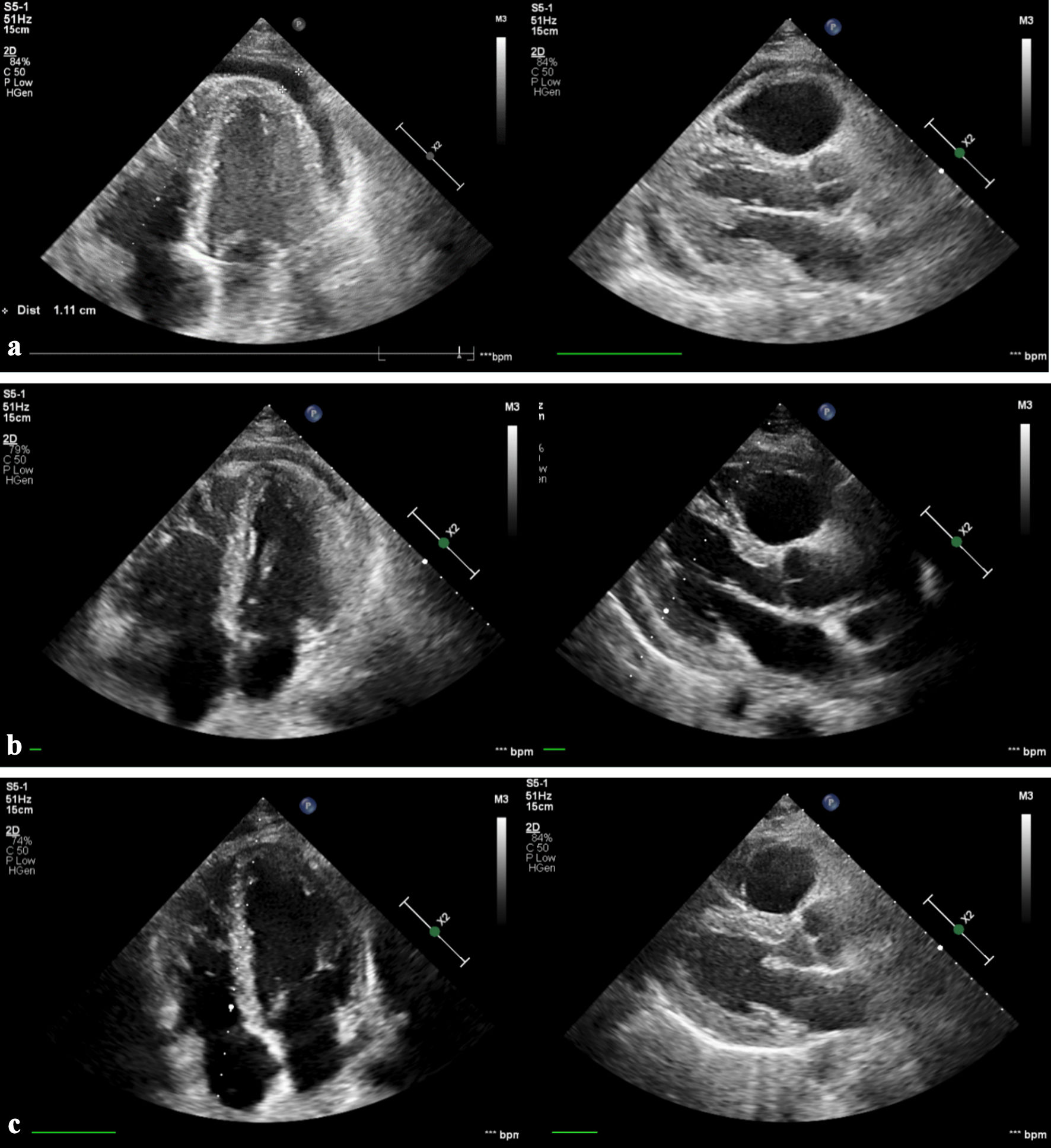 Click for large image | Figure 7. Echocardiography images. (a) Two weeks’ follow-up demonstrating moderate pericardial effusion at the apex. (b) Three weeks’ follow-up showing improvement to mild pericardial effusion. (c) Five weeks’ follow-up with complete resolution of pericardial effusion. |
At 5 weeks’ follow-up, the patient denied any chest pain. The echocardiogram showed no effusion (Fig. 7c), and inflammatory marker CRP returned back to normal level. However, the laboratory tests came back positive for HLA B51, which is strongly associated with BD.
Based on the past history of recurrent oral ulcers, genital ulcer, strong positive HLA B51 genetic test, and his presentation with AMI with hypercoagulable state, he was diagnosed as BD according to the International Criteria for Behcet Disease (ICBD).
| Discussion | ▴Top |
BD, first described in 1937 by Hulusi Behcet, is an autoimmune vaculitic disease. Its distribution was noted in Mediterranean countries, Iran, China, and Japan. It is a multi-system disorder affecting eye, skin, and musculoskeletal, neurological and cardiovascular systems [5, 6]. The ICBD criteria is considered a highly sensitive and specific tool for diagnosis and classification of this disease. Ocular lesions, oral aphthosis and genital aphthosis are each assigned 2 points, while skin lesions, central nervous system involvement and vascular manifestations 1 point each. The pathergy test, when used, was assigned 1 point. A patient scoring ≥ 4 points is classified as having BD [7].
Cardiac involvement was reported to be rare in BD. Yet, it is critical as it affects the young population and is associated with high mortality rate. The reported cardiac diseases include pericarditis, pericardial effusion, CAD, myocarditis, endocarditis and consequently, any type of arrhythmia could be generated [4].
CAD may vary between aneurysm, stenosis or arteritis. Myocarditis can be silent and progress to dilated cardiomyopathy and cardiac decompensation. Endocarditis may involve single or multiple valvular affection. Moreover, it may present with endocardial fibrosis affecting right and left ventricles [8] and may be associated with intracardiac thrombus formation [9, 10].
Most BD patients who suffer CADs had been previously diagnosed with the disease and were on regular treatment. Less commonly, as in our case, coronary complications may occur as the first manifestation of the disease [11]. Treatment of cardiovascular involvement in BD is largely aimed to reduce inflammation to suppress vasculitis [12]. Glucocorticoids and colchicine have been used for treatment with dramatic response in many cases; however, several side effects have been experienced from glucocorticoids use [13].
In our case, there was acute onset myocardial infarction with total occlusion of the right coronary artery. The decision to go for primary PCI, aspiration thrombectomy and stenting were taken as recommended in the guidelines in such cases. However, the patient suffered acute in-stent thrombosis and no-reflow. Moreover, he was complicated with pericarditis. Up to date, there is no clear recommendation for definitive treatment of CAD for BD patients. Yet, PCI may increase the risk of acute stent thrombosis. Dual antiplatelet treatment and colchicine regimen were given, and excellent clinical and radiological feedback was noted over regular follow-up.
Conclusions
BD can present for the first time with acute cardiac manifestations. AMI in young adults due to arterial thrombosis can be attributed to hypercoagulable state related to early expression of BD. Increased knowledge of AMI in young adults and its presentation in BD is necessary to reduce morbidity and mortality. Corticosteroids and colchicine may improve cardiac manifestations in BD. Coronary artery stenting may be associated with an increased risk of acute stent thrombosis. Corticosteroids and colchicine could help reduce inflammatory process of the disease and improve the outcome.
Acknowledgments
Nonet to declare.
Financial Disclosure
No funding was received for the case report.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
Written informed consent was obtained from the patient.
Author Contributions
Ahmed Hegazi Abdelsamie contributed to the study design, participated in data collection and writing of the case report. Nayef Al-Asiri participated in data collection and writing of the discussion.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AMI: acute myocardial infarction; BD: Behcet disease; CAD: coronary artery disease; CAG: coronary angiography; CRP: C-reactive protein; ECG: electrocardiogram; ICBD: International Criteria for Behcet disease; IV: intravenous; IVUS: intravascular ultrasound; OPD: Outpatient Department; PCI: percutaneous coronary intervention; TIMI: Thrombolysis In Myocardial Infarction
| References | ▴Top |
- Rallidis LS, Xenogiannis I, Brilakis ES, Bhatt DL. Causes, angiographic characteristics, and management of premature myocardial infarction: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;79(24):2431-2449.
doi pubmed - Sagris M, Antonopoulos AS, Theofilis P, Oikonomou E, Siasos G, Tsalamandris S, Antoniades C, et al. Risk factors profile of young and older patients with myocardial infarction. Cardiovasc Res. 2022;118(10):2281-2292.
doi pubmed - Sakr H, Azazy AS, Hillani A, Ebada M, Alharbi A, Alshalash S, Abazid R, et al. Clinical profiles and outcomes of acute ST-segment elevation myocardial infarction in young adults in a tertiary care center in Saudi Arabia. Saudi Med J. 2021;42(11):1201-1208.
doi pubmed pmc - Geri G, Wechsler B, Thi Huong DL, Isnard R, Piette JC, Amoura Z, Resche-Rigon M, et al. Spectrum of cardiac lesions in Behcet disease: a series of 52 patients and review of the literature. Medicine (Baltimore). 2012;91(1):25-34.
doi pubmed - Davatchi F. Behcet's disease. In: Hows HS, Feng PH (eds). Textbook of Clinical Rheumatology. National Arthritis Foundation, Singapore. 1998; p. 298-315.
- Shahram F, Davatchi F, Akbarian M, et al. The 1996 survey of Behcet's disease in Iran, study of 3153 cases. In: Hamza H (ed). Behcet's disease. Pub Adhoua, Tunisia. 1997; p. 165-169.
- International Team for the Revision of the International Criteria for Behcet's Disease (ITR-ICBD). The International Criteria for Behcet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28(3):338-347.
doi pubmed - Huong DL, Wechsler B, Papo T, de Zuttere D, Bletry O, Hernigou A, Delcourt A, et al. Endomyocardial fibrosis in Behcet's disease. Ann Rheum Dis. 1997;56(3):205-208.
doi pubmed pmc - Huong DL, Dolmazon C, De Zuttere D, Wechsler B, Godeau P, Piette JC. Complete recovery of right intraventricular thrombus and pulmonary arteritis in Behcet's disease. Br J Rheumatol. 1997;36(1):130-132.
doi pubmed - Madanat WY, Prokaeva TB, Kotel'nikova GP, Alekberova ZS. Endocarditis with left atrial thrombus formation in Behcet's disease mimicking myxoma. J Rheumatol. 1993;20(11):1982-1984.
pubmed - Saadoun D, Wechsler B. Behcet's disease. Orphanet J Rare Dis. 2012;7:20.
doi pubmed pmc - Demirelli S, Degirmenci H, Inci S, Arisoy A. Cardiac manifestations in Behcet's disease. Intractable Rare Dis Res. 2015;4(2):70-75.
doi pubmed pmc - Owlia MB, Mehrpoor G. Behcet's disease: new concepts in cardiovascular involvements and future direction for treatment. ISRN Pharmacol. 2012;2012:760484.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


