| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Short Communication
Volume 16, Number 4, April 2024, pages 174-181
Feasibility Study of a Prototype Wearable Inertial Measurement Unit for Elderly Postural Sway Assessment
Siriphan Kongsawasdia , Chakrit Wiboonsuntharangkoonb
, Pattaraporn Tajarernmuanga
, Kittichai Wantanajittikulc, d
aDepartment of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
bResearch Administration, Academic Services and International Relations Section, Faculty of Engineering, Chiang Mai University, Chiang Mai, Thailand
cDepartment of Radiologic Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
dCorresponding Author: Kittichai Wantanajittikul, Department of Radiologic Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
Manuscript submitted February 12, 2024, accepted March 7, 2024, published online April 30, 2024
Short title: Study Wearable IMU for Elderly Postural Sway
doi: https://doi.org/10.14740/jocmr5125
| Abstract | ▴Top |
Background: Falls are a major public health problem among older adults since they are a primary cause of injuries, functional decline and mortality. Identifying individuals susceptible to falls enables early intervention and prevention strategies. Currently, wearable sensors have emerged as a promising tool for assessing balance and mobility due to their affordability, compact size, and established efficacy. Therefore, the objective of the present study was to evaluate inertial measurement unit (IMU)-based postural sway metrics during quiet stance with four different bases of support and compare them among elderly individuals who are at risk of falling and those who are not.
Methods: A triaxial IMU prototype was developed for evaluating postural sway during quiet stance, with various bases of support. Totally, 103 elderly participants with mean age of 68.5 ± 5.7 years were included. Sway metrics, including the root mean square (RMS) of magnitude, summation of range of signal (Range), summation of sway area (SA) and summation of distance (SD) were employed to detect sway perturbations.
Results: All of the sway metrics revealed a significantly increasing magnitude of signal trajectory with a decreasing base of support. When comparing IMU sway metrics between groups of individuals at potential risk and non-risk of falls, statistically significant differences were observed in some variables, including RMS, Range, and SA during semi-tandem stance, and Range and SA during one-leg standing.
Conclusions: The findings support earlier studies that demonstrated the objective nature of the IMU in assessing balance and predicting future risk of falls. Limited significant findings in this study may be due to the lower sampling rate of the IMU prototype (50 Hz) compared to commonly reported frequencies (100 Hz), as well as the inclusion of elderly ambulatory participants who were capable of being independent in their daily activities. The IMU is capable of providing comprehensive data, and detecting subtle changes, early signs of balance impairment and fall tendencies.
Keywords: Wearable sensor; IMU; Inertial sensor; Postural sway; Static balance
| Introduction | ▴Top |
Falls are the major cause of long-term health problems or mortality in the elderly population. Since 1990, total global deaths and disability-adjusted life years (DALYs) have increased consistently due to falls, with mortality counts almost doubled by 2017 [1]. The World Health Organization estimated that falls are the second leading cause of unintentional injury deaths worldwide, and the most common cause of injury-related hospital admissions among older adults [2]. The incidence of falls and associated injuries is expected to rise, not only due to the growing population of older adults, but also because of the increasing prevalence of multimorbidity, numerous medications, and increased frailty within this group [2, 3]. Injuries from falls are the leading cause of disability, resulting in various serious consequences, such as hip fractures and traumatic brain injuries, which significantly impact long-term functional abilities [4]. Older adults face an increased risk of falls due to age-related physiological changes, including poor balance, impaired vision, hearing loss, medication-induced dizziness, and physical conditions associated with musculoskeletal and neurological problems. Postural control is a complex motor skill, based on interaction of dynamic sensorimotor processes and the ability to orient the body parts with respect to gravity, support surface and visual surround, and internal references are a critical component of postural control [5]. Postural stability is a major fundamental for achieving balance by maintaining body center of mass (COM) within the limit of stability, with minimal sway [6, 7]. Thus, the measurement of postural instability, by evaluating COM displacement coordinates during quiet stance, could be utilized in forecasting the incidence of falls, as reported in earlier studies [8-12]. Clinical assessments of fall risk, such as the Berg Balance Scale and Timed Up and Go, are used widely in healthcare settings to determine the likelihood of falls among older adults [1-3]. However, these approaches are subjective and lack discriminative ability [4, 12]. Laboratory examinations such as posturography using force platforms and optoelectronic systems have been used to provide objective and reliable measurements for balance evaluation. The displacement trajectory of center of pressure (COP) represents balance performance [9, 13, 14]; although this is recognized as standard equipment, it is not appropriate for employment in routine clinical settings, as it needs to be used in a costly laboratory setting [15, 16]. To date, an alternative, based on wearable sensors such as the inertial measurement unit (IMU), is a promising solution for developing a wearable monitoring system, because of its low cost, compact size, and proven ability to evaluate balance and gait [4, 17, 18]. The integration of accelerometers, gyroscopes, and magnetometers provides accurate information on body spatial orientation and motion, as well as ability to detect the trajectory of COM, in order to maintain standing balance within the limits of stability. The IMU captures three-dimensional motion and has demonstrated accuracy when compared to standard devices such as force platforms and motion-capture systems [17, 19, 20]. Previous research revealed a significant correlation between accelerometer measures and force-plate-derived COP values, specifically for normalized path length, root mean square (RMS), and peak-to-peak values across various standing balance test conditions [14]. A previous study by the authors utilized supervised machine learning to determine the COP trajectory of a force-plate system, based on inertial sensor metrics, yielding excellent agreement between the two measures (intraclass correlation coefficient (ICC): 0.89 - 0.95) [21]. Therefore, the objective of this study was to evaluate IMU-based postural sway metrics during quiet stance with four different bases of support and compare them among elderly individuals at risk and non-risk of falls based on clinical balance tests.
| Materials and Methods | ▴Top |
Participants
A total of 103 older adults (66 females and 37 males, aged 68.5 ± 5.7 years) were recruited from Chiang Mai province, Thailand. All of them were able to walk independently in their daily lives and reported being free of any neurological or musculoskeletal disorders, as well as severe visual impairment that impacted balance. Sixty-eight participants were in the potential risk of falling group with an average gait speed of 0.8 m/s, while 33 in the non-risk group had an average gait speed of 1.13 m/s. Participants in the fall risk group were classified based on their gait speed of less than 1 m/s [22]. The Short Physical Performance Battery (SPPB) is an objective measurement instrument of balance, lower extremity strength, and functional capacity in older adults [23]; and the fall risk assessment test, Thai version (Thai-FRT), is composed of six factors, including history of falls, impaired balance, being female, specific medication used, impaired visual acuity and Thai style house [24], and used to differentiate among the potential risk and non-risk group. The demographic characteristics of the participants are shown in Table 1. Age, weight, height, and body mass index (BMI) were not significantly different between the groups. Gait speed, Thai-FRT and SPPB revealed significant differences between the groups. All procedures were approved by the Ethics Committee, Faculty of Associated Medical Sciences, Chiang Mai University (study code AMSEC-63EX-056 (2020)). The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
 Click to view | Table 1. Demographic Data and Balance Test of the Elderly Participants |
IMU sensor and data acquisition
This study developed an IMU prototype with a box measuring 60 × 65 × 25 mm in size, a weight of 79 g, and battery capacity of 2,000 mAh for 10-h continuous data collection. IMU signals were processed using a third-order high-pass Butterworth filter, with a sampling frequency of 50 Hz to minimize the impact of high-frequency noise. The sensor was attached to the L4-5 vertebrae region near the COM using an elastic belt, ensuring alignment of the sensor axes with the anatomical directions in the anteroposterior (AP), mediolateral (ML), and vertical (V) orientations (Fig. 1).
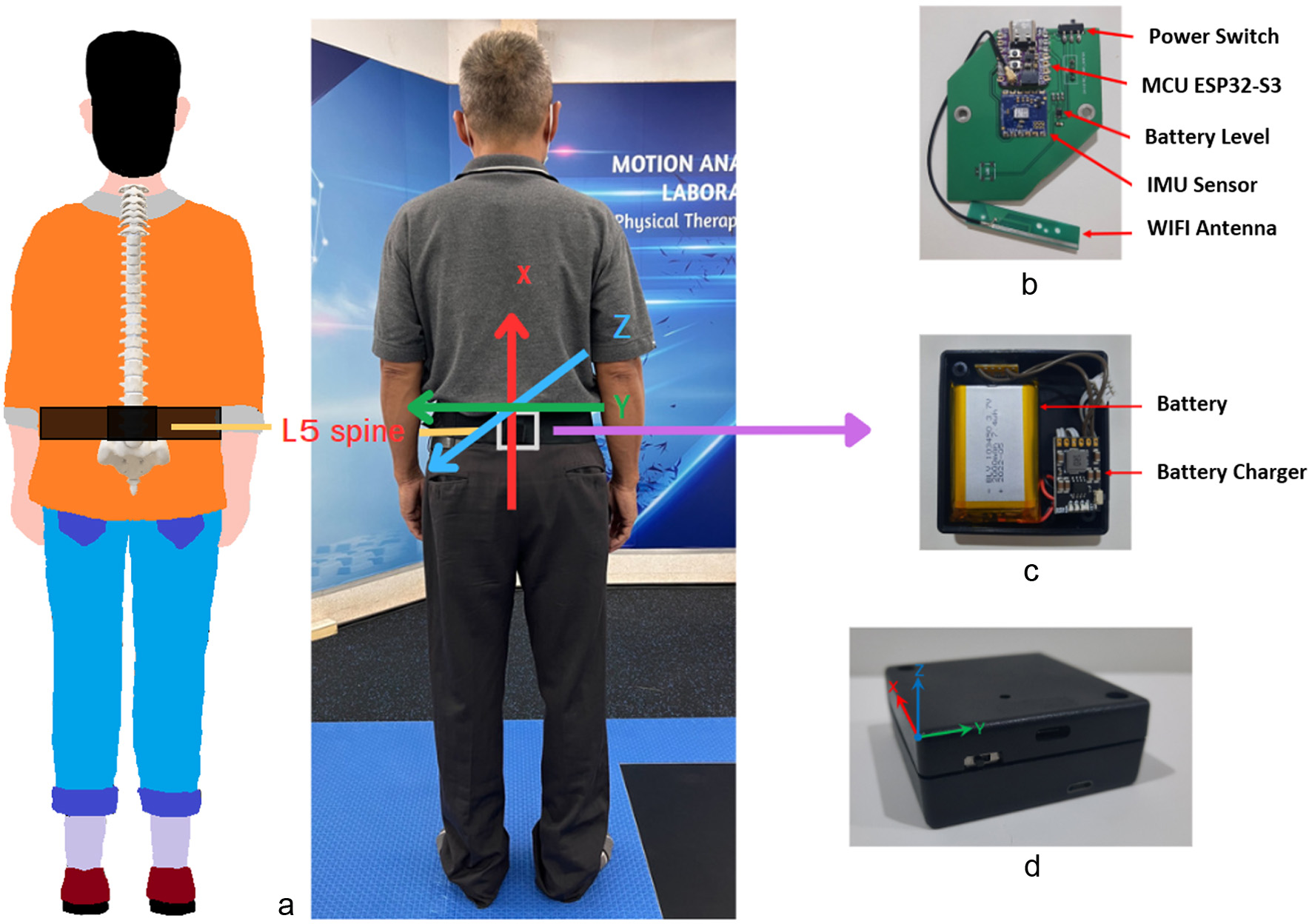 Click for large image | Figure 1. A prototype of the inertial sensor system. (a) Sensor placement in relation to the center of mass (COM) at the L5 vertebra in the lumbar region. (b, c) Subcomponents of the inertial measurement unit (IMU). (d) An assembled IMU. |
The gyroscope-derived angular velocities in three-dimensional axes (x, y, and z axes) were transmitted via WIFI to computer laptop, where a web-based application examined the perturbation of postural sway. The time-domain parameters were determined in order to quantify the magnitude and trajectory of postural sway in accordance with the earlier studies of Martinez-Mendez et al [15], Rouis et al [20], McManus et al [25] and the authors of this study [21]. The following metrics were utilized in these studies to detect sway perturbations: the RMS of magnitude, the generalized mean of the quadratic representing the average of signals, the Range, the summation of the range of signals, the summation of the sway area (SA) or area spanned from the signals normalized with respect to the duration of the measurement, and the summation of distance (SD) or total trajectory length. These metrics were calculated using equations 1) to 4) provided below:
The initial and last five seconds of each signal were eliminated in order to provide potential movement artifacts at the beginning and end of the balance test. All signal processing, feature extraction, and analyses were performed using MATLAB version 2021a (The Mathworks Inc., Natick, MA, USA) (Fig. 1).
Experimental procedure
The participants were instructed to perform a static standing balance test on a flat firm surface, in which the base of support was reduced gradually under four different conditions (Fig. 2) consisting of standing stance with arms at sides (ST), semi-tandem stance (S-TD), tandem stance (TD) (front of non-dominant foot placed beside heel of dominant foot), and one-leg standing (OLS). The participants were provided with instructions and trailed until achieving accurate performance prior to undertaking assessments. During the tests, the participants were asked to remove their shoes, arms at their sides and head in a normal forward-looking eye position and remain as still as possible in an upright standing position for 30 s. To ensure participant safety, a research assistant stood on either side of the individual throughout the testing protocol (Fig. 2).
 Click for large image | Figure 2. Static standing balance test under four conditions: standing stance with arms at sides (a), semi-tandem stance (b), tandem stance (front of non-dominant foot placed beside heel of dominant foot) (c), and one-leg standing (d). |
Statistical analysis
Continuous variables included demographic data (age, weight, height, BMI, and gait speed), and sway metrics were illustrated as the mean, standard deviation, and minimum and maximum values. Comparison between the two groups was carried out by a nonparametric test, due to the absence of normality and equal variance among them. Therefore, the Mann-Whitney U test was conducted for the two groups, and the Kruskal-Wallis test for multiple comparisons, with a pairwise post hoc analysis with the former. All statistical analyses were conducted with SPSS17.0 software (Illinois, USA), using a 95% level of significance.
| Results | ▴Top |
The average magnitudes of IMU metrics, including standard deviation and maximum and minimum values, for controlling balance in four static stance conditions among older individuals are presented in Table 2. Based on the hypothesis in this study, observation of increased sway metrics in older individuals was expected, as indicated by the RMS, Range, SA and SD parameters, when balancing on a narrower base of support, indicating greater postural control challenges. To assess these differences, a nonparametric Kruskal-Wallis test was conducted for multiple independent variables, and a post hoc analysis using pairwise Mann-Whitney U tests revealed statistically significant differences (P < 0.001) between each testing procedure for all IMU parameters (Table 2, Fig. 3).
 Click to view | Table 2. Body Sway of IMU Variables for Each Test Condition |
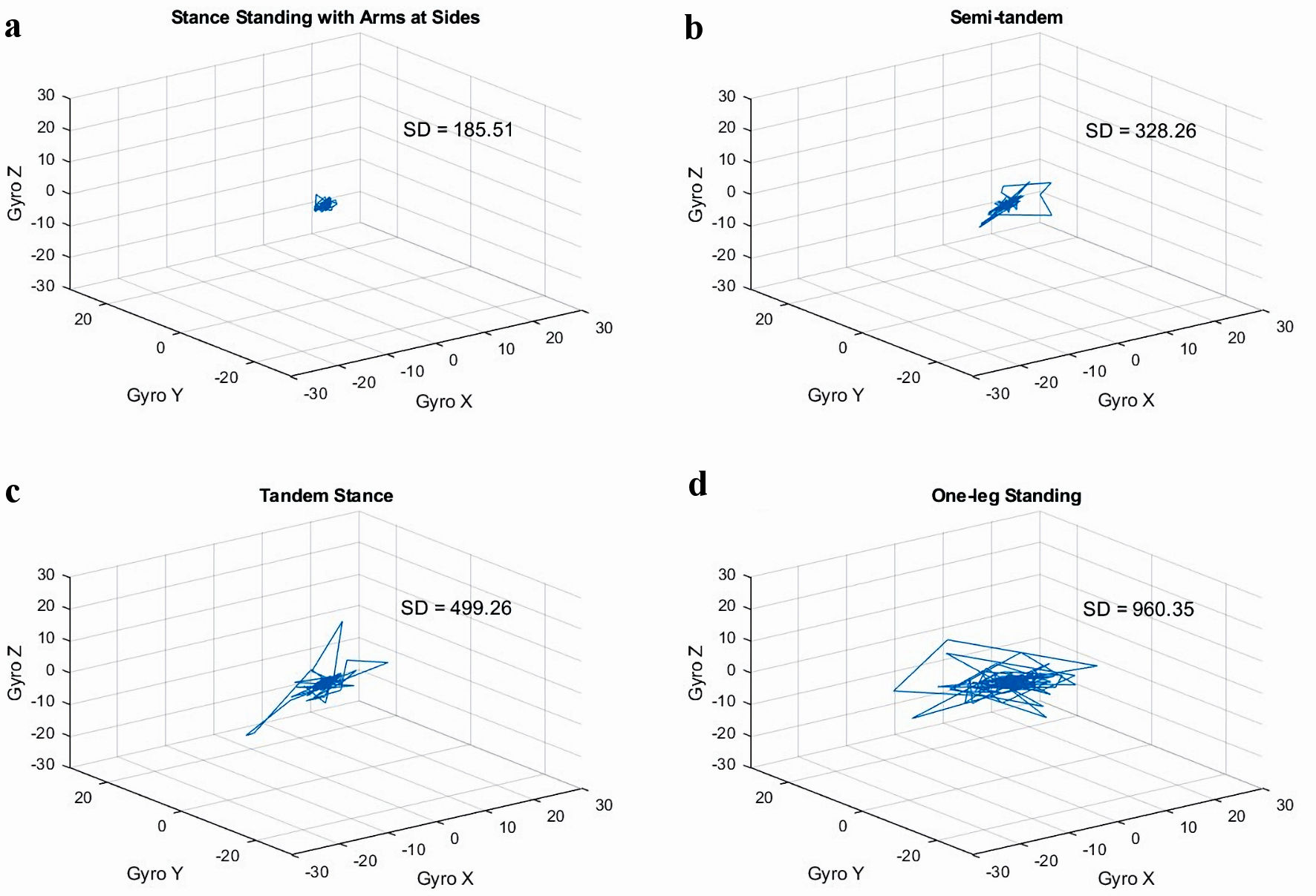 Click for large image | Figure 3. Summation of distance (SD), the sway diagram obtained from the IMU under each testing condition: (a) standing stance with arms at sides, (b) semi-tandem stance, (c) tandem stance and (d) one-leg standing. IMU: inertial measurement unit. |
Based on the gait speed of less than 1 m/s, the participants were categorized into two groups: non-risk and potential risk of falling. A comparison was carried out between the Thai-FRT and SPPB, which revealed significant differences between the two groups. When the IMU sway metrics were compared between the two groups, it became apparent that some of the IMU variables, which included the RMS, Range and SA during S-TD, and Range and SA during OLS, had statistically significant differences (P < 0.05) (Table 3, Fig. 4).
 Click to view | Table 3. IMU Body Sway Variables Between Non-Risk and Risk of Falling |
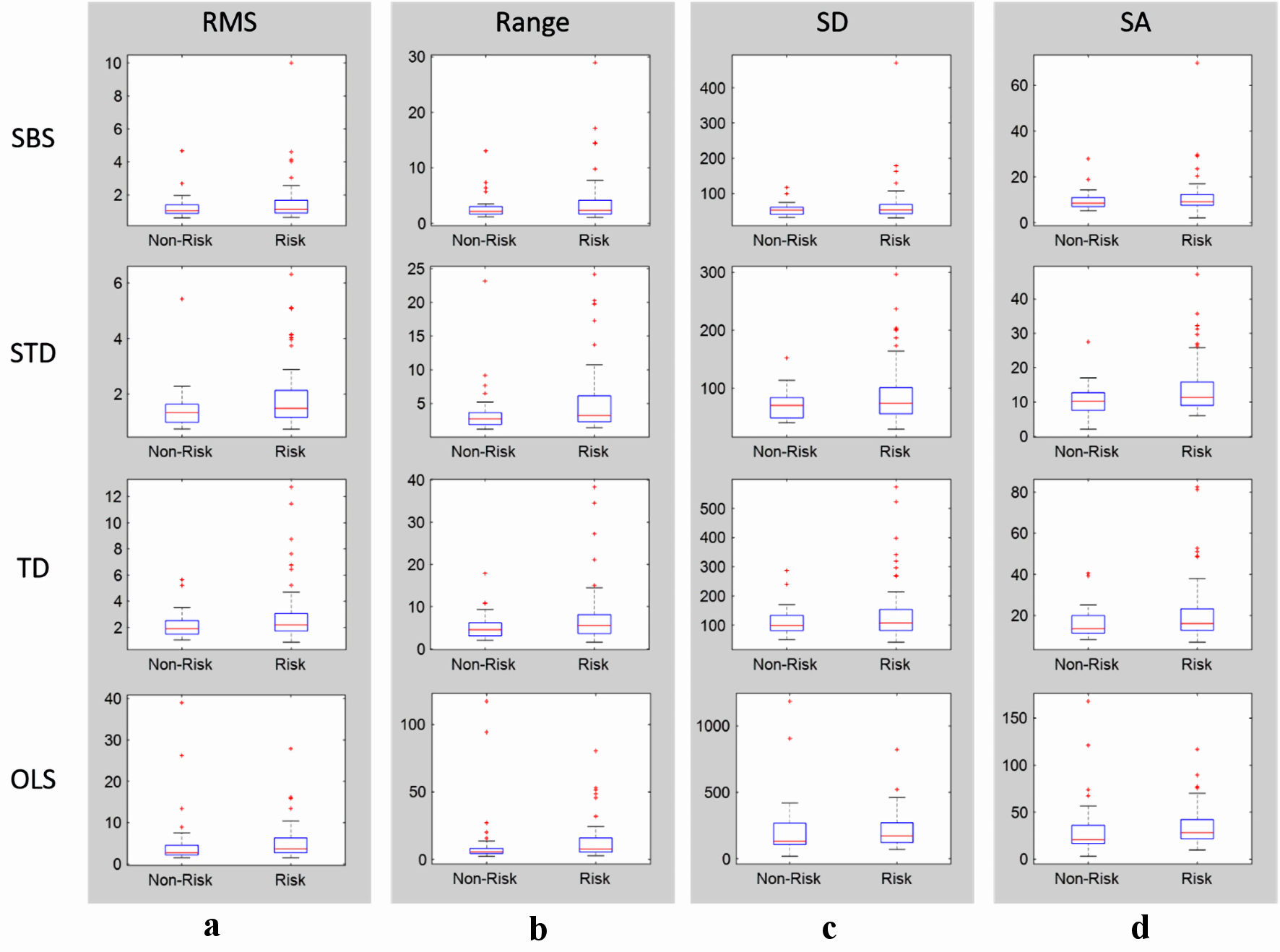 Click for large image | Figure 4. Boxplot depicting the median (50th percentile) and maximum and minimum values for each IMU parameter of the static standing balance test under the four conditions among both the non-risk and potential-risk groups (a) RMS. (b) Range. (c) SD. (d) SA. ST: standing stance with arms at sides; S-TD: semi-tandem stance; TD: tandem stance; OLS: one-leg standing; RMS: root mean square of magnitude; Range: summation of the range of signals; SA: summation of the sway area; SD: summation of distance; IMU: inertial measurement unit. |
| Discussion | ▴Top |
Maintenance of balance and body stability is necessary for people to participate in daily activities of living movement, which results from complex interaction between the sensory (visual, vestibular, and somatosensory) and motor systems, with integration from the central nervous system [6]. Falling is recognized as a serious health issue for the elderly, as it impacts not only themselves and their families, but also economically. As a result, surveillance and preventive actions should be prioritized. Assessing body sway during quiet standing is a well-established method for evaluating the ability of the human neuromuscular system to integrate and maintain an upright posture, thereby ensuring balance. With the current development of wearable sensor technology for measuring variables associated with standing balance, systematic studies by Ghislieri et al [17], Baker et al [26], Subramaniam et al [18], and others [4, 9, 11, 20] have demonstrated the ability of inertial sensors to identify postural sway and overcome clinical tests or a laboratory setting.
The objective of this study was to investigate changes in parameters derived from IMU signals under varying balance situations, depending on the area of support. Its findings support the established understanding of balance control; and with the principle that a wider base of support enhances stability, a larger area for the center of gravity (COG) to shift is provided, while maintaining equilibrium [5]. The results demonstrate an association between decreasing area of support and increased difficulty in maintaining balance. This is evident in the significantly higher magnitude of sway trajectory observed in the single-leg stance, compared to other test conditions. Furthermore, the significant differences observed across all parameters in varying test conditions suggest that the calculated metrics obtained from the IMU prototype are sensitive to changes in balance control strategies, which was employed by the participants. This provides evidence that the IMU-based approach has potential for an accurate assessment of balance function, particularly in situations influenced by lower limb function, as investigated in this study.
Despite the test conditions, parameters and sensor placement location were all based on recently reviewed studies [4, 17, 26]. Statistically significant differences were found in a few parameters when comparing between participants in the non-risk and potential risk of falling groups, including the RMS, Range, and summation of SA during S-TD, as well as the Range and SA during OLS (Table 3). This study identified the risk group based on low gait speed and confirmed it with clinical tests such as the SPPB, as previously reported [22, 24, 27, 28]. One potential factor could be attributed to the procedure of the data collection, which comprised ambulatory elderly participants, including those within the risk group, who retained the ability to walk independently on a daily basis. The prototype’s lower sampling rate of 50 Hz, compared to the reported sampling frequency of 100 Hz in systematic reviews, may have contributed to limited significant findings in this study [17, 26, 29]. However, a distinct benefit of the custom-built prototype is that it may provide access to raw data, thus enabling researchers to validate findings, develop new algorithms, and expand various types of motion analysis studies. This is a major advantage over commercial IMUs.
In conclusion, the findings of this study are consistent with earlier research, by demonstrating that the IMU is an objective assessment for balancing and predicting the probability of future falls [20, 26, 30]. They provide data from multiple axes, allowing for comprehensive evaluation of balance control, which contributes to better understanding of balance capabilities and fall risk factors in individuals. The IMU also has the potential to detect subtle changes or early signs of balance impairment and fall tendencies. As a result, it offers a portable and affordable option for balance assessment, with the added benefit of real-time monitoring, which makes it accessible in various settings such as clinical facilities, community centers, and home-based monitoring. However, given that this study was preliminary in nature, improvements to the IMU prototype, particularly in terms of sampling rate, are necessary for capturing small perturbations accurately. Future studies should focus on evaluating sway axes, such as antero-posterior and medio-lateral sway and incorporating the ankle strategy as a discriminating parameter for individuals at risk of falling.
Acknowledgments
The authors gratefully acknowledge the elderly volunteers who participated in this study.
Financial Disclosure
This work was funded by the Faculty of Associated Medical Sciences, Chiang Mai University, Thailand.
Conflict of Interest
None to declare.
Informed Consent
Completed written informed consent was obtained.
Author Contributions
Conceptualization: SK and KW. Development of prototype: KW and CW. Software: KW. Data collection: SK and PT. Writing the article: SK and KW. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data sets analyzed in this study are available from the corresponding author on reasonable request.
Abbreviations
AP: anteroposterior; BMI: body mass index; COM: center of mass; COP: center of pressure; IMU: inertial measurement unit; ML: mediolateral; OLS: one-leg standing; RMS: root mean square; SA: summation of sway area; SD: summation of distance; SPPB: Short Physical Performance Battery; ST: standing stance with arms at sides; S-TD: semi-tandem stance; TD: tandem stance; Thai-FRT: fall risk assessment test, Thai version; V: vertical
| References | ▴Top |
- James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, Hamilton EB, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev. 2020;26(Supp 1):i3-i11.
doi pubmed pmc - World Health Organization. Falls [Internet]. 2021 [Updated April 26, 2012]. Available from: https://www.who.int/news-room/fact-sheets/detail/falls. [cited May 8, 2023].
- Montero-Odasso M, van der Velde N, Martin FC, Petrovic M, Tan MP, Ryg J, Aguilar-Navarro S, et al. World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing. 2022;51(9):afac205.
doi pubmed pmc - Zampogna A, Mileti I, Palermo E, Celletti C, Paoloni M, Manoni A, Mazzetta I, et al. Fifteen years of wireless sensors for balance assessment in neurological disorders. Sensors (Basel). 2020;20(11):3247.
doi pubmed pmc - Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(Suppl 2):ii7-ii11.
doi pubmed - Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10(6):727-738.
doi pubmed - Pollock AS, Durward BR, Rowe PJ, Paul JP. What is balance? Clin Rehabil. 2000;14(4):402-406.
doi pubmed - Lee CH, Sun TL. Evaluation of postural stability based on a force plate and inertial sensor during static balance measurements. J Physiol Anthropol. 2018;37(1):27.
doi pubmed pmc - Mahoney JR, Oh-Park M, Ayers E, Verghese J. Quantitative trunk sway and prediction of incident falls in older adults. Gait Posture. 2017;58:183-187.
doi pubmed pmc - Gago MF, Fernandes V, Ferreira J, Silva H, Rocha L, Bicho E, Sousa N. Postural stability analysis with inertial measurement units in Alzheimer's disease. Dement Geriatr Cogn Dis Extra. 2014;4(1):22-30.
doi pubmed pmc - Ghahramani M, Stirling D, Naghdy F, Naghdy G, Potter J. Body postural sway analysis in older people with different fall histories. Med Biol Eng Comput. 2019;57(2):533-542.
doi pubmed - McGough EL, Hsu LY, Thompson H, Teri L. Concurrent validity of postural sway measures in older adults with cognitive impairment. Phys Occup Ther Geriatr. 2018;36(4):399-410.
doi pubmed pmc - Liapi E, Geschwind JF. Transcatheter arterial chemoembolization for liver cancer: is it time to distinguish conventional from drug-eluting chemoembolization? Cardiovasc Intervent Radiol. 2011;34(1):37-49.
doi pubmed pmc - Piirtola M, Era P. Force platform measurements as predictors of falls among older people - a review. Gerontology. 2006;52(1):1-16.
doi pubmed - Martinez-Mendez R, Sekine M, Tamura T. Postural sway parameters using a triaxial accelerometer: comparing elderly and young healthy adults. Comput Methods Biomech Biomed Engin. 2012;15(9):899-910.
doi pubmed - Seimetz C, Tan D, Katayama R, Lockhart T. A comparison between methods of measuring postrual stability: force plates versus accelerometers. Biomed Sci Instrum. 2012;48:386-392.
pubmed pmc - Ghislieri M, Gastaldi L, Pastorelli S, Tadano S, Agostini V. Wearable inertial sensors to assess standing balance: a systematic review. Sensors (Basel). 2019;19(19):4075.
doi pubmed pmc - Subramaniam S, Faisal AI, Deen MJ. Wearable sensor systems for fall risk assessment: a review. Front Digit Health. 2022;4:921506.
doi pubmed pmc - Neville C, Ludlow C, Rieger B. Measuring postural stability with an inertial sensor: validity and sensitivity. Med Devices (Auckl). 2015;8:447-455.
doi pubmed pmc - Rouis A, Rezzoug N, Gorce P. Validity of a low-cost wearable device for body sway parameter evaluation. Comput Methods Biomech Biomed Engin. 2014;17(Suppl 1):182-183.
doi pubmed - Wantanajittikul K, Wiboonsuntharangkoon C, Chuatrakoon B, Kongsawasdi S. Application of machine learning to predict trajectory of the center of pressure (COP) path of postural sway using a triaxial inertial sensor. ScientificWorldJournal. 2022;2022:9483665.
doi pubmed pmc - Kyrdalen IL, Thingstad P, Sandvik L, Ormstad H. Associations between gait speed and well-known fall risk factors among community-dwelling older adults. Physiother Res Int. 2019;24(1):e1743.
doi pubmed - Reid KF, Naumova EN, Carabello RJ, Phillips EM, Fielding RA. Lower extremity muscle mass predicts functional performance in mobility-limited elders. J Nutr Health Aging. 2008;12(7):493-498.
doi pubmed pmc - Baba T, Watanabe M, Ogihara H, Handa S, Sasamoto K, Okada S, Okuizumi H, et al. Validity of temporo-spatial characteristics of gait as an index for fall risk screening in community-dwelling older people. J Phys Ther Sci. 2023;35(3):265-269.
doi pubmed pmc - McManus K, Greene BR, Ader LGM, Caulfield B. Development of data-driven metrics for balance impairment and fall risk assessment in older adults. IEEE Trans Biomed Eng. 2022;69(7):2324-2332.
doi pubmed - Baker N, Gough C, Gordon SJ. Inertial sensor reliability and validity for static and dynamic balance in healthy adults: a systematic review. Sensors (Basel). 2021;21(15):5167.
doi pubmed pmc - Veronese N, Bolzetta F, Toffanello ED, Zambon S, De Rui M, Perissinotto E, Coin A, et al. Association between Short Physical Performance Battery and falls in older people: the Progetto Veneto Anziani Study. Rejuvenation Res. 2014;17(3):276-284.
doi pubmed pmc - Montero-Odasso M, Schapira M, Soriano ER, Varela M, Kaplan R, Camera LA, Mayorga LM. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60(10):1304-1309.
doi pubmed - Johnston W, O'Reilly M, Argent R, Caulfield B. Reliability, validity and utility of inertial sensor systems for postural control assessment in sport science and medicine applications: a systematic review. Sports Med. 2019;49(5):783-818.
doi pubmed - Sturnieks DL, Arnold R, Lord SR. Validity and reliability of the Swaymeter device for measuring postural sway. BMC Geriatr. 2011;11:63.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


