| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 16, Number 2-3, March 2024, pages 56-62
Economic Impact of COVID-19 on a Free-Standing Pediatric Ambulatory Center
Connor Randalla, Christian Mpodyb, c, Vidya T. Ramanc, Olubukola O. Nafiub, c, Joseph D. Tobiasb, c, d
aHeritage College of Osteopathic Medicine - Athens Campus, Athens, Ohio and Ohio University, Athens, OH, USA
bDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
cDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
dCorresponding Author: Joseph D. Tobias, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted December 5, 2023, accepted January 31, 2024, published online March 16, 2024
Short title: Economic Impact of COVID-19 on Pediatrics
doi: https://doi.org/10.14740/jocmr5083
| Abstract | ▴Top |
Background: Operating safely throughout the coronavirus disease 2019 (COVID-19) pandemic has required surgical centers to adapt and raise their level of readiness. Intuitively, additional expenses related to such adaptation may have resulted in an increase in the cost of surgical care. However, little is known about the magnitude of such an increase, and no study has evaluated the temporal variation in the costs of care throughout the pandemic. The aim of the current study was to evaluate the impact of COVID-19 on the cost of surgical and anesthetic care in a free-standing, pediatric ambulatory care center.
Methods: We performed a retrospective review of the electronic medical record (EMR) and financial data for pediatric ambulatory settings between 2019 and 2020 (April - August) from our tertiary care children’s hospital. The primary outcomes were the inflation-adjusted surgical cost for elective tonsillectomy, adenoidectomy, and tympanostomy tubes (BTI) placement procedures in children less than 18 years of age. These data were obtained from financial databases and aggregated into categories including anesthesia services, operating room services, recovery room services, and supply and medical devices.
Results: Costs per case to provide care were significantly higher following the COVID-19 pandemic in 2020 compared to 2019 across all services: anesthesia ($1,268 versus $1,143; cost ratio (CR): 1.11, 95% confidence interval (CI): 1.08 - 1.14, P-value < 0.001), operating room ($1,221 vs. $1,255; CR: 1.03, 95% CI: 1.02 - 1.04, P-value < 0.001), recovery room ($659 vs. $751; CR: 1.14, 95% CI: 1.10 - 1.18, P-value < 0.001), and supply ($150 vs. $271; CR: 1.81, 95% CI: 1.26 - 2.6, P-value = 0.001). There was an overall increase in healthcare service costs in 2020, with significant fluctuations in the early and mid-year months.
Conclusion: Our study identified specific economic impacts of COVID-19 on free-standing pediatric ambulatory centers, thereby highlighting the need for innovative practices with cost containment for sustainability of such specialized centers when dealing with future pandemics related to COVID-19 or other viral pathogens.
Keywords: Pediatric anesthesia; COVID-19; Preoperative testing; Personal protective equipment; Hospital economics
| Introduction | ▴Top |
The coronavirus disease 2019 (COVID-19) pandemic exposed a significant unmet need for preparedness among healthcare institutions [1]. Free-standing pediatric ambulatory centers may have underestimated the pandemic and its potential impact on daily operations including the cost of providing anesthesia and surgical services [2]. During this period, one of the primary challenges faced by ambulatory surgery centers was the implementation of additional safety measures to ensure the safe completion of scheduled surgical procedures due to the impact of COVID-19 on patients and healthcare providers [3-5]. This led to the deferral of numerous surgical procedures labeled as non-essential or elective, thereby negatively affecting patients and their quality of life [6]. In particular, pediatric patients may have been denied potentially life-improving surgeries such as tonsillectomies, adenoidectomies, or tympanostomy tube placements.
Recognizing the potential for the cancellation of these surgical procedures to result in a decline in the quality of patient care, surgical centers had to adapt and improve their readiness to treat patients safely and efficiently. To address the concerns arising from surgical procedure deferment, pediatric ambulatory centers adapted by implementing new regulations to ensure patient and healthcare worker safety when there was a resumption of elective surgery. These regulations, including strict adherence to social distancing, improved surface disinfection, use of personal protective equipment (PPE), and increased attention to hand-washing allowed centers to align with CDC guidelines and enhanced their ability to care for patients and yet prevent COVID-19 transmission and infection [7]. With these measures in place, pediatric ambulatory centers successfully increased their capacity to perform surgical procedures. However, as they adapted, new issues emerged including limitations in the supply chain led to increased cost of surgical care.
Although it is known that the cost of surgical care increased during the COVID-19 era for pediatric ambulatory care centers, the exact magnitude of this increase and the factors primarily responsible for it remain uncertain. To date, there has been limited emphasis on the impact of supply chain limitations on increasing the overall cost of surgical care [8]. Understanding this connection enables the management of pediatric ambulatory surgical centers to navigate similar supply chain challenges more effectively should we be faced with future pandemics. Given the ongoing risk of future global pandemics, preparation is crucial for pediatric ambulatory surgical centers to ensure the timely completion of non-urgent surgical procedures which can significantly impact the quality of life of patients as well as result in ongoing comorbidities if not addressed. With the goal of enhancing the health outcomes for children and their families during future global pandemics, our study evaluates the economic and financial impact of COVID-19 on pediatric surgery. We have collected data on the costs of overall care, otolaryngology cases, recovery room care, operating room services, anesthesia services, and medical supplies to examine how these costs evolved during the pandemic. The primary goal is to shed light on the fluctuation in surgical costs during the COVID-19 pandemic, offering valuable insights for hospitals and healthcare professionals.
| Materials and Methods | ▴Top |
Study setting, design and population
This retrospective study was approved by the Institutional Review Board of Nationwide Children’s Hospital (Columbus, Ohio) and was conducted in compliance with the ethical standards of clinical research on human subjects and the Helsinki Declaration. Following IRB approval, we performed a cross-sectional study integrating the electronic medical record (EMR) of our free-standing, tertiary care children’s hospital and financial data for pediatric ambulatory settings, comparing the months of April through August for the years 2019 and 2020. For the purpose of the study, a convenience sample that included two 6-month periods of time was chosen using the database from the operating room of our own hospital, Nationwide Children’s Hospital (NCH). NCH is a large tertiary care, free-standing children’s hospital in the state of Ohio. This allowed a time-based comparison of a 6-month period prior to the COVID-19 pandemic (2019) with a 6-month period during the height of the pandemic (2020) and its impact on surgical volumes and cost. The study cohort included children < 18 years who underwent elective tonsillectomy, adenoidectomy, or tympanostomy tubes (BTI) placement.
Study outcomes
Our study outcome was the inflation-adjusted surgical costs, defined as the total amount spent to deliver care, including wages, supplies, and utility costs. These costs were obtained from financial databases and aggregated into categories, including anesthesia services, operating room services, recovery room services, and supply and medical devices. We inflated the costs to the 2021 US dollars using Consumer Price Index for the gross domestic products [9].
Statistical analysis
Categorical variables were presented as frequency and column percentage. We tested the normality of continuous variables by using the one-sample Kolmogorov-Smirnov test. Non-continuous variables were summarized as median (interquartile range (IQR)). Poisson regression was used to estimate the average costs and their 95% confidence interval (CI) for 2019 and 2020. To compare the costs between 2019 and 2020, we used a generalized linear model with gamma distribution to account for the non-normality of costs. Results were presented as cost ratios (CRs) and their 95% CI. We performed all data analyses and management using Stata, version 16 (StataCorp, College Station, TX).
| Results | ▴Top |
The study cohort included 1,797 children who underwent elective otolaryngology surgery during 2019 compared to 622 patients during the same period in 2020, resulting in a 52.9% reduction in case volumes (Table 1). In 2020, the children who were cared for were older (P-value < 0.001) and had a higher American Society of Anesthesiologists (ASA) physical classification status (P value = 0.001). Costs per case to provide care were significantly higher in 2020 compared to 2019 across all services: anesthesia ($1,268 versus $1,143; CR: 1.11, 95% CI: 1.08 - 1.14, P-value < 0.001), operating room ($1,221 vs. $1,255; CR: 1.03, 95% CI: 1.02 - 1.04, P-value < 0.001), recovery room ($659 vs. $751; CR: 1.14, 95% CI: 1.10 - 1.18, P-value < 0.001), and supply and medical devices ($150 vs. $271; CR: 1.81, 95% CI: 1.26 - 2.6, P-value = 0.001) (Table 2 and Figs. 1-5). Figures 1 to 5 summarize the comparative trend in average costs for various healthcare services between the study months of the years 2019 versus 2020. Starting with operating room services, there was an observable downward trend from March to April 2020, subsequently followed by a steady rise through August, with the costs generally surpassing those of 2019, except for a notable dip in April 2020. In contrast, the costs for anesthesia services in 2020 displayed more variability, with a significant decline in April and a peak in July, suggesting an increase in cost volatility during this year compared to the more stable trend observed in 2019.
 Click to view | Table 1. Demographic Data of the Study Cohort |
 Click to view | Table 2. Average Healthcare-Related Costs |
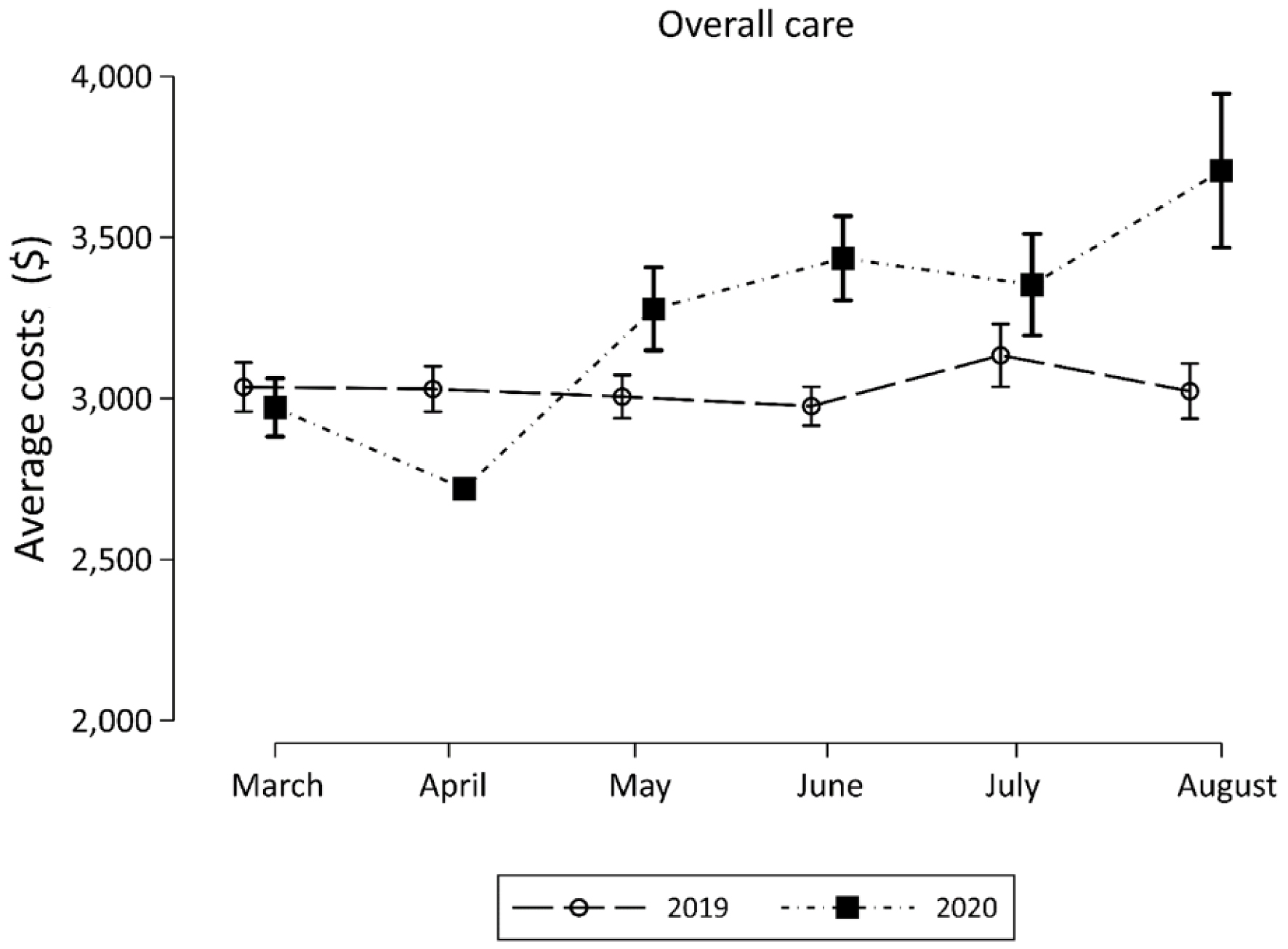 Click for large image | Figure 1. Average cost of overall care during April - August in 2019 compared to April - August 2020. |
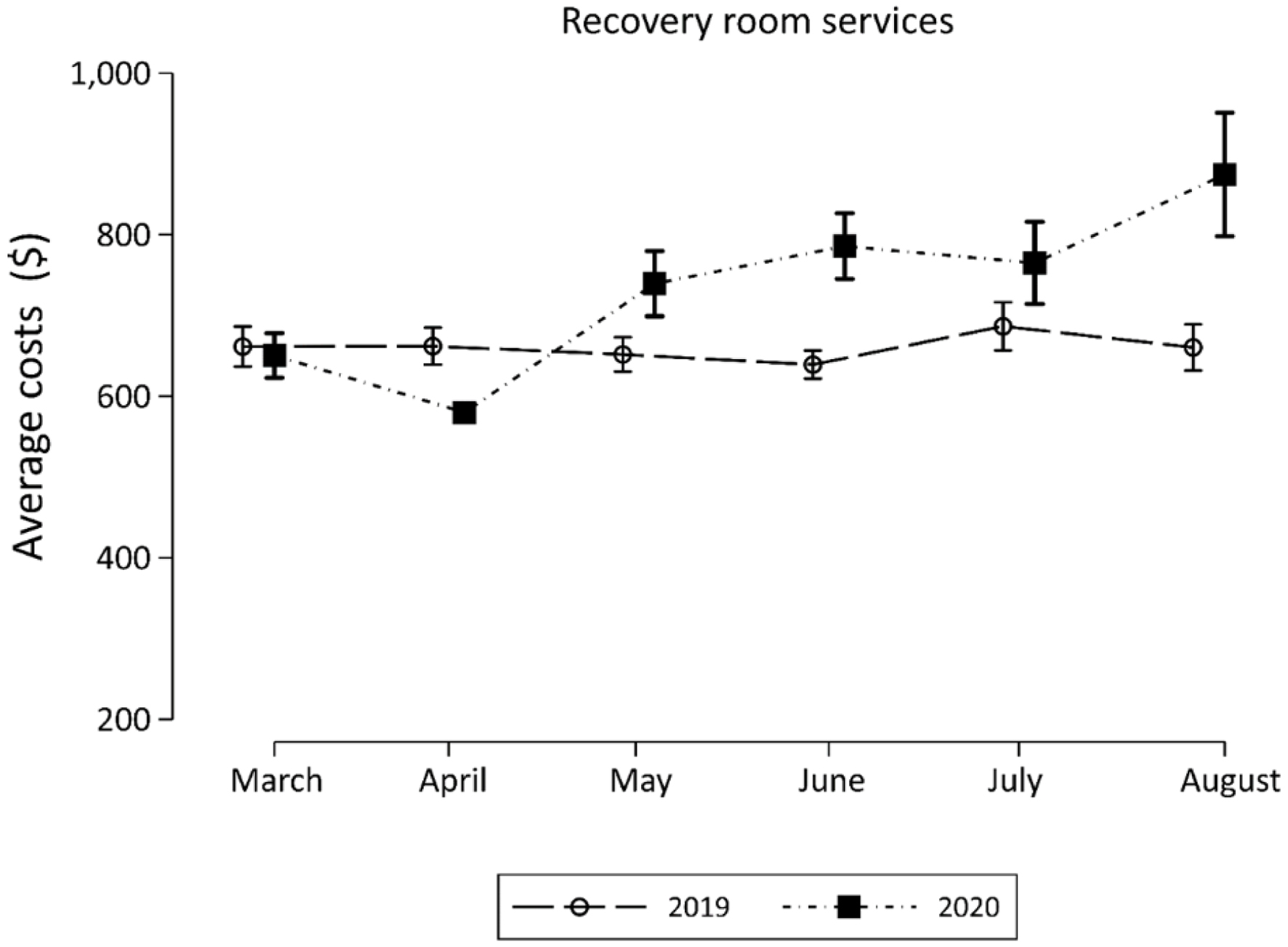 Click for large image | Figure 2. Average cost of recovery room services during April - August in 2019 compared to April - August 2020. |
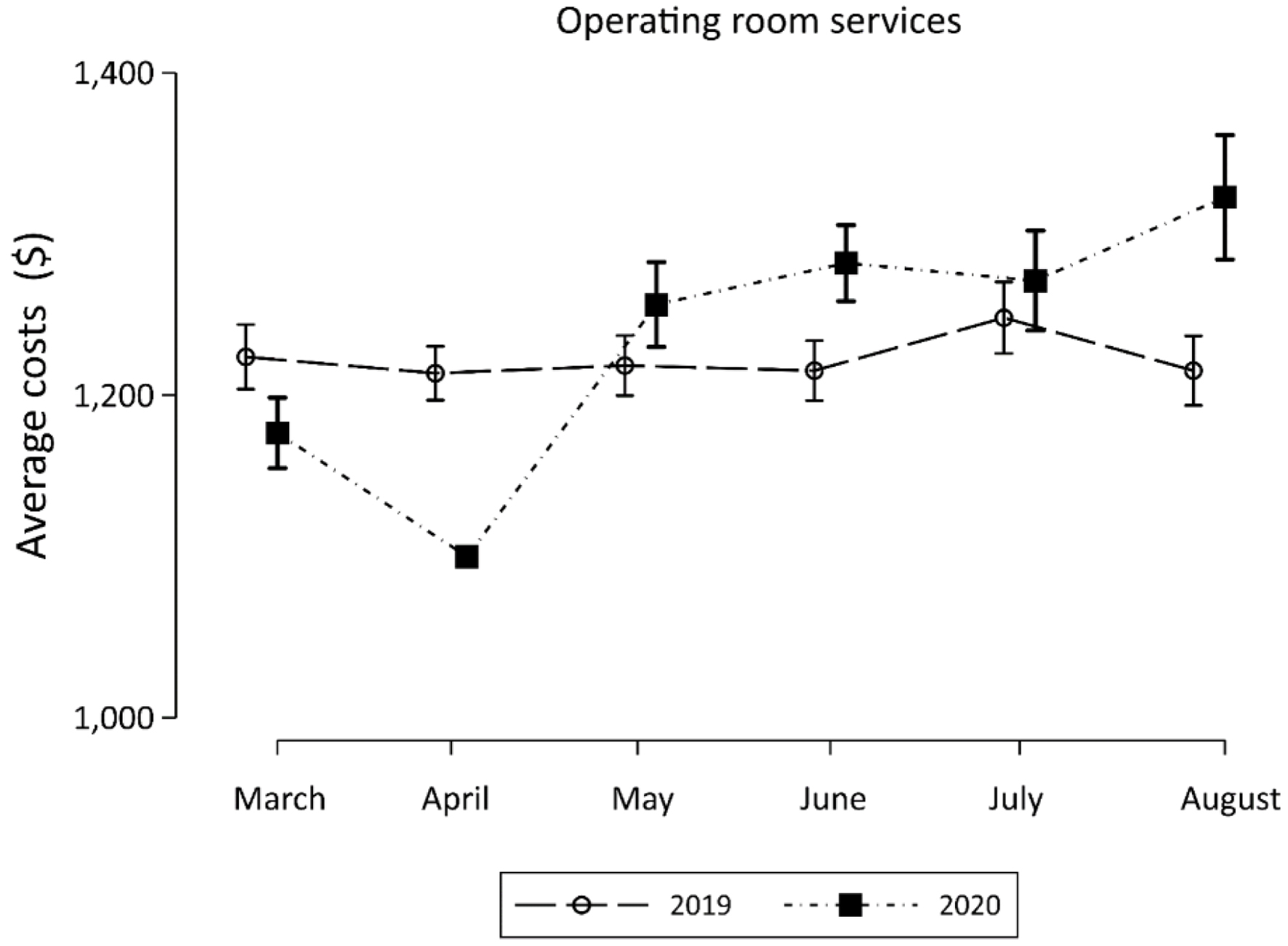 Click for large image | Figure 3. Average cost of operating room services during April - August in 2019 compared to April - August 2020. |
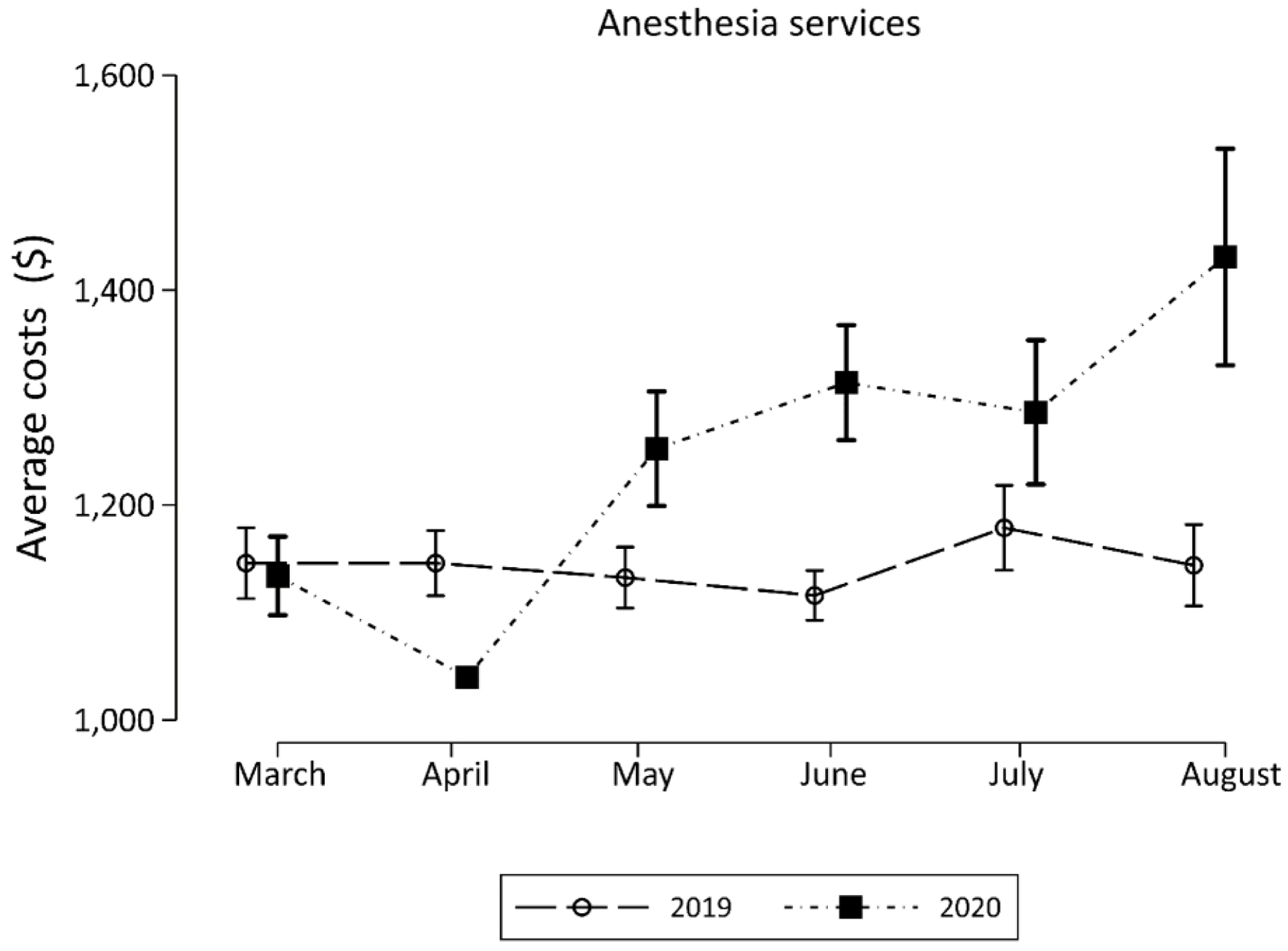 Click for large image | Figure 4. Average cost of anesthesia services during April - August in 2019 compared to April - August 2020. |
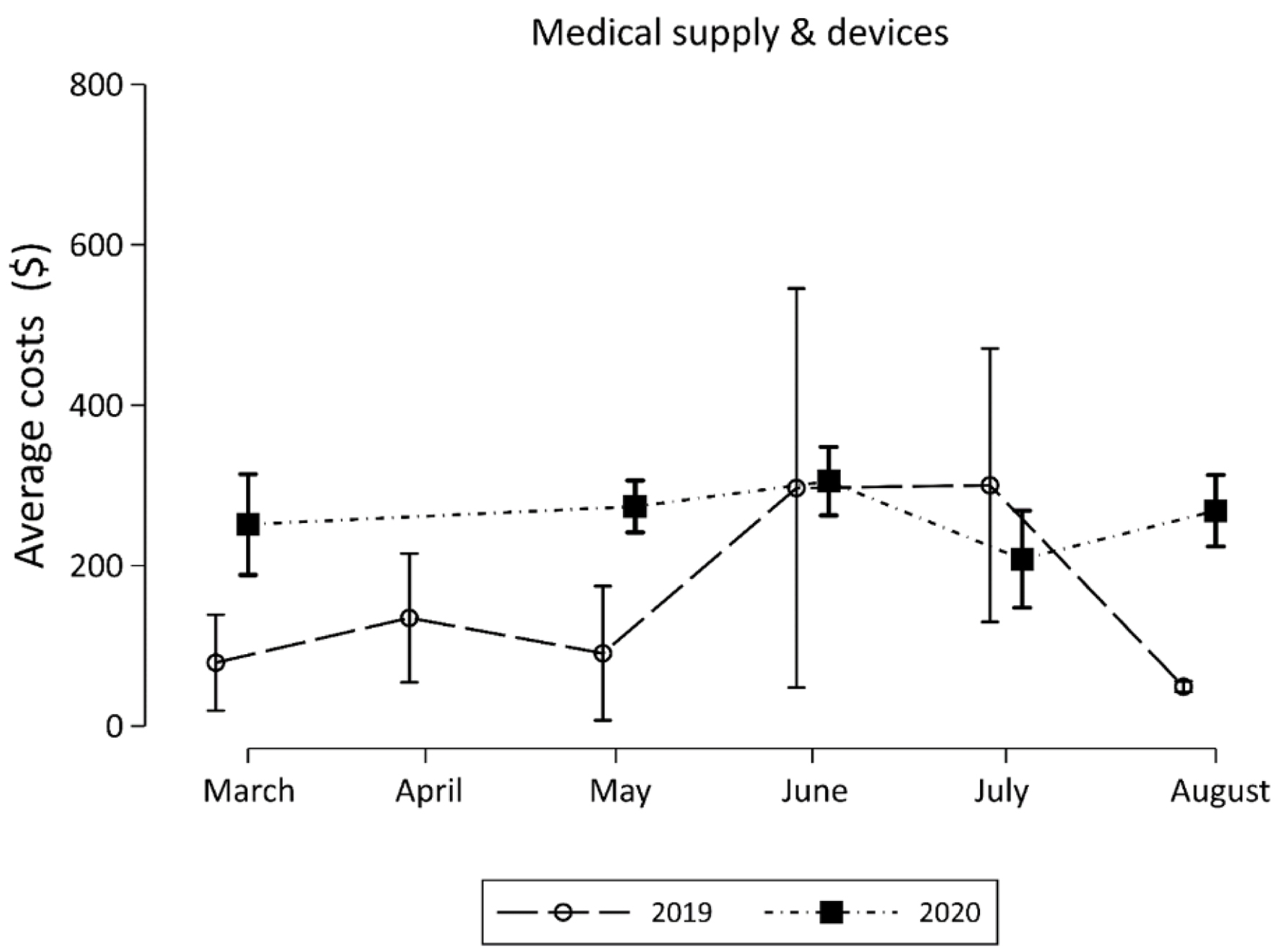 Click for large image | Figure 5. Average cost of medical supplies and devices during April - August in 2019 compared to April - August 2020. |
For medical supplies and devices, 2020 showed an increase in costs in May, which contrasts with the moderate fluctuations seen in 2019. The overall care costs are consistent with this pattern of heightened variability in 2020, with the highest average cost recorded in July, overshadowing the more consistent costs across the months of 2019. Recovery room services mirror the general trend, with costs in 2020 consistently higher than in the previous year, alongside a mid-year rise.
| Discussion | ▴Top |
Our study not only confirms the significant financial impact of the COVID-19 pandemic on free-standing pediatric ambulatory centers, but also serves as a warning regarding the potential consequences of future pandemics without adequate preparation. The unpreparedness of healthcare organizations for a global pandemic resulted in a substantial decline in ambulatory otolaryngology procedures. In many centers, there was not just a decline, but a cessation of elective or non-urgent surgical cases as it was necessary to divert healthcare resources and personnel to care for patients with COVID-19 infections [10, 11]. The restrictions on elective surgery were also implemented in an effort to limit the ongoing spread of the virus. These restrictions were widespread and included pediatric centers even though the number and severity of COVID-19 infections was limited when compared to adult hospitals [11]. These measures were implemented in an effort to free up supplies, equipment, and personnel to care for adult patients if needed. Similar decreases in patient volumes were seen when comparing the pre-COVID-19 era to the COVID-19 period with decreases in emergency department (ED) visits and decreases in overall hospitalizations [11, 12]. As many of these ED visits and hospitalizations were related to acute respiratory illnesses including asthma and bronchiolitis, it was postulated that the overall decrease in respiratory illnesses may have been related to masking and social distancing imperatives. Other patient-care issues related to the pandemic were similarly noted in other hospital-based services including palliative care [13].
Eventual efforts to address the decline in outpatient surgery including increased availability of PPE and other supplies, were hindered by an inadequate supply chain that struggled to provide essential goods in a timely fashion and at reasonable prices. Other areas of care also saw cost increases during this period, with recovery room services, operating room services, and anesthesia services. Our data underscore the significantly higher financial burden placed on both patients and providers during the COVID-19 pandemic.
The economic impact of hospitals suspending elective procedures was significant, with an average loss of $50.7 billion reported by hospitals in the United States from March 1 to June 30, 2020, according to the American Hospital Association [2]. This loss was attributed to a combination of operational restrictions imposed on ambulatory surgical centers, which reduced caseloads while increasing costs, and a notable decline in pediatric patient hospitalization rates during 2020 compared to previous years. Our ambulatory center experienced a 52% decrease in pediatric otolaryngology caseload. In 2020, the total pediatric surgical case numbers for the hospital declined by 21%, marking the first year of decline in a decade of consistent growth. In many centers, the decline in surgical numbers resulted in not only loss of revenue for the hospital, but also impacts on the staff including the reassignment of nursing staff and other highly trained employees to other areas or in lay-offs and salary cuts.
This study, while providing valuable insights with specific cost data, has certain limitations. First, it is a single-center study, which may limit the generalizability of the findings to other pediatric ambulatory centers with different patient demographics or operational structures. Secondly, the study period only covers the first year of the COVID-19 pandemic, and therefore, longer-term impacts on surgical costs and healthcare delivery might not be fully captured. However, when evaluating our current surgical volume during the calendar year 2023, we have noticed a significant rebound with total surgical cases exceeding 43,000 for the first year ever at our hospital and exceeding the previous high of 39,000 the year prior to the pandemic. Additionally, the study focuses solely on elective otolaryngology procedures in pediatric patients, excluding other surgical specialties that might have experienced different trends. We chose this population to maintain a homogenous and manageable data set. The impact of other external factors, such as regional COVID-19 policies and healthcare funding changes, was not accounted for, which might have influenced the study outcomes. During the COVID-19 pandemic, with the restriction of elective surgical procedures, there was a slight change in the demographic population so that the patients during 2020 months were younger and had a higher ASA physical classification. Lastly, the cost analysis did not include indirect costs such as lost wages or transportation expenses for patients and their families, which could have further contributed to the financial burden.
In summary, the COVID-19 pandemic undeniably disrupted the pediatric surgical healthcare system, particularly elective ambulatory surgery settings. Our study illustrates the significant financial impact of the pandemic on pediatric ambulatory centers, emphasizing the need for robust preparedness plans for future health crises. Although we noted cost increases in all four services (anesthesia, operating room, recovery room, and supply and medical devices) totaling an average of $283, 43% of the increase came from supply chain issues (increase of $121) and 33% was due to recovery room costs (increase of $92). The observed reduction in elective surgical procedures and the subsequent increase in care costs underscore the vulnerabilities in healthcare delivery during and after pandemic scenarios. Our findings highlight the importance of strategic resource allocation, including PPE stockpiling and efficient supply chain management, to ensure continuity and quality of care. The lessons learned from this pandemic are invaluable for guiding future policies and practices in healthcare settings, especially in maintaining essential surgical services for pediatric patients. It should also be noted that the impact of the initial COVID-19 pandemic of 2020 continues to have long reaching effects on our healthcare system including ongoing faculty staffing and staff shortages across the perioperative and inpatient setting, equipment and medication supply chain issues, and increased burnout leading to retirement or job changes which further affects staffing shortages [14]. This impact extends far beyond the financial consequences of the pandemic. As healthcare systems continue to evolve in response to global health challenges, our study contributes to a growing body of knowledge that can lead to better preparedness and resilience in the face of the current and future pandemics.
Acknowledgments
Special thanks to Steve Swift and Veronica Weber for providing financial data.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
As a retrospective study, the need for individual written informed consent was waived.
Author Contributions
CR: preparation of initial and subsequent drafts, review of final manuscript; VTR: compliance regulation, data collection and analysis, review of drafts and final manuscript; CM and OON: data analysis, preparation of tables, review of drafts and final manuscript; JDT: study oversight, data collection and analysis, review of drafts and final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Fan VY, Jamison DT, Summers LH. Pandemic risk: how large are the expected losses? Bull World Health Organ. 2018;96(2):129-134.
doi pubmed pmc - Kaye AD, Okeagu CN, Pham AD, Silva RA, Hurley JJ, Arron BL, Sarfraz N, et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293-306.
doi pubmed pmc - Davenport M, Pakarinen MP, Tam P, Laje P, Holcomb GW, 3rd. From the editors: the COVID-19 crisis and its implications for pediatric surgeons. J Pediatr Surg. 2020;55(5):785-788.
doi pubmed pmc - Shukla P, Lee M, Whitman SA, Pine KH. Delay of routine health care during the COVID-19 pandemic: A theoretical model of individuals' risk assessment and decision making. Soc Sci Med. 2022;307:115164.
doi pubmed pmc - El-Boghdadly K, Cook TM, Goodacre T, Kua J, Denmark S, McNally S, Mercer N, et al. Timing of elective surgery and risk assessment after SARS-CoV-2 infection: an update: A multidisciplinary consensus statement on behalf of the Association of Anaesthetists, Centre for Perioperative Care, Federation of Surgical Specialty Associations, Royal College of Anaesthetists, Royal College of Surgeons of England. Anaesthesia. 2022;77(5):580-587.
doi pubmed pmc - COVID Surg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107(11):1440-1449.
doi pubmed pmc - Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6):900-902.
doi pubmed pmc - Miller TR, Radcliff TA. Economic shocks from the Novel COVID-19 pandemic for anesthesiologists and their practices. Anesth Analg. 2020;131(1):112-116.
doi pubmed pmc - U.S. Department of Commerce Bureau of Economic Analysis. National income and product accounts tables. Domestic product and income. https://www.bea.gov/news/2023/gross-domestic-product-second-estimate-corporate-profits-preliminary-estimate-third. Accessed December 4, 2023.
- Wilder JL, Parsons CR, Growdon AS, Toomey SL, Mansbach JM. Pediatric hospitalizations during the COVID-19 pandemic. Pediatrics. 2020;146(6):e2020005983.
doi pubmed - Dexter F, Epstein RH, Rodriguez LI. Decline of pediatric ambulatory surgery cases performed at florida general hospitals between 2010 and 2018: an historical cohort study. Anesth Analg. 2020;131(5):1557-1565.
doi pubmed - Rivera-Sepulveda A, Maul T, Dong K, Crate K, Helman T, Bria C, Martin L, et al. Effect of the COVID-19 pandemic on the pediatric emergency department flow. Disaster Med Public Health Prep. 2021;17:e83.
doi pubmed pmc - Weaver MS, Rosenberg AR, Fry A, Shostrom V, Wiener L. Impact of the coronavirus pandemic on pediatric palliative care team structures, services, and care delivery. J Palliat Med. 2021;24(8):1213-1220.
doi pubmed pmc - Zhong J, Bradford V, Fernandez AM, Infosino A, Soneru CN, Staffa SJ, Raman VT, et al. Continued challenges in pediatric anesthesia during COVID-19 in 2022: An international survey from the pediatric anesthesia COVID-19 collaborative. Paediatr Anaesth. 2023;33(12):1020-1028.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


