| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 16, Number 1, January 2024, pages 24-30
RAM Cannula Versus Bi-Nasal Prongs as Respiratory Device Interfaces in Neonates of Thirty-Two or More Weeks of Gestation With Respiratory Distress: The First “ProRAM” Randomized Trial Report
Manar Al-lawamaa, b, d, Bayan Alaraja, Mahmoud Abu Zahraa, Ibtehal AlHasanata, Heba Habasha, AbdelKareem Alhyaric, Leen Alshajrawic, Salma Jaafrehc
aPediatric Department, School of Medicine, The University of Jordan, Amman, Jordan
bDepartment of Clinical sciences, Yarmouk University, Irbid, Jordan
cSchool of Medicine, The University of Jordan, Amman, Jordan
dCorresponding Author: Manar Al-lawama, Pediatric Department, School of Medicine, The University of Jordan, Amman, Jordan
Manuscript submitted December 1, 2023, accepted December 28, 2023, published online January 10, 2024
Short title: RAM Versus Nasal Prongs in Neonates
doi: https://doi.org/10.14740/jocmr5077
| Abstract | ▴Top |
Background: Using bilateral short nasal prongs as an interface for noninvasive respiratory support is challenging, and it is associated with nasal injury. We aimed to compare RAM cannula with nasal prongs in delivering noninvasive ventilation to newborn infants.
Methods: This is a single-center randomized trial (trial registry: ISRCTN10561691). The setting involves a tertiary neonatal unit with a capacity of 30 beds and more than 13 years of experience in neonatal noninvasive ventilation. We included 50 infants born at ≥ 32 weeks of gestation, who had respiratory distress at birth. We excluded those with major congenital anomalies and those who required intubation in the delivery room. Primary outcomes were intubation rate and use of noninvasive positive-pressure ventilation (NIPPV); other outcomes included air leak and nasal injury rate. The infants were assigned using randomly generated numbers into bi-nasal prong and RAM canula groups in a 1:1 ratio.
Results: Two and four babies in the RAM and prong groups, respectively, were upgraded to NIPPV (P = 0.600). One versus no baby in the RAM vs. prong groups was intubated (P = 1.000). Newborns in the prong group required oxygen support for a longer period (mean duration: 154.6 ± 255.2 h) than those in the RAM group (40.7 ± 72.6 h, P = 0.030). None of the patients in the RAM group had traumatic nasal injury compared to five babies in the prong group (P = 0.050). Four babies in our study developed air leaks, with two in each group.
Conclusions: The use of RAM cannula in delivering noninvasive ventilation to newborns ≥ 32 weeks of age did not affect the noninvasive ventilation failure rate or incidence of air leak. The use was associated with a shorter duration of respiratory support and a reduced risk of nasal septal injury.
Keywords: Neonates; RAM canula; Nasal prongs; Respiratory distress; Noninvasive ventilation
| Introduction | ▴Top |
Respiratory distress in the neonatal period has been described as any sign of breathing difficulty in the newborn. These signs would include tachypnea, grunting, retraction, nasal flaring, and cyanosis [1, 2]. It is a very common entity that occurs in up to 7% of newborn infants, comprising a high percentage of neonatal intensive care unit (NICU) admissions worldwide [3, 4]. Many conditions can present with respiratory symptoms, including transient tachypnea of the newborn, respiratory distress syndrome, congenital pneumonia, meconium aspiration, airway malformations, sepsis, congenital heart disease, and other less common etiologies [5].
Regardless of the cause, respiratory support should be provided to infants using invasive or noninvasive methods of ventilation according to their condition. Noninvasive ventilation has been increasingly used in NICU since the 1970s [6-8]. The use of nasal continuous positive airway pressure (CPAP) and nasal intermittent positive pressure ventilation (NIPPV) to treat different neonatal respiratory diseases has been successful, decreasing the need for intubation and invasive mechanical ventilation and their associated complications [9-12].
Respiratory support to neonates using noninvasive ventilation has traditionally been provided using bilateral short nasal prongs [13]. The use of this interface is challenging and requires significant nursing experience, with nasal septal injury being the most common side effect [12-14]. Several trials have been conducted to investigate the use of a different, more user-friendly, and less traumatizing interface to deliver CPAP to newborns with respiratory distress [15, 16]. The main alternative interface is the RAM canula. It is easier to use, and potentially less traumatic to the nasal septum. However, there is a considerable concern of delivering suboptimal pressure.
In this randomized study, we aimed to compare RAM cannulas with traditional nasal prongs in delivering noninvasive ventilation to newborn infants.
| Materials and Methods | ▴Top |
This study was conducted at Jordan University Hospital NICU, Amman, Jordan, a tertiary care center with a 30-bed capacity. The study protocol was prospectively registered in the Clinical Trial Registry (registration number: ISRCTN10561691). This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The study was approved by the Jordan University Hospital Institutional Review Board (approval number: 10/2021/109/9). No changes were made to the study protocol or the outcomes after registration.
All admitted neonates diagnosed with respiratory distress were included in the study, and neonates with major congenital malformations were excluded. Neonates who were intubated in the delivery room or transferred to our unit from other hospitals were also excluded.
According to the gestational age, the admitted neonates were classified into two groups: born at < 32 weeks or ≥ 32 weeks. Each group was randomized separately. This paper reports the outcomes of infants born at ≥ 32 weeks of gestation. The investigators used random letters generated using an online tool to assign the included infants to each study arm in a 1:1 ratio. Randomized letters were kept in serially numbered sealed opaque envelopes and were used to assign the newborn to bi-nasal prongs or RAM cannula use (Neotech RAM cannula®). The target was to randomize 50 infants. Regarding multifetal gestation, each infant was randomly assigned to one group. Each infant received the same assigned interface for respiratory support until weaned off, or the decision to change the interface was determined by the lead investigator (see the CONSORT flow chart in Figure 1).
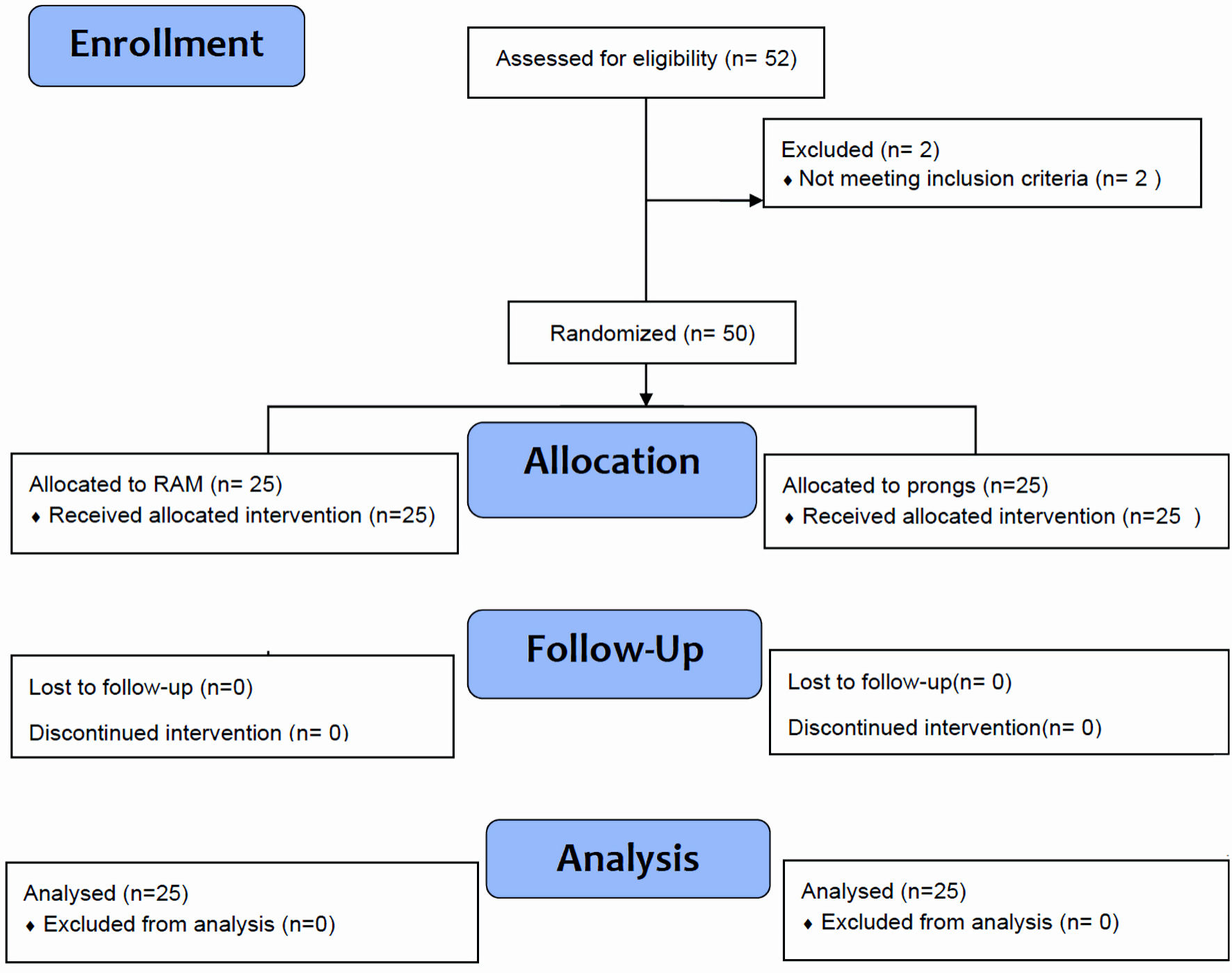 Click for large image | Figure 1. “ProRAM” randomized trial flow diagram for neonates ≥ 32 weeks of gestation. |
All neonates received bubble CPAP with positive end-expiratory pressure (PEEP) of 6 cm H2O as the primary mode of respiratory support. Our institute’s respiratory bundle for CPAP introduction, titration, upgrading, and weaning was followed (Figs. 2, 3). ACORN score was used to determine the severity of respiratory distress [17].
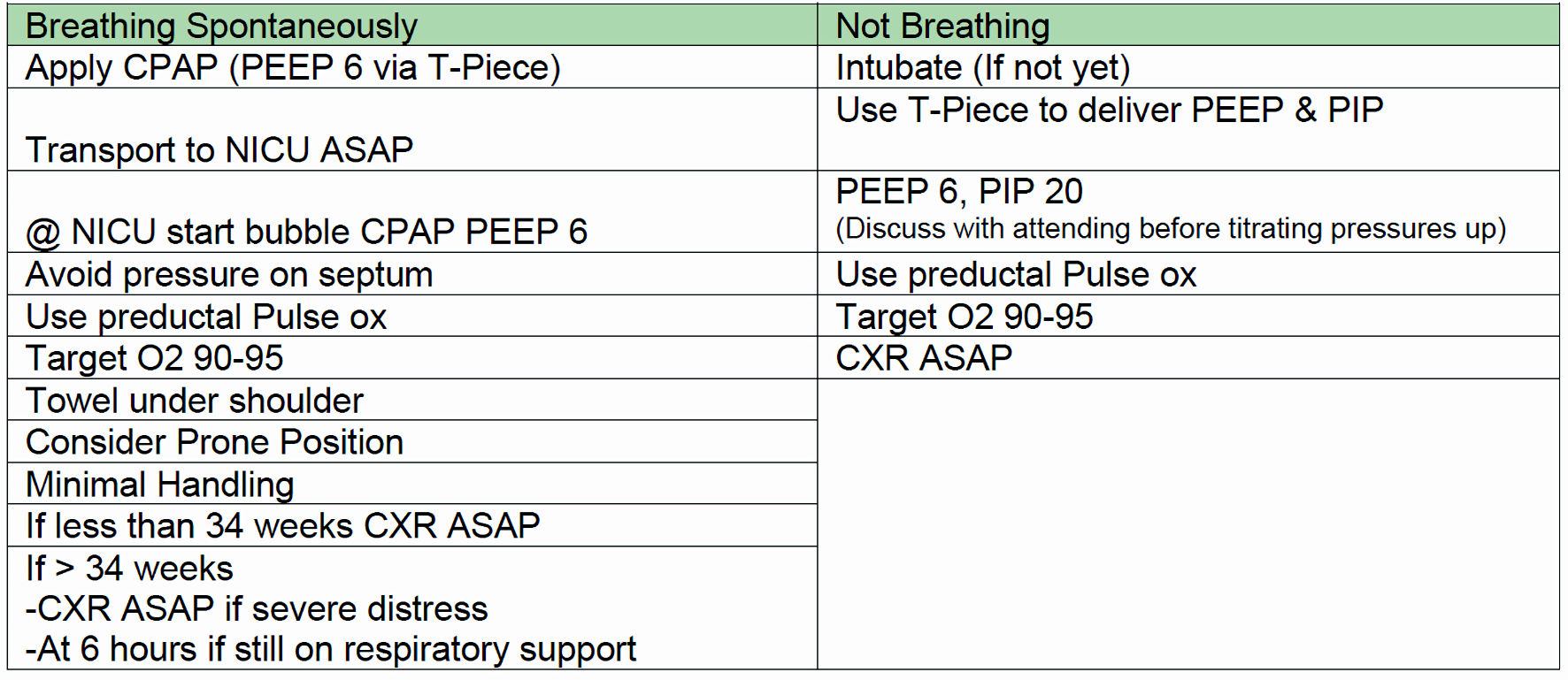 Click for large image | Figure 2. Post resuscitation respiratory care bundle. PEEP: positive end-expiratory pressure; ASAP: as soon as possible; CPAP: continuous positive airway pressure; NICU: neonatal intensive care unit; CXR: chest X-ray; PIP: peak inspiratory pressure. |
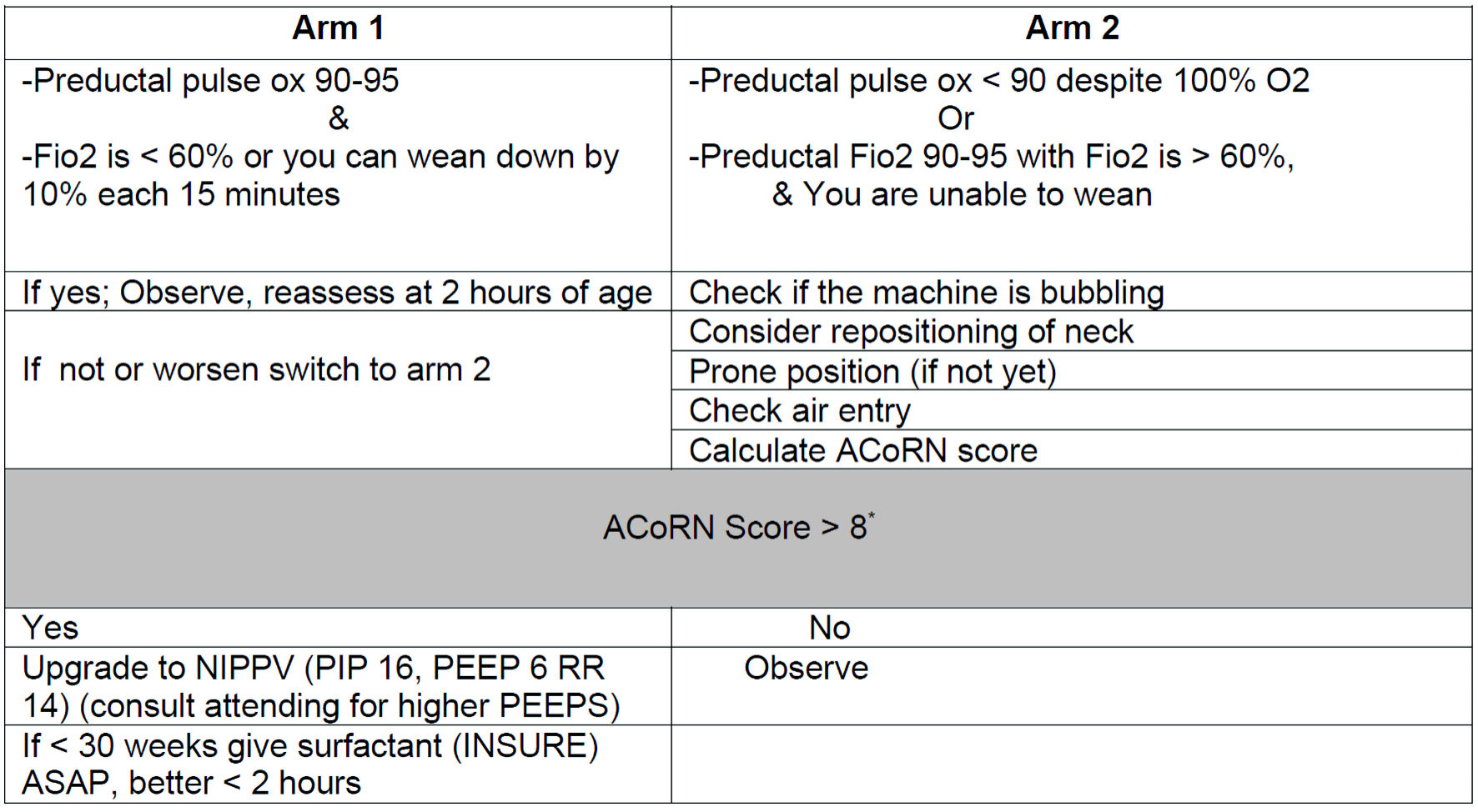 Click for large image | Figure 3. CPAP care bundle of neonates with respiratory distress. CPAP: continuous positive airway pressure; FiO2: fraction of inspired oxygen. |
The size of the interface was selected according to the manufacturer’s recommendations. The short nasal prongs were fixed with gentle skin tape to reduce leaks around the nostrils and produce proper CPAP pressures. Interface fixation and stability in the infant nostrils were monitored by bedside nurses.
The data, which were collected prospectively, included maternal and neonatal demographics including risk factors, initial neonatal presenting respiratory symptoms and signs, and the clinical course, including different management interventions and complications. Respiratory rate at admission was stratified into the following categories according to the severity of tachypnea: respiratory rate ≤ 60, 61 - 70, 71 - 80, > 80. The neonatal nasal septum was observed daily by a senior neonatologist and staged according to the degree of injury as follows: I: hyperemia, and hemorrhage; II: disruption of skin integrity and superficial ulceration; and III: nasal deformity. The most severe state was recorded.
We aimed to compare the use of RAM cannula to the traditional nasal prongs in delivering noninvasive ventilation to newborns with respiratory distress, with the need for respiratory support escalation to NIPPV, mechanical ventilation, or other measures such as surfactant administration, as our primary outcome along with the extent of nasal injury at each interface.
Statistical analysis
The sample size was calculated based on our unit’s CPAP failure rate (6%) [12], and an expected failure rate of 40% when using the RAM canula. This was based on theoretical difficulty of building enough pressure while using an interface with a leak. A sample size of 23 per group was required at 5% alpha error and 80% power.
Microsoft Excel 2010 was used to analyze the results. Continuous variables are presented as mean and standard deviation. Categorical variables are presented as numbers and percentages. Categorical variables were compared using the two-tailed Chi-square test (two-tailed). Continuous variables were compared using Student’s t-test. Statistical significance was set at P < 0.05.
| Results | ▴Top |
Fifty neonates born at ≥ 32 weeks of gestation and admitted to our NICU with respiratory distress after birth were included. The neonates were randomized into two groups according to the allocated nasal airway interface: RAM and prong groups. The neonates in both groups had no significant differences in mean gestational ages, birth weights, antenatal maternal illnesses, and infectious risk factors (Table 1).
 Click to view | Table 1. Demographic and Perinatal Characteristics of Newborn Randomized to Both Study Groups |
All babies were started on bubble CPAP as an initial mode of respiratory support. Neonates in both groups were almost similar in their respiratory rates at admission, with a mean of 61 breaths/min, as well as similar initial fraction of inspired oxygen (FiO2) requirement with a mean of 23% in both groups (Table 2). Two babies in the RAM group and four in the prong group were upgraded to NIPPV due to worsening respiratory status (P = 0.667). Only one infant in the prong group was intubated (P = 1.000). Most newborns in both groups were diagnosed with transient tachypnea (68% vs. 64% in RAM and prong groups, respectively). Newborns in the prong group required oxygen support for a longer period (mean duration of support,154.6 ± 255.2 h) than those in the RAM group (40.7 ± 72.6 h, P = 0.030).
 Click to view | Table 2. Respiratory Characteristics and Clinical Outcome for Included Infants |
Of the babies who received RAM cannulas, none had traumatic nasal injury compared to five babies in the prong group who had a nasal injury value of 0.050. Only four babies in our study developed air leak syndrome, with two cases of pneumomediastinum in the RAM group and one case of pneumothorax and pneumomediastinum in the prong group (P = 1.000). None of the infants in either group died before hospital discharge (Table 2).
| Discussion | ▴Top |
Respiratory distress is one of the major indications of newborn admission to intensive care units [18]. Noninvasive ventilation remains the main source of respiratory support in such neonates [19]. Choosing the most practical nasal interface that delivers oxygen to babies with the highest efficacy and lowest complications remains controversial [20]. In our institute, prongs are the most used interfaces. However, the availability of RAM cannulas has raised the question of their comparability to nasal prongs: whether they deliver the same support without adding more risks, or even whether they decrease some of the commonly faced complications.
Both groups of neonates who were randomly assigned to receive either a nasal prong or RAM cannula as a respiratory support interface upon admission, had similar demographic and perinatal characteristics (Table 1), with comparable mean gestational age, mean birth weight, and similar rates of maternal infections, antenatal steroids, and Apgar scores. The included infants in both groups had similar severity of respiratory distress, evident by similar rates of tachypnea and FiO2 needs on admission (Table 1). One major concern about using the RAM cannula as a respiratory interface is the suboptimal pressure delivery, and consequently, increases in the CPAP failure rate. The basis of this concern was an in vitro study that failed to achieve a set CPAP level with the RAM cannula in comparison with other CPAP interfaces [21]. This study is useful in demonstrating the physics and dynamics of CPAP interfaces but does not necessarily report the clinical implications. Regarding clinical studies, results vary in demonstrating the clinical differences between RAM cannulas and bi-nasal prongs, with most of these studies exploring these differences in premature neonates. Drescher et al demonstrated a need for high settings in the RAM cannula group compared to the control group, but no significant difference in invasive ventilation rates. However, there was a significant reduction in the duration of respiratory support and a trend towards reduction of bronchopulmonary dysplasia in the RAM group [22]. In a randomized controlled trial by Gokce et al, more neonates on RAM cannula required invasive ventilation in the first 72 h and surfactant administration in comparison to bi-nasal prongs. However, there was no increase in the duration of respiratory support or bronchopulmonary dysplasia [23]. Moreover, Hochwald et al showed the noninferiority of the RAM cannula compared to the short nasal prong in providing intermittent positive pressure ventilation in preterm infants born between 24 weeks and 33 weeks and 6 days’ gestation [24]. Studies that include late preterm and term infants are lacking in literature.
In our study, requiring NIPPV or mechanical ventilation was considered failure of the treatment in both groups. Adding more pressure to the baseline CPAP is potentially more injurious to the lungs and indicates either a more serious respiratory illness or failure to achieve the intended CAPAP pressure. the RAM cannula showed noninferiority compared to the short nasal prong, as there was no significant difference between the two groups in the need to upgrade the respiratory support or further treatments (Table 2). Adherence to strict respiratory care bundles may also be attributed to this result.
In contrast, our groups showed a significant difference in the mean duration of oxygen support despite the similarities between the final respiratory distress diagnoses. The mean duration of support in the prong group was 154.6 h compared to 40.7 h in the RAM group (P < 0.05). This was similar to the findings of Drescher et al, who demonstrated reduced days of noninvasive respiratory support when using the RAM system [22]. In our study, the respiratory support duration difference was mainly due to the continued need of oxygen support in the four babies in the prong group for more than 1 week compared to those in the RAM group, during which the allocated nasal interface was kept the same.
This prolonged need for oxygen therapy was independent of the initial respiratory diagnosis and was mainly caused by persistent desaturation, leading to weaning failure in these neonates. All four infants developed nasal septal injury during their stay. Nasal septal injury, causing nasal blockage and discomfort, can be attributed to the persistent need for respiratory support. Furthermore, there was no difference in the rate of air leak syndrome between the two groups. Some previous studies showed a similar incidence of air leak [23], and others showed a higher but insignificant incidence in the RAM group [20].
This study showed that the rates of all forms of nasal injuries were lower in the RAM group than in the prong group, as none of the neonates who were randomized to the RAM cannula group developed nasal injury. Despite the study outcome P value of 0.05, it was considered significant because the randomized sample was relatively small, and all nasal injuries occurred in the prong group. A reduced risk of nasal injury has also been reported in previous studies [22, 24]. In contrast, Gokce et al studied the efficacy of RAM and prong as a means of noninvasive ventilation interface and found no difference in the incidence of nasal injury or other morbidities [23]. To our knowledge, no previous studies have been conducted to demonstrate this difference between the late preterm and full-term neonates, which comprises of most NICU admissions at our institute. Ten percent of our studied neonates developed nasal septal injury, which, in general, has a low risk of nasal injuries compared to premature and very low birth weight [14, 25]. This reduced nasal injury in the RAM cannula group could be attributed to the softness of the device, ease of fixation and stabilization, simplicity of nursing care, and better access to the neonate.
The use of RAM cannulas in delivering noninvasive ventilation to newborns ≥ 32 weeks did not affect noninvasive ventilation failure rates, and there was no significant difference in the incidence of air leak and other complications. This was associated with a shorter duration of O2 support and a reduced risk of nasal septal injury. RAM cannulas can be used as the primary method for delivering noninvasive ventilation to neonates.
Acknowledgments
The authors acknowledge the efforts of our unit nursing staff in providing neonatal care.
Financial Disclosure
This study did not receive any funding.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written consent was not taken from the parents since nasal CPAP is the standard of care and our nurses use both interfaces on babies interchangeably before the study, and the parents were informed of the choice of treatment upon admission, and they approved it.
Author Contributions
MA: conceptualization, design, supervising, analysis, and writing. BA: supervising and conducting, analysis, writing, approving final manuscript. MAZ, IA, HH, AA, LA, and SJ: analysis, writing, and approving final manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Hermansen CL, Mahajan A. Newborn respiratory distress. Am Fam Physician. 2015;92(11):994-1002.
pubmed - Mathai SS, Raju U, Kanitkar M. Management of respiratory distress in the newborn. Med J Armed Forces India. 2007;63(3):269-272.
doi pubmed pmc - Edwards MO, Kotecha SJ, Kotecha S. Respiratory distress of the term newborn infant. Paediatr Respir Rev. 2013;14(1):29-36.
doi pubmed - Al-Momani MM. Admission patterns and risk factors linked with neonatal mortality: A hospital-based retrospective study. Pak J Med Sci. 2020;36(6):1371-1376.
doi pubmed pmc - Liszewski MC, Stanescu AL, Phillips GS, Lee EY. Respiratory distress in neonates: underlying causes and current imaging assessment. Radiol Clin North Am. 2017;55(4):629-644.
doi pubmed - Anne RP, Murki S. Noninvasive respiratory support in neonates: a review of current evidence and practices. Indian J Pediatr. 2021;88(7):670-678.
doi pubmed pmc - Gregory GA, Kitterman JA, Phibbs RH, Tooley WH, Hamilton WK. Treatment of the idiopathic respiratory-distress syndrome with continuous positive airway pressure. N Engl J Med. 1971;284(24):1333-1340.
doi pubmed - Rhodes PG, Hall RT. Continuous positive airway pressure delivered by face mask in infants with the idiopathic respiratory distress syndrome: a controlled study. Pediatrics. 1973;52(1):1-5.
pubmed - Oktem A, Yigit S, Celik HT, Yurdakok M. Comparison of four different non-invasive respiratory support techniques as primary respiratory support in preterm infants. Turk J Pediatr. 2021;63(1):23-30.
doi pubmed - Behnke J, Lemyre B, Czernik C, Zimmer KP, Ehrhardt H, Waitz M. Non-invasive ventilation in neonatology. Dtsch Arztebl Int. 2019;116(11):177-183.
doi pubmed pmc - Fathi O, Schlegel AB, Shepherd EG. Non-Invasive Ventilation of the Neonate. Noninvasive Ventilation in Medicine. IntechOpen, Rijeka. 2017.
- Al-Lawama M, Alkhatib H, Wakileh Z, Elqaisi R, AlMassad G, Badran E, Hartman T. Bubble CPAP therapy for neonatal respiratory distress in level III neonatal unit in Amman, Jordan: a prospective observational study. Int J Gen Med. 2019;12:25-30.
doi pubmed pmc - Ribeiro DFC, Barros FS, Fernandes BL, Nakato AM, Nohama P. Nasal prongs: risks, injuries incidence and preventive approaches associated with their use in newborns. J Multidiscip Healthc. 2020;13:527-537.
doi pubmed pmc - Imbulana DI, Manley BJ, Dawson JA, Davis PG, Owen LS. Nasal injury in preterm infants receiving non-invasive respiratory support: a systematic review. Arch Dis Child Fetal Neonatal Ed. 2018;103(1):F29-F35.
doi pubmed - Singh N, McNally MJ, Darnall RA. Does the RAM cannula provide continuous positive airway pressure as effectively as the Hudson prongs in preterm neonates? Am J Perinatol. 2019;36(8):849-854.
doi pubmed - Sharma D, Murki S, Maram S, Pratap T, Kiran S, Venkateshwarlu V, Dinesh P, et al. Comparison of delivered distending pressures in the oropharynx in preterm infant on bubble CPAP and on three different nasal interfaces. Pediatr Pulmonol. 2020;55(7):1631-1639.
doi pubmed - Downes JJ, Vidyasagar D, Boggs TR, Jr., Morrow GM, 3rd. Respiratory distress syndrome of newborn infants. I. New clinical scoring system (RDS score) with acid—base and blood-gas correlations. Clin Pediatr (Phila). 1970;9(6):325-331.
doi pubmed - Reuter S, Moser C, Baack M. Respiratory distress in the newborn. Pediatr Rev. 2014;35(10):417-428.
doi pubmed pmc - Mahmoud RA, Roehr CC, Schmalisch G. Current methods of non-invasive ventilatory support for neonates. Paediatr Respir Rev. 2011;12(3):196-205.
doi pubmed - Maram S, Murki S, Nayyar S, Kadam S, Oleti TP, Anne RP, Deshobhotla S, et al. RAM cannula with Cannulaide versus Hudson prongs for delivery of nasal continuous positive airway pressure in preterm infants: an RCT. Sci Rep. 2021;11(1):23527.
doi pubmed pmc - Gerdes JS, Sivieri EM, Abbasi S. Factors influencing delivered mean airway pressure during nasal CPAP with the RAM cannula. Pediatr Pulmonol. 2016;51(1):60-69.
doi pubmed - Drescher GS, Hughes CW. Comparison of interfaces for the delivery of noninvasive respiratory support to low birthweight infants. Respir Care. 2018;63(10):1197-1206.
doi pubmed - Gokce IK, Kaya H, Ozdemir R. A randomized trial comparing the short binasal prong to the RAM cannula for noninvasive ventilation support of preterm infants with respiratory distress syndrome. J Matern Fetal Neonatal Med. 2021;34(12):1868-1874.
doi pubmed - Hochwald O, Riskin A, Borenstein-Levin L, Shoris I, Dinur GP, Said W, Jubran H, et al. Cannula with long and narrow tubing vs short binasal prongs for noninvasive ventilation in preterm infants: noninferiority randomized clinical trial. JAMA Pediatr. 2021;175(1):36-43.
doi pubmed pmc - Buettiker V, Hug MI, Baenziger O, Meyer C, Frey B. Advantages and disadvantages of different nasal CPAP systems in newborns. Intensive Care Med. 2004;30(5):926-930.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


