| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 6, June 2023, pages 321-327
Nutritional Interpretation of Hospital Diets for Elderly Patients With Chronic Diseases and Analysis of Factors Influencing Actual Intakes
Yasuko Fukudaa, b, e, Mikako Ochic, Ryouko Kanazawaa, Hiromu Nakajimad, Keisuke Fukuoa, b, Masanobu Nakaic
aDepartment of Food Science and Nutrition, School of Human Environmental Science, Mukogawa Women’s University, Ikebiraki-cho, Nishinomiya, Hyogo 663-8558, Japan
bResearch Institute for Nutrition Science, Mukogawa Women’s University, Ikebiraki-cho, Nishinomiya, Hyogo 663-8558, Japan
cNakai Hospital, Nada-ku, Kobe, Hyogo 657-0833, Japan
dDepartment of Endocrinology and Metabolism/Clinical Laboratory, Osaka International Cancer Institute, Chuo-ku, Osaka, Osaka 541-8567, Japan
eCorresponding Author: Yasuko Fukuda, Department of Food Science and Nutrition, School of Human Environmental Science, Mukogawa Women’s University, Ikebiraki-cho, Nishinomiya, Hyogo 663-8558, Japan
Manuscript submitted May 22, 2023, accepted June 23, 2023, published online June 29, 2023
Short title: Gender Impact on Nutritional Interpretation
doi: https://doi.org/10.14740/jocmr4961
| Abstract | ▴Top |
Background: The provision of hospital meals is considered a therapeutic intervention, and a therapeutic diet consisting of a post-discharge meal sample is provided. For elderly patients who require long-term care, it is important to determine the significance of nutrition by taking into account hospital meals, including therapeutic meals for conditions such as diabetes. Therefore, it is important to identify the factors that influence this judgment. This study aimed to investigate the difference between the expected nutritional intake via nutritional interpretation and actual nutritional intake.
Methods: The study included 51 geriatric patients (77.7 ± 9.5 years; 36 males and 15 females) who could eat meals independently. The participants completed a dietary survey to determine the perceived nutritional intake obtained from hospital meal contents. Additionally, we investigated the amount of hospital meal leftovers from the medical records and the amount of nutrients from the menus to calculate the actual nutritional intake. We calculated the amount of calories, protein concentration, and non-protein/nitrogen ratio from the perceived and actual nutritional intake values. We then calculated the cosine similarity and conducted a qualitative analysis of factorial units to examine similarities between perceived and actual intake.
Results: Among factors that constituted the large cosine similarity group (gender, age, etc.), gender was found as a particularly significant factor, with a high number of female patients (P = 0.014).
Conclusions: Gender was found to influence the appropriate interpretation of the significance of hospital meals. The perception of such meals as samples for post-discharge dietary practice was more significant among female patients. This demonstrated that in elderly patients, it is important to consider gender differences when providing diet and convalescence guidance.
Keywords: Geriatric patients; Hospital meals; Perceived; Actual; Cosine similarity; Non-protein calorie/nitrogen ratio
| Introduction | ▴Top |
Hospital meals promote disease healing and recovery by improving/maintaining the patient’s condition and nutritional status. They can also be considered as a sample for post-hospital diet therapy. However, if patients’ depth of interest in the ingredients, quantities, and cooking methods used for hospital meals is insufficient, the role and function of hospital meals cannot be properly applied.
The food perception of elderly individuals is influenced by the way ingredients are cut, the state of the broth, and the color of the plate on which the food is served [1]. In addition, patients with chronic illnesses such as chronic heart disease, chronic obstructive pulmonary disease, bronchial asthma, and diabetes are instructed that diet therapy during hospitalization is part of their treatment modalities. Therefore, to strictly follow a therapeutic diet may become a mental burden in some cases. The level of such burden is also significantly affected by social factors such as X, Y and Z [2]. It is assumed that the perception level varies, such as in the extent to which hospital meals are considered important and the extent to which hospital meals are deemed beneficial for treatment. We considered that understanding the factors contributing to disparities in the perception of hospitalized food as a whole, including both regular and therapeutic food, and actual intake would be crucial and beneficial in providing nutritional support following hospital discharge.
The non-protein calorie/nitrogen (NPC/N) ratio, the balance of energy and protein, is considered to promote protein synthesis in the body. The NPC/N ratio indicates the amount of carbohydrates and protein that should be consumed per protein intake to maximize protein utilization [3]. In previous studies, we have shown that differences in nutrient intake from breakfast/lunch/dinner, which is calculated from nutritional intake obtained through hospital meals consumed by elderly patients might affect albumin (Alb) synthesis in the liver [4]. We also found that the NPC/N ratio in elderly patients’ nutritional intake may influence their discharge locations [5]. Additionally, we have demonstrated that to improve Alb levels at discharge, it might be useful to increase the proportion of carbohydrates within the permitted range in the NPC/N ratio of breakfast and improve non-protein energy intake obtained from breakfast [6]. Therefore, the NPC/N ratio can be applied to evaluate the nutrient composition of meals in this study.
The cosine similarity method is used to evaluate the similarity of documents in natural language processing. Using the vectors formed by the documents and the angles made by the vectors, the similarity of two documents can be assessed [7, 8].
In this study, we focused to examine the difference between the expected nutritional intake by nutritional interpretation and actual nutritional intake. To create a nutritional-support measure based on the understanding of hospital meals provided to elderly patients that can be used in providing discharge support of elderly patients, we calculated the cosine similarity of the amount of protein, energy, and the NPC/N ratio. We analyzed the level of contribution of gender, age, type of hospital meal (regular diet or therapeutic diet), body mass index (BMI), Alb levels, and intake according to staple food and side dish to the similarity. Then, we conducted an analysis of factors that caused a discrepancy between perceived and actual intake values obtained from hospital meals using the same-direction vector group.
| Materials and Methods | ▴Top |
Participants
The target hospital was a small (48-bed) hospital providing care-mix medical care in Nada Ward, Kobe, Hyogo. Participants were chosen in a consecutive and nondiscriminatory manner from hospitalized patients. The participant sample included 51 geriatric patients (aged 77.7 ± 9.5 years; quartile: 68.5 - 85.0 years; 36 males and 15 females) who admitted to the target hospital from August 2021 to March 2023. The participants had a chronic illness, who could independently eat hospital meals, and for whom dietary intake information could be obtained 1 month after hospitalization.
There was no double counting. However, patients with cognitive impairment and those who were deemed inappropriate by the hospital director were excluded (Fig. 1).
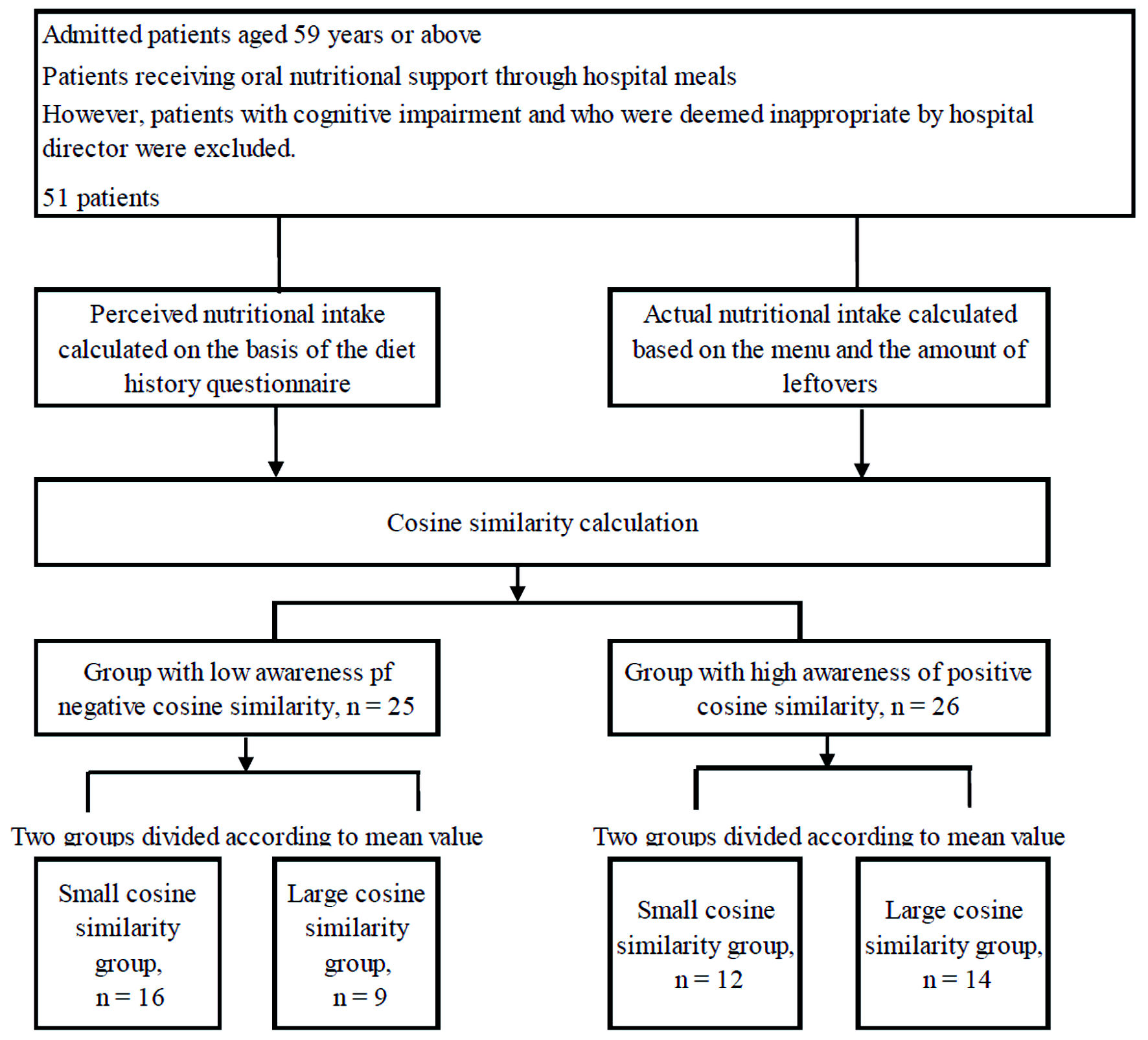 Click for large image | Figure 1. Scheme for subject recruitment and study workflow. |
Methods
Perceived nutritional intake
Perceived nutritional intake was defined as the expected intake based on the understanding of hospital meals. We conducted a dietary survey to determine the perceived nutritional intake. The expected value estimated from participant responses was considered the perceived nutritional intake. Using the brief-type self-administered diet history questionnaire (BDHQ), we conducted dietary surveys 4 weeks after hospitalization. However, at less than 4 weeks after admission, participants were advised to respond with regard to meals during hospitalization after admission to our hospital. The dietary intakes of individual patients were surveyed. The participants were asked to provide self-recorded responses to the questionnaire. From the nutritional amounts obtained from the BDHQ, we calculated the amount of calories, protein concentration, and NPC/N ratio, which we utilized after normalization.
Actual nutritional intake
The actual nutritional intake was calculated based on the amount of leftovers and diet recipe. Then, we conducted a retrospective search of medical records. In addition to the amount of leftovers at breakfast, lunch, and dinner, as well as the staple food and side dishes for 4 weeks after hospitalization, the survey items included basic attributes, comorbidities, type of hospital meal, and serum Alb levels at admission. BMI was calculated using height and weight. Based on the actual nutritional intake, we calculated the amount of calories, protein concentration, and NPC/N, which we used after normalization.
Cosine similarity
Cosine similarity was calculated using two vectors: one obtained from the perceived nutritional intake and one from the actual nutritional intake [9-11]. The calculation formula is as follows:
a: Based on the calculation of the perceived nutritional intake, we obtained the normalized amount of calories, protein concentration, and NPC/N ratio; b: Based on the calculation of the actual nutritional intake, we obtained the normalized amount of calories, protein concentration, and NPC/N ratio (n = 51).
Analysis
Analysis included: 1) To determine the amount of calories, protein concentration, and NPC/N ratio of the 51 participants before normalization, the relationship between perceived and actual nutritional intake were examined. 2) The relationship between cosine similarity and gender, age, type of hospital meal (normal diet or special therapeutic diet), BMI, Alb levels, and intake of staple foods and side dishes was investigated. By definition, cosine similarity expression ranges from -1 to 1. A value of 1 indicates vectors of the same direction, i.e., completely similar, whereas a value of -1 indicates vectors of opposite directions, i.e., completely dissimilar. Therefore, we subsequently analyzed the data divided into two groups: the opposite-direction vector group and the same-direction vector group. 3) After dividing the two groups, including the opposite-direction vector group (opposite-direction vector group: cosine similarity ≤ -0.1) and the same-direction vector group (same-direction vector group: cosine similarity ≥ 0.1), in the small cosine similarity group and the large cosine similarity group of each group, based on the mean cosine similarity, we compared gender, age, type of hospital meal (normal diet or special therapeutic diet), BMI, Alb levels, and the amount of intake according to the staple food and side dishes.
Analyses were performed using the Statistical Analysis System (SAS) version 9.4 (SAS Institute Inc., Cary, NC, USA), and a P value of less than 0.05 was defined as statistically significant.
Ethical considerations
The Research Ethics Committee of Mukogawa Women’s University and Junior College approved this study on May 28, 2022 (Approval No. 22-17). The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
We observed the following points from the analysis: 1) No correlation was found between perceived and actual nutritional intake (Table 1). 2) There was no relationship between the cosine similarity and each item for the 51 participants (Table 2). 3) Table 3 presents the results of the high awareness and low awareness groups examined with each group divided based on the mean cosine similarity.
 Click to view | Table 1. Demographics |
 Click to view | Table 2. The Relationship Between Cosine Similarity and Each Item |
 Click to view | Table 3. Comparison Between the High Awareness and the Low Awareness Group: Cosine Similarity Was Used to Stratify Each Group Based on the Mean Cosine Similarity |
Furthermore, during the survey period, there was no change from a normal diet to a therapeutic diet for any patient, and hospital meals containing a consistent amount of nutrition were continuously provided. The mean staple food and side dish intake over 1 month were 96±10%, and 95±12%, respectively in the 15 patients consuming a normal diet, 89±20%, and 94±8% respectively in the 15 patients consuming a diet for heart disease and hypertension, and 92±13%, and 93±11%, respectively in the 10 patients consuming a diabetic diet. Moreover, on hospital meal slips, the ordered amount of dietary salt was 6.5 g/day for a normal diet, less than 6 g/day for a diet for heart disease and hypertension, and 6.5 g/day for a diabetic diet. Regarding potassium management, in all meal types, not a single patient was deprived of fresh fruit and vegetables and ordered to have water intake restricted. Regarding energy management, 1,600 kcal/day for a normal diet, and 1,600 kcal/day for a diabetic diet were ordered. For other diet types, approximately 1,600 kcal/day were ordered. Furthermore, we surveyed the amount of meal intake for each individual. For example, the staple food changed from boiled rice to rice porridge, or bread in accordance with the patient’s appetite, and changes in the nutritional amount were reflected in the actual nutritional intake. Therefore, it is unlikely that the amount of meal intake of each individual patient was affected by the difference in the meal type and nutritional restrictions.
| Discussion | ▴Top |
In the present study, we examined the similarity between elderly patients’ perceived and actual nutritional intake values calculated from hospital meals to develop nutritional-support measures that can be used for discharge support of elderly patients. The amount of calories, protein concentration, and NPC/N ratio were normalized and used for the vector data. The NPC/N ratio was used because it can be used to assess the nutrient composition of meals. Then, we calculated the cosine similarity to determine how similar the directions of the two vectors were. The cosine similarity value was normalized to -1; therefore, in the 26 patients with vectors pointing in the same direction, we further analyzed the factors that cause a difference between the perceived and actual nutritional intake values (Fig. 1). The results indicated that gender was the factor of interest. The similarity between perceived and actual nutritional intake values was higher in women, and women had an increased awareness of hospital meals as sample meals after discharge.
Furthermore, it is very interesting that in the low awareness group, even when the cosine similarity value was negative, there were significantly more patients eating a therapeutic diet who had high cosine similarity than patients eating a normal diet. It is plausible that this might be affected by previous empirical results.
In the present study, female patients exhibited higher similarities between perceived and actual nutritional intake. This was assumed to involve the relationship between knowledge and skill between female and male patients in terms of meals. In the generation of elderly patients included in the present study, men worked outside, whereas women were devoted to housework and cooking. Therefore, women have greater knowledge and interests of meal composition and the nutritional value of meals, as well as higher cooking skills. Furthermore, among the participants of the present study, women place a higher priority on meal awareness. According to the results of a nationwide survey of 2,248 healthy adults in Japan, women place more emphasis on all criteria for food selection than men [12]. Moreover, it has been reported that as compared to men, women have more nutrition knowledge and are more adept at cooking techniques for all meals [12]. It has been found that there was a completely inverse relationship between men and women, i.e., for men, the greater the age, the lower the level of skill in cooking techniques for all meals, whereas, for women, the greater the age, the higher the level of skill in cooking techniques for all meals [12]. In the present study, there were significantly more women than men in the large cosine similarity group (the group with high similarity), which is similar to the distribution of study population in previous studies showing female patients have more knowledge of all meals and a higher level of skill.
On the contrary, it was assumed that differences between men and women, such as their sense of values, needs, obstacles, and nutrition and meal concerns, caused a discrepancy in the level of similarity. For example, in patients with diabetes mellitus, the three main types of treatment include diet therapy, exercise therapy, and pharmacotherapy. Although it is important to continuously manage these treatments independently, treatment compliance differs due to gender differences [13]. According to the results of a qualitative analysis of the self-management experiences of men and women with type 2 diabetes, it is important to consider gender differences while providing support for diabetes treatment. Men focused on the practical aspects of self-monitoring of blood glucose (SMBG) and attempted various aspects of management to reduce drug dependency, whereas women focused on the emotional elements of SMBG [14]. While men with type 2 diabetes have lower expectations for the benefits of self-management than women, it is emphasized that men value assistance from friends and family [15]. Diet therapy is an important part of diabetes care, and it is important to address it in a gender-sensitive manner. In the present study participants, it was found that gender differences caused a difference between perceived and actual nutritional intake obtained through hospital meals. Therefore, based on gender differences, it was suggested that it is advantageous to proceed with nutritional support, taking both emotional and practical aspects into account. Female patients with a higher similarity between perceived and actual nutritional intake may consider hospital meals as instructional aids for diet therapy after discharge. In contrast, no similarity was found between perceived and actual intake in male patients, suggesting that male patients eat independently. Accordingly, it was determined that for male patients, repeated nutritional guidance within the permissible range using hospital meals as instructional aids would be necessary and beneficial.
Limitations of the study
The limitations of this study are as follows: it is a retrospective study rather than an interventional study; the participants are limited; and the number of cases is small as geriatric patients admitted to a small, local hospital were targeted. However, for questions regarding hospital meals and menus in everyday nutrition rounds, female patients had better perception compared with male patients, which helped us to proceed with this study. Therefore, there are limitations in the interpretation of the results. The results should not be generalized because of the insufficient sample size. Nevertheless, the current result provides an excellent opportunity to validate this issue through a large-scale study in the future.
Conclusions
We calculated the cosine similarity between the perceived amount of nutritional intake and the actual amount of nutritional intake obtained from hospital meals in elderly patients, focusing on the amount of calories, protein concentration, and NPC/N ratio. We found that the similarity and discrepancy between the two amounts were influenced by gender differences. There would be differences in values, knowledge, and needs regarding diet due to gender differences. Therefore, it is recommended that nutritional support might be considered from both practical and emotional aspects, taking gender differences into account.
Acknowledgments
We would like to express our deep gratitude to the patients admitted to the Nakai Hospital who provided their consent to participate in this study.
Financial Disclosure
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
We have obtained informed consent for publication from all participants.
Author Contributions
Yasuko Fukuda: all processes, including data collection, analysis, and manuscript writing. Mikako Ochi and Ryoko Kanazawa: medical chart survey. Hiromu Nakajima, Keisuke Fukuo, and Masanobu Nakai: final proofreading of the manuscript.
Data Availability
Any inquiries regarding the availability of supporting data for this study should be directed to the corresponding author.
Abbreviations
Alb: albumin; NPC/N: non-protein calorie/nitrogen ratio; BW: body weight; BMI: body mass index; SMBG: self-monitoring of blood glucose
| References | ▴Top |
- Schiffman S. Food recognition by the elderly. J Gerontol. 1977;32(5):586-592.
doi pubmed - Araki A, Izumo Y, Inoue J, Hattori A, Nakamura T, Takahashi R, Takanashi K, et al. [Burden of dietary therapy on elderly patients with diabetes mellitus]. Nihon Ronen Igakkai Zasshi. 1995;32(12):804-809.
doi pubmed - Amagai T, Hasegawa M, Kitagawa M, Haji S. Non-protein calorie: nitrogen ratio (NPC/N) as an indicator of nitrogen balance in clinical setting. Biomed J Sci & Tech Res. 2018;6(1):5013-5015.
- Fukuda Y, Kanazawa R, Yao N, Ishida T, Nakaoka A, Tazuhara M, Yao S, et al. Nutritional intake by meal time zone in geriatric patients is related to nutritional assessment index. J Clin Med Res. 2021;13(6):334-342.
doi pubmed pmc - Fukuda Y, Kohara M, Hatakeyama A, Ochi M, Nakai M. Influence of geriatric patients' food preferences on the selection of discharge destination. J Clin Med Res. 2020;12(11):705-710.
doi pubmed pmc - Fukuda Y, Ochi M, Kanazawa R, Nakajima H, Fukuo K, Nakai M. Positive correlation between changes in serum albumin levels and breakfast non-protein calorie/nitrogen ratio in geriatric patients. J Clin Med Res. 2023;15(2):109-115.
doi pubmed pmc - Papineni K, Roukos S, Ward T, Zhu W. BLEU: a method for automatic evaluation of machine translation. IBM Research Report. RC22176(W0109-022). 2001.
- Lin CW. ROUGE: a package for automatic evaluation of summaries. Proceeding of the ACL-04 workshop text summarization branches out. In: Text Summarization Branches Out. Barcelona: Association for Computational Linguistics; 2004. p. 74-81.
- Luhn HP. A statistical approach to mechanized encoding and searching of literary information. IBM J Res Dev. 1957;1(4):309-317.
- Sparck Jones K. A statistical interpretation of term specificity and its application in retrieval. J Doc. 1972;28(1):11-21
- Lee J, Maslove DM, Dubin JA. Personalized mortality prediction driven by electronic medical data and a patient similarity metric. PLoS One. 2015;10(5):e0127428.
doi pubmed pmc - Murakami K, Shinozaki N, Yuan X, Tajima R, Matsumoto M, Masayasu S, Sasaki S. Food choice values and food literacy in a nationwide sample of Japanese adults: associations with sex, age, and body mass index. Nutrients. 2022;14(9):1899.
doi pubmed pmc - Unden AL, Elofsson S, Andreasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med. 2008;5(2):162-180.
doi pubmed - Mathew R, Gucciardi E, De Melo M, Barata P. Self-management experiences among men and women with type 2 diabetes mellitus: a qualitative analysis. BMC Fam Pract. 2012;13:122.
doi pubmed pmc - Aguilar R. Managing type 2 diabetes in men. J Fam Pract. 2012;61(6 Suppl):S16-S21.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


