| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 2, February 2023, pages 99-108
Cannabis Use and Its Association With Thirty- and Ninety-Day Hospital Readmissions for Patients Admitted for an Inflammatory Bowel Disease Exacerbation
Ellen A. Osenia, d , Miriam Blumenthala, Stephanie Izardb, Michael Qiub, Anjali Monec, Arun Swaminathc, Keith Sultana
aDivision of Gastroenterology, Northshore University Hospital, Manhasset, NY, USA
bCenter for Health Innovations and Outcomes Research, Feinstein Institutes for Medical Research, Manhasset, NY, USA
cDivision of Gastroenterology, Lenox Hill Hospital, New York, NY, USA
dCorresponding Author: Ellen Oseni, Division of Gastroenterology, Northshore University Hospital, Manhasset, NY 11030, USA
Manuscript submitted November 19, 2022, accepted February 9, 2022, published online February 28, 2023
Short title: Cannabis Use in an Inflammatory Bowel Disease
doi: https://doi.org/10.14740/jocmr4846
| Abstract | ▴Top |
Background: Though viewed as a potentially safer palliative alternative to opioids, studies of cannabis use for inflammatory bowel disease (IBD) are limited. The impact of opioids on hospital readmissions for IBD has been extensively examined, but cannabis has not been similarly studied. Our goal was to examine the relationship between cannabis use and the risk of 30- and 90-day hospital readmissions.
Methods: We conducted a review of all adults admitted for an IBD exacerbation from January 1, 2016 to March 1, 2020 within the Northwell Health Care system. Patients with an IBD exacerbation were identified by primary or secondary ICD10 code (K50.xx or K51.xx) and administration of intravenous (IV) solumedrol and/or biologic therapy. Admission documents were reviewed for the terms “marijuana”, “cannabis”, “pot” and “CBD”.
Results: A total of 1,021 patient admissions met inclusion criteria, of whom 484 (47.40%) had Crohn’s disease (CD) and 542 (53.09%) were female. Pre-admission cannabis use was reported by 74 (7.25%) patients. Factors found to be associated with cannabis use included younger age, male gender, African American/Black race, current tobacco and former alcohol use, anxiety, and depression. Cannabis use was found to be associated with 30-day readmission among patients with ulcerative colitis (UC), but not among patients with CD, after respectively adjusting each final model by other factors (odds ratio (OR): 2.48, 95% confidence interval (CI): 1.06 - 5.79 and OR: 0.59, 95% CI: 0.22 - 1.62, respectively). Cannabis use was not found to be associated with 90-day readmission on univariable analysis (OR: 1.11, 95% CI: 0.65 - 1.87) nor in the final multivariable model after adjusting for other factors (OR: 1.19, 95% CI: 0.68 - 2.05).
Conclusion: Pre-admission cannabis use was found to be associated with 30-day readmission among patients with UC, but not with 30-day readmission for patients with CD nor with 90-day readmission, following an IBD exacerbation.
Keywords: Crohn’s disease; Ulcerative colitis; Inflammatory bowel disease; Cannabis; Opioids
| Introduction | ▴Top |
Inflammatory bowel disease (IBD), consisting primarily of ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic inflammatory condition affecting more than 1.5 million people in the United States [1]. Disease severity and/or complications frequently require hospitalization. These hospitalizations and high rates of hospital readmission are major factors contributing to the high cost of IBD-related care, and significantly diminish quality of life (QOL) in this population [2, 3]. It is widely acknowledged that factors associated with an increased risk of hospital readmission among IBD patients need to be better understood and addressed.
Prior analyses of factors associated with IBD hospital readmissions have included disease severity, corticosteroid use, surgical procedures, psychiatric disorders including anxiety and depression, psychological stressors, chronic pain and opioid use [1, 4-12]. Opioid use in the setting of IBD has been extensively studied. In addition to higher rates of hospital readmission, opioids have been associated with an increased risk of infection and death among IBD patients, and their use is generally discouraged in this population [13-16].
Given ongoing concerns regarding the use of opioids, many IBD patients have turned to cannabis as a potentially safer palliative alternative to opioids for symptom management. Cannabis use appears to be common in the IBD population with rates estimated as high as 10-12%, even prior to the legalization of cannabis in many states for both recreational and/or medical use [17]. New York State has specifically identified IBD as a condition qualifying those suffering to obtain medicinal cannabis legally. While studies of cannabis have not shown it to improve the inflammation associated with IBD, it may be an effective palliative therapy for complaints such as pain, anorexia and diarrhea [17-19]. However, as has long been the concern with opioid use, there is a risk that cannabis may merely mask complaints as the disease progresses, and/or patients may be tempted to underutilize or discontinue use of their standard IBD medications. Given the increasing use of cannabis in IBD, analyses for potential complications need to be conducted, as has been the case with opioids. The aim of this study was to examine the relationship between cannabis use and the risk of 30- and 90-day hospital readmissions among patients with IBD exacerbation.
| Materials and Methods | ▴Top |
Study design
IRB approval was obtained for a retrospective review of all adult IBD patients over the age of 18 who were admitted through the emergency room (ER), and underwent hospitalization for an IBD exacerbation from January 1, 2016 to March 1, 2020 within the Northwell Health Care system. The beginning date corresponds to the availability of legalized cannabis for IBD medicinal purposes in New York State. Patients were identified by either a primary or secondary ICD10 code (K50.xx, K51.xx), corresponding to CD or UC. The sample was limited to patients with an IBD exacerbation defined by administration of intravenous (IV) solumedrol and/or biologic therapy during the index admission. For patients with multiple admissions during the study period, only the first recorded admission was regarded as the index hospitalization, limiting each patient analyzed to one index admission. Pregnant patients and those who underwent an IBD-related surgery during the index admission were excluded from analysis.
Variables of interest
Patient characteristics and exposures examined included age in years, gender, disease type (CD vs. UC), race (African American/Black, Asian, other/multiracial, White), tobacco use (current, former, never, unknown), and alcohol use (current, former, never, unknown), a diagnosis of anxiety or depression, Charlson comorbidity index (CCI) score, index admission length of stay (LOS) in days and hospital opioid use. To assess for cannabis use prior to hospitalization, a natural language search of admission documents was performed for the terms “marijuana”, “cannabis”, “pot” and “CBD”. Manual chart review was then performed to confirm cannabis use. Cannabis use was categorized as either active, past or none. Active cannabis use was further classified as medicinal, recreational, or unknown.
Outcomes
The co-primary outcomes of interest were 30-day readmission and 90-day readmission inclusive of ER encounters. Analysis was limited to a single readmission event following the first/index admission for each patient.
Statistical analysis
Demographic and clinical characteristics were summarized descriptively overall and by outcome group for each aim (i.e., cannabis use, 30-day readmission, 90-day readmission). Specifically, categorical variables were summarized using frequencies and percentages, and continuous variables were summarized using means and standard deviations (SDs).
To assess the association between each main exposure and outcome of interest, a series of separate logistic regression models were used. First, the interaction between cannabis use and IBD type was assessed to determine whether the relationship between cannabis use and 30-day or 90-day readmission differed by IBD type. If interaction was identified, analyses were stratified by IBD type. A univariable screen with a cutoff of P < 0.20 was then applied to identify covariates that could potentially be associated with each outcome of interest. If a variable was found to meet the screening threshold or was one of the main characteristics/exposures of interest (i.e., cannabis use and hospital opioid use), it was then included in a preliminary multivariable model. Backwards elimination was then applied, and main characteristics of interest were added back in when dropped to reach a final multivariable model for each outcome.
All analyses were completed using R version 4.1.2, and a P-value < 0.05 was considered statistically significant unless otherwise noted. This study was conducted in compliance with the ethical standards of Northwell Health on human subjects as well as with the Helsinki declaration.
| Results | ▴Top |
A total of 1,021 patients were identified who were admitted for an IBD exacerbation within the study period, of whom 484 (47.40%) had CD, 542 (53.09%) were female, and the mean ± SD age was 45.28 ± 20.24 years old. Pre-admission cannabis use was reported by 74 (7.25%) patients (Table 1). Cannabis use was most commonly reported to be recreational (63.00%) (Fig. 1). In total, 322 patients (31.54%) had any use of opioids during admission. On adjusted analysis, younger age was found to be associated with cannabis use, as were male gender, African American race, current tobacco use, former alcohol use, anxiety, and depression (Table 2).
 Click to view | Table 1. Demographic and Patient Characteristics (N = 1,021) |
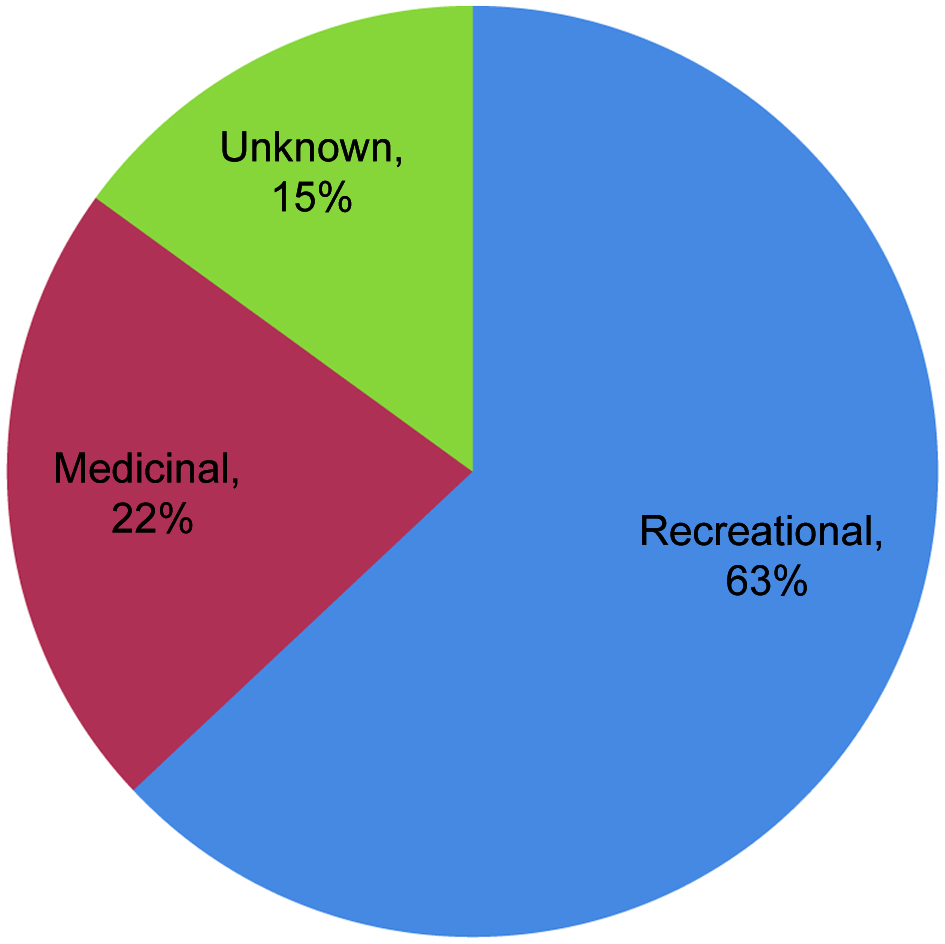 Click for large image | Figure 1. Cannabis use classifications. |
 Click to view | Table 2. Association Between Pre-Admission Characteristics and Cannabis Use (N = 1,021) |
30-day readmission
A total of 184 (18.02%) patients were readmitted within 30 days, 92 of whom had CD and 92 had UC. Assessment of interaction between cannabis use and IBD type for 30-day readmission was found to be significant, indicating that the relationship between cannabis use and 30-day readmission was found to differ by IBD type (P = 0.0223). Analyses were therefore stratified by IBD type (CD and UC) (Tables 3 and 4, respectively).
 Click to view | Table 3. Association Between Cannabis Use and Hospital Opioid Use With 30-Day Readmission Among Patients With Crohn’s Disease (N = 484) |
 Click to view | Table 4. Association Between Cannabis Use and Hospital Opioid Use With 30-Day Readmission Among Patients With Ulcerative Colitis (N = 537) |
For CD, variables selected using the univariable screen to be used in the preliminary multivariable model included cannabis use, hospital opioid use, race, history of depression, CCI, and LOS on index hospitalization. Cannabis use was not found to be associated with 30-day readmission on univariable analysis nor in the final multivariable analysis adjusting for hospital opioid use, race, depression, and CCI (odds ratio (OR): 0.55, 95% confidence interval (CI): 0.21 - 1.45 and OR: 0.59, 95% CI: 0.22 - 1.62, respectively). Hospital opioid use was also not found to be associated with 30-day readmission on univariable analysis nor in the final multivariable analysis adjusting for cannabis use, race, depression, and CCI (OR: 1.45, 95% CI: 0.91 - 2.31 and OR: 1.45, 95% CI: 0.89 - 2.33, respectively). The final multivariable model indicated that African American/Black race, other/multiracial race, and higher CCI were risk factors for 30-day readmissions.
For UC, variables selected using the univariable screen to be used in the preliminary multivariable model included cannabis use, hospital opioid use, age, race, tobacco use, alcohol use, CCI, and LOS on index hospitalization. Cannabis use was found to be associated with 30-day readmission on univariable analysis as well as in the final multivariable analysis after adjusting for hospital opioid use, race, and LOS on index hospitalization (OR: 2.35, 95% CI: 01.07 - 5.14 and OR: 2.48, 95% CI: 1.06 - 5.79, respectively). Hospital opioid use was again not found to be associated with 30-day readmission on univariable analysis nor in the final multivariable analysis adjusting for cannabis use, race, and LOS on index hospitalization (OR: 1.01, 95% CI: 0.61 - 1.66 and OR: 0.79, 95% CI: 0.46 - 1.36, respectively). The final multivariable model also indicated that African American/Black race, other/multiracial race, and longer LOS on index hospitalization were risk factors for 30-day readmissions.
90-day readmission
Assessment of interaction between cannabis use and IBD type for 90-day readmission was not found to be significant, indicating that the relationship between cannabis use and 90-day readmission was not found to differ by IBD type (P = 0.1249). A total of 271 patients (26.54%) were readmitted within 90 days (Table 5). Using the univariable screen, cannabis use, hospital opioid use, age, gender, tobacco use, alcohol use, IBD type, CCI, and LOS on index hospitalization were selected to be included in the preliminary multivariable model. On univariable analysis as well as in the final multivariable model after applying backwards elimination, neither cannabis use (OR: 1.11, 95% CI: 0.65 - 1.87 and OR: 1.19, 95% CI: 0.68 - 2.05, respectively), nor hospital opioid use (OR: 1.16, 95% CI: 0.86 - 1.56 and OR: 1.01, 95% CI: 0.74 - 1.37, respectively) were found to be associated with 90-day readmission. However, younger age, CD, higher CCI, and longer LOS on index hospitalization were found to be risk factors for 90-day readmission.
 Click to view | Table 5. Association Between Cannabis Use and Hospital Opioid Use With 90-Day Readmission (N = 1,021) |
There were 15 patients found to have a readmission within 30 days, and 21 patients found to have a readmission within 90 days among patients with a history of cannabis use. For both 30-day and 90-day readmissions, the majority of patients were readmitted due to a non-IBD related (“other”) cause, 11 (73.33%) and 12 (57.14%) respectively.
| Discussion | ▴Top |
Despite advances in care, IBD hospitalization and readmission continues to have a major impact both on the cost of care and QOL of IBD patients. Our observation of 18% readmission within 30 days and 26.5% within 90 days is in keeping with findings from other recent analyses from large academic centers, cohort studies and the National Readmissions Database (NRD). Our findings of more frequent readmission among patients with longer index hospitalizations and higher comorbidities have also been observed previously [4, 5, 10]. We observed significant associations between cannabis use and younger age, male gender, African American race, tobacco use, anxiety, depression and former alcohol use. We noted that former rather than current alcohol use was associated with cannabis. The study design would not allow for further analysis of this observation, though we speculate that cannabis may also serve as a “substitute” for those with prior alcohol use. For our primary outcomes, cannabis use was noted to be associated with 30-day, but not 90-day readmission in the UC cohort, and was not associated with either 30- or 90-day readmission for those with CD.
Notably, we did not find an association between opioid use during hospitalization and readmission. Prior analysis of this issue has been mixed. Charilaou et al’s recent analysis of opioid use disorder (OUD) from the NRD from 2010 to 2014 observed a significant association with OUD and 30-day readmission, hazard ratio 1.47, 95% CI 1.28 - 1.69, P < 0.001 [20]. However, OUD, which was identified in only 1.4% of patients, appears to be a distinct entity from the far more common inpatient opioid use. We observed opioid use by almost a third of patients, also consistent with findings of other large cohort studies [21, 22] and recent meta-analysis [14]. A recent Cleveland Clinic cohort report from Hazratjee et al also found no association between inpatient opioid use and readmission, while noting that those discharged without opioids had a 2.2-fold increased risk for readmission [6].
Our study is among the first to examine cannabis use among patients hospitalized for IBD exacerbation. We found that slightly over 7% of patients reported pre-admission cannabis use, with a majority self-categorizing as recreational users. It is important to emphasize that various aspects of cannabis use vary across countries. Ransing et al demonstrated a higher prevalence of cannabis use among teenagers in countries such as South Africa, Italy and Spain [23]. Thailand in comparison demonstrated an overall decline in cannabis use across ages [23]. While the prevalence demonstrated in our study is lower than that of recent outpatient studies showing rates of active cannabis use of 10-12% [24, 25], it is similar to the findings of Dalal et al’s recent cohort reporting 8% active cannabis use among IBD inpatients [21]. As was the case with descriptions of opioid use, the method of analysis of cannabis use appears to impact this figure. Micic et al’s study of the NRD, utilizing the ICD code for cannabis dependence, reported a rate of only 1.6%. Cannabis dependence was associated with an increased risk of 30-day hospital readmission on univariate analysis, but not multivariate analysis [9]. Our analysis of cannabis use, as distinct from cannabis dependence, revealed an association between cannabis and 30-day readmission for patients with UC. In such a large registry as the NRD, it is impossible to say how precise the application of the diagnosis of cannabis dependence truly was, but the lower prevalence suggests a distinct and perhaps more medically significant entity from the more common cannabis use. Also, while our cohort showed similar rates of cannabis use to Dalal et al, we did not repeat their observation of higher inpatient opioid use by cannabis users, despite high rates of opioid use in each cohort. This leaves open the question of whether cannabis use is a “gateway” drug/predictor of future opioid use. Considering the increasing availability of cannabis, and the dismal history of opioids for IBD [26], this is an important question for future study.
Limitations to the study are those common to retrospective analysis of real-world data pulled from an electronic health record. While the methodology of the natural language search offered the ability to capture documentation of cannabis use beyond specific data point entries, it seems likely that many cannabis users were missed. Though documentation of cannabis use is encouraged by the electronic health record (EHR), it is not required to complete the admission process, at which time this history is typically recorded. Also, though cannabis use is becoming more accepted by society in general, it seems likely that the history of stigma and illegality associated with its use might cause some patients to withhold information of their own cannabis use. Also, while it would have been helpful for study purposes, urine toxicology for cannabis for objective evidence of use was (and is) not required at the study institutions, and was rare among those hospitalized for an IBD exacerbation. Though many of the typical cofactors associated with readmission were accessible by inpatient EHR data extraction, such as age, length of stay, and CCI, the data pull could not account for other factors that may have been associated with readmissions. Disease duration and severity quantified by accepted disease activity indices were not calculated during hospitalization for the study population and were therefore unknown. Also, post-discharge factors such as corticosteroid tapering and the timeliness of outpatient follow-up, which has also been observed to impact IBD readmissions [8], were not available for inclusion in our analysis. Also, we chose to include patients with a secondary admitting diagnosis of either CD or UC, but maintained the same standard of inpatient corticosteroid and/or biologic consistent with disease flare. This was intended to avoid excluding admissions for IBD for whom the admitting general medicine doctor may have preferred the use of an alternate primary admitting diagnostic code. Numbers of cannabidiol (CBD) users were also too few to perform any meaningful sub-analysis. Finally, the main limitation of the study was our inability to track cannabis use post discharge. Given the palliative properties of cannabis, it would be reasonable to assume that its use would continue or even increase following IBD hospitalization. This remains an assumption, leaving an unfilled gap in our knowledge of how cannabis use may impact rehospitalization.
In conclusion, our analysis of 30- and 90-day hospital readmissions in a large cohort of patients hospitalized with an IBD exacerbation confirmed risk factors for readmission including longer index hospitalization/LOS, and increased medical comorbidities. Inpatient opioid use was not associated with hospital readmission. A history of cannabis use was not associated with more frequent readmissions following an CD exacerbation, but was for UC patients within 30 days. As cannabis use becomes more prevalent, and as its use as a palliative therapy becomes more accepted, further analyses will be needed to better understand its impact on long-term outcomes. The current study suggests a possible “red flag” in regards to cannabis use and rehospitalization, but further studies incorporating the outpatient IBD/cannabis experience post discharge are needed to further endorse its use in this important population.
Acknowledgments
We thank Northwell Health, Center for Health Innovations and Outcomes Research, Department of Medicine Biostatistics Unit, Feinstein Institute of Medical Research.
Financial Disclosure
None to declare.
Conflict of Interest
The authors disclose no conflict of interest.
Informed Consent
Study obtained IRB approval to waive documented informed consent.
Author Contributions
Ellen Oseni: conception and design of the study; acquisition of data; drafting the article and revising it for critically important intellectual content. Miriam Blumenthal: acquisition of data; interpretation of data. Stephanie Izard: statistical analysis of data; interpretation of data; drafting the article and revising it for critically important intellectual content. Michael Qiu: acquisition of data. Anjali Mone: drafting the article and revising it for critically important intellectual content. Arun Swaminath: drafting the article and revising it for critically important intellectual content. Keith Sultan: conception and design of the study; interpretation of data; drafting the article and revising it for critically important intellectual content; final approval of the version to be submitted.
Data Availability
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
| References | ▴Top |
- Allegretti JR, Borges L, Lucci M, Chang M, Cao B, Collins E, Vogel B, et al. Risk factors for rehospitalization within 90 days in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2015;21(11):2583-2589.
doi pubmed - Dias CC, Santiago M, Correia L, Portela F, Ministro P, Lago P, Trindade E, et al. Hospitalization trends of the inflammatory bowel disease landscape: a nationwide overview of 16 years. Dig Liver Dis. 2019;51(7):952-960.
doi pubmed - Park KT, Ehrlich OG, Allen JI, Meadows P, Szigethy EM, Henrichsen K, Kim SC, et al. The cost of inflammatory bowel disease: an initiative from the Crohn's & Colitis Foundation. Inflamm Bowel Dis. 2020;26(1):1-10.
doi pubmed - Barnes EL, Kochar B, Long MD, Kappelman MD, Martin CF, Korzenik JR, Crockett SD. Modifiable risk factors for hospital readmission among patients with inflammatory bowel disease in a nationwide database. Inflamm Bowel Dis. 2017;23(6):875-881.
doi pubmed - Christian KE, Jambaulikar GD, Hagan MN, Syed AM, Briscoe JA, Brown SA, Campbell EV, 3rd, et al. Predictors of early readmission in hospitalized patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017;23(11):1891-1897.
doi pubmed - Hazratjee N, Agito M, Lopez R, Lashner B, Rizk MK. Hospital readmissions in patients with inflammatory bowel disease. Am J Gastroenterol. 2013;108(7):1024-1032.
doi pubmed - Long DR, Lihn AL, Friedrich S, Scheffenbichler FT, Safavi KC, Burns SM, Schneider JC, et al. Association between intraoperative opioid administration and 30-day readmission: a pre-specified analysis of registry data from a healthcare network in New England. Br J Anaesth. 2018;120(5):1090-1102.
doi pubmed - Malhotra A, Phatharacharukul P, Thongprayoon C. Risk factors for 90-day readmission in veterans with inflammatory bowel disease-Does post-discharge follow-up matter? Mil Med Res. 2018;5(1):5.
doi pubmed - Micic D, Gaetano JN, Rubin JN, Cohen RD, Sakuraba A, Rubin DT, Pekow J. Factors associated with readmission to the hospital within 30 days in patients with inflammatory bowel disease. PLoS One. 2017;12(8):e0182900.
doi pubmed - Mudireddy P, Scott F, Feathers A, Lichtenstein GR. Inflammatory bowel disease: predictors and causes of early and late hospital readmissions. Inflamm Bowel Dis. 2017;23(10):1832-1839.
doi pubmed - Nguyen GC, Bollegala N, Chong CA. Factors associated with readmissions and outcomes of patients hospitalized for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12(11):1897-1904.e1.
doi pubmed - Tinsley A, Naymagon S, Mathers B, Kingsley M, Sands BE, Ullman TA. Early readmission in patients hospitalized for ulcerative colitis: incidence and risk factors. Scand J Gastroenterol. 2015;50(9):1103-1109.
doi pubmed - Dalal RS, Palchaudhuri S, Snider CK, Lewis JD, Mehta SJ, Lichtenstein GR. Exposure to intravenous opioids is associated with future exposure to opioids in hospitalized patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2020;18(10):2269-2278.e2263.
doi pubmed - Niccum B, Moninuola O, Miller K, Khalili H. Opioid use among patients with inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2021;19(5):895-907.e894.
doi pubmed - Cohen-Mekelburg S, Rosenblatt R, Gold S, Burakoff R, Waljee AK, Saini S, Schackman BR, et al. The impact of opioid epidemic trends on hospitalised inflammatory bowel disease patients. J Crohns Colitis. 2018;12(9):1030-1035.
doi pubmed - Kienzl M, Storr M, Schicho R. Cannabinoids and opioids in the treatment of inflammatory bowel diseases. Clin Transl Gastroenterol. 2020;11(1):e00120.
doi pubmed - Ahmed W, Katz S. Therapeutic use of cannabis in inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2016;12(11):668-679.
- Swaminath A, Berlin EP, Cheifetz A, Hoffenberg E, Kinnucan J, Wingate L, Buchanan S, et al. The role of cannabis in the management of inflammatory bowel disease: a review of clinical, scientific, and regulatory information. Inflamm Bowel Dis. 2019;25(3):427-435.
doi pubmed - Doeve BH, van de Meeberg MM, van Schaik FDM, Fidder HH. A systematic review with meta-analysis of the efficacy of cannabis and cannabinoids for inflammatory bowel disease: what can we learn from randomized and nonrandomized studies? J Clin Gastroenterol. 2021;55(9):798-809.
doi pubmed - Charilaou P, Mohapatra S, Joshi T, Devani K, Gadiparthi C, Pitchumoni CS, Goldstein D. Opioid use disorder increases 30-day readmission risk in inflammatory bowel disease hospitalizations: a nationwide matched analysis. J Crohns Colitis. 2020;14(5):636-645.
doi pubmed - Dalal RS, Palchaudhuri S, Snider CK, Lewis JD, Mehta SJ, Lichtenstein GR. Preadmission cannabis use is positively correlated with inpatient opioid dose exposure in hospitalized patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2021;27(4):500-506.
doi pubmed - Berry SK, Takakura W, Bresee C, Melmed GY. Pain in inflammatory bowel disease is not improved during hospitalization: the impact of opioids on pain and healthcare utilization. Dig Dis Sci. 2020;65(6):1777-1783.
doi pubmed - Ransing R, de la Rosa PA, Pereira-Sanchez V, Handuleh JIM, Jerotic S, Gupta AK, Karaliuniene R, et al. Current state of cannabis use, policies, and research across sixteen countries: cross-country comparisons and international perspectives. Trends Psychiatry Psychother. 2022;44(Suppl 1):e20210263.
doi pubmed - Ravikoff Allegretti J, Courtwright A, Lucci M, Korzenik JR, Levine J. Marijuana use patterns among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(13):2809-2814.
doi pubmed - Lal S, Prasad N, Ryan M, Tangri S, Silverberg MS, Gordon A, Steinhart H. Cannabis use amongst patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2011;23(10):891-896.
doi pubmed - Sultan K, Swaminath A. From bad to worse: the relationship between opioid use and inflammatory bowel disease. J Crohns Colitis. 2020;14(9):1188-1189.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


