| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 1, January 2023, pages 23-30
Factors Influencing Sarcopenic Changes in YUBI-WAKKA Finger-Ring Test Results After One Year: A Retrospective Observational Study
Hitomi Fujiia, e, Eitaro Kodanib, Tomohiro Kanekoc, Hiroyuki Nakamurad, Hajime Sasabed, Yutaka Tamurad
aDepartment of Internal Medicine, Tama-Center Mirai Clinic, Tama City, Tokyo, Japan
bDepartment of Cardiovascular Medicine, Nippon Medical School Tama-Nagayama Hospital, Tama City, Tokyo, Japan
cDepartment of Nephrology, Nippon Medical School Tama-Nagayama Hospital, Tama City, Tokyo, Japan
dTama City Medical Association, Tama City, Tokyo, Japan
eCorresponding Author: Hitomi Fujii, Department of Internal Medicine, Tama-Center Mirai Clinic, Tama City, Tokyo, Japan
Manuscript submitted October 16, 2022, accepted January 18, 2023, published online January 24, 2023
Short title: Sarcopenic Changes After Finger-Ring Retest
doi: https://doi.org/10.14740/jocmr4827
| Abstract | ▴Top |
Background: The YUBI-WAKKA (finger-ring) test was developed and validated as a predictor of sarcopenia, physical disability, and even mortality. We focused on the sarcopenic status and subsequent changes after 1 year using this test and analyzed factors related to these changes. We also examined the robustness of this test by administering it alongside annual checkups held in local clinics.
Methods: We conducted the study to investigate the data of the annual checkup of National Health Insurance at primary care clinics in 2017 and 2018 in Tama City. We studied the participants in a retrospective observational way. The participants of the YUBI-WAKKA test were a total of 5,405 and 4,391 residents between the ages of 65 and 74 years. We first compared anthropological biomarkers of two groups, those that had calves larger than their own finger-ring and those that had calves smaller than their own finger-ring. Then, we compared these results to those from the previous year’s 1,048 pairs of data. We were particularly interested in changes from larger to smaller, which we defined here as a sarcopenic change, and performed multivariate logistic regression analysis with forced entry methods to determine the related factors. We also calculated the concordant rate of the test results after 1 year.
Results: In total, 14% (men) and 16% (women) each year received a positive (sarcopenic) YUBI-WAKKA test result. The factors related to this sarcopenic change in 1 year were low uric acid in men and a low or decreasing body mass index and increased hemoglobin and alanine aminotransferase in women. The concordant rates of the larger, just fit and smaller groups following finger-ring testing were 72.8%, 63.5%, and 52.0%, respectively.
Conclusions: We propose that low uric acid and low or reducing body weight were related to low muscle mass and that ALT and Hb may be indirectly related to sarcopenia. These could be predictive factors to determine sarcopenia-prone individuals. The YUBI-WAKKA (finger-ring) test results and their change were considered to be a sustainable and reasonable way to use in the community with small effort to find those who are at high risk for sarcopenia among the elderly population and who may require intervention.
Keywords: Frailty; Sarcopenia; YUBI-WAKKA (finger-ring) test
| Introduction | ▴Top |
The YUBI-WAKKA (finger-ring) test was developed by Professor Iijima et al [1] as a simple self-check method that does not require any technical instruments and was validated for its ability to identify the risk of sarcopenia, disability, and mortality in the future. In Tama City, a western suburb of Tokyo, the Tama City Medical Association participated in the study by including the YUBI-WAKKA test while conducting annual checkups for their patients in 2017. The test was performed in a half-self-screened manner (self-screened, but under the direction of medical staff) and feasible enough to show any relationships with other clinical data. The results of these tests have been reported in previous studies [2, 3]. However, two main agendas remained: to ascertain test-retest variability and to observe the change over the course of time. Thus, after obtaining the results 1 year later, we decided to determine: 1) any apparent changes in patient status, from normal to sarcopenic, whereby examinee calves are larger or smaller than their finger-ring size, using the YUBI-WAKKA finger-ring test, 2) a causal relationship or factors related to this change, and 3) the robustness of this test by comparing the two datasets, before and after 1 year.
| Materials and Methods | ▴Top |
Participants
Tama City offers an annual checkup to citizens aged 40 - 74 years and who are covered by National Health Insurance. The average rate of participation was around 60% of all eligible citizens. The primary care doctors were asked to perform the YUBI-WAKKA test, but it was not mandatory. In total, the YUBI-WAKKA test was administered to 5,405 and 4,391 examinees aged 65 years or older in the first (2017) and second (2018) year, respectively, and mainly at primary care clinics in the private sector. The inclusion criterion was limited to an age range of 65 - 74 years because the YUBI-WAKKA test is performed to screen for sarcopenia, disability, and even mortality in elderly populations. No exclusion criteria were set except if their primary care doctors refused to administer the test.
Ethics and consent
As our research is based on the results of the annual checkup of National Health Insurance conducted by the city, Tama City and the Tama City Medical Association informed citizens and/or patients that the checkup data could be used for public health research, anonymously analyzed, and published. All participants were given the right to withdraw. Tama City and the Tama City Medical Association publicized this opt-out procedure as part of their public relations. Our study was conducted in accordance with the Declaration of Helsinki (as revised in Brazil 2013) and IRB approval was obtained from the Tama-Center Mirai Clinic (No. 2020013).
Study design of TAMA MED Project-Frail
The TAMA MED projects (Frail [2, 3], AF [4], CKD [5, 6]) have been conducted by the Tama City Medical Association to analyze consecutive annual health checkup data performed under the National Health Insurance. This cross-sectional study retrospectively observed the prevalence of sarcopenia using the finger-ring test, evaluated any test result changes after 1 year, and analyzed factors relating to these changes.
YUBI-WAKKA (finger-ring) test
The detailed method of this test has been explained elsewhere [1]. Briefly, the examinee surrounds their non-dominant calf using their thumbs and index fingers of both hands joined together (finger-ring) while they are in a sitting position, and whether their calf circumference is larger, just fits, or is smaller than their finger-ring is determined. In this study, calf circumference and its changes after 1 year were analyzed.
National Health Insurance annual checkup in Tama City
Anthropological data, such as body height (BH), body weight (BW), waist circumference (WC), and blood pressure (BP), were measured. Blood (serum albumin, liver, kidney, lipids, glucose, and blood cell counts) and urine samples were obtained along with simple medical history questions. The registered local clinic practitioners were sent a written request to participate in the YUBI-WAKKA test along with visual instructions. They were also asked whether their staff would explain the procedure and observe the examinees.
Statistical analysis
We analyzed the relationships between the results of the YUBI-WAKKA test and the other clinical data. We excluded the intermediate, “just fits” group, and compared the remaining two groups (larger and smaller). Smaller meant the participants calf circumference was smaller than their finger-ring, and was considered as a positive test result. We also analyzed the concordance of the results after 1 year and any change that had occurred. We especially focused on changes from the larger to smaller group, which was defined as a sarcopenic change.
We used Student’s t-tests to compare the means of the groups and Chi-square tests to analyze the prevalence of change. We also used a logistic regression test to adjust for multiple variables to determine factors related to the sarcopenic change separated by sex after a year. All variables (age, body mass index (BMI), WC, systolic and diastolic blood pressure (SBP, DBP), existence of metabolic syndrome (MetS) (no-, pre-, and MetS), hemoglobin A1c (HbA1c), red blood cell (RBC) count, hemoglobin (Hb), albumin (ALB), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), creatinine (Cr), estimated glomerular filtration rate (eGFR), creatine kinase (CK), asparagine aminotransferase/glutamic oxaloacetic transaminase (AST/GOT), alanine transaminase/glutamic pyruvic transaminase (ALT/GPT), gamma glutamic pyruvic transaminase (gGTP), alkaline phosphatase (ALP), amylase (AMY), and uric acid (UA)) were entered simultaneously. We also entered the change of each of the values from 2017 to 2018 as delta BMI (dBMI), dBW, dWC, dHbA1c, dHb, dALB, dHDL-C, dLDL-C, dTG, dCr, deGFR, dCCr, dCK, dAST/GOT, dALT/GPT, dgGTP, dALP, dAMY, and dUA. We checked correlations of each variable, and to avoid collinearity, we used BMI instead of BW, eGFR instead of CCr. All statistical analyses were performed using SPSS version 23.0 (IBM Corp., Armonk, NY, USA).
| Results | ▴Top |
We obtained data from 5,405 participants in 2017 (as baseline data) and from 4,391 participants in the 2018 (as the second year data). In total, 38.8% and 41.4% of the participants’ calves were grouped as larger than their finger-ring in 2017 and in 2018, respectively. The just fits group were 45.6% and 43.4%, and the smaller group, which is the positive test result group, were 15.6% and 15.2%, respectively (Table 1).
 Click to view | Table 1. The Distribution of the Results of the Finger-Ring Test in 2017 and 2018 |
From the whole data, we obtained 3,481 paired data from the same subject of baseline and second year (Table 2). In these twice test results, the concordance of the result was seen in 2,277 pairs (65.4%). The concordant rate was not significantly different between sexes, and was 72.8%, 63.5%, and 52.0% in the larger, just fits, and smaller groups, respectively. The concordance rate was highest in the larger group, lower in the just fits group and was the lowest in the smaller group. The Spearman’s correlation coefficient was 0.547 (P < 0.01) overall. The kappa-value was 0.469 for men and 0.419 for women.
 Click to view | Table 2. The Intra-Individual Concordance of the Results Between Baseline (2017) and the Second Year (2018) |
In 2018, 35 of 52 clinics (67.3%) that participated in the annual health checkup cooperated with this pilot study and answered our questionnaire (Fig. 1). Question 1 asked whether the clinic staff explained the procedure of this test or not (only by showing the picture to the examinee and having them do it by themselves). Question 2 asked whether the test was performed under staff supervision. For both questions, 27 facilities (77.1%) out of 35 answered “yes”, and five (14.3%) answered “no”. Meanwhile, 23 clinics answered affirmatively to both the questions. The age and sex of the examinees were not significantly different between both groups. The examinees who had not received an explanation on how to perform the test accurately (n = 396 out of 3,737), tended not to choose “larger” as opposed to the group that received an explanation (Chi-squared test: P < 0.001). Additionally, those who had not been observed while performing the test (n = 610 out of 3,503) chose “just fits” more than “larger” or “smaller” (P < 0.001).
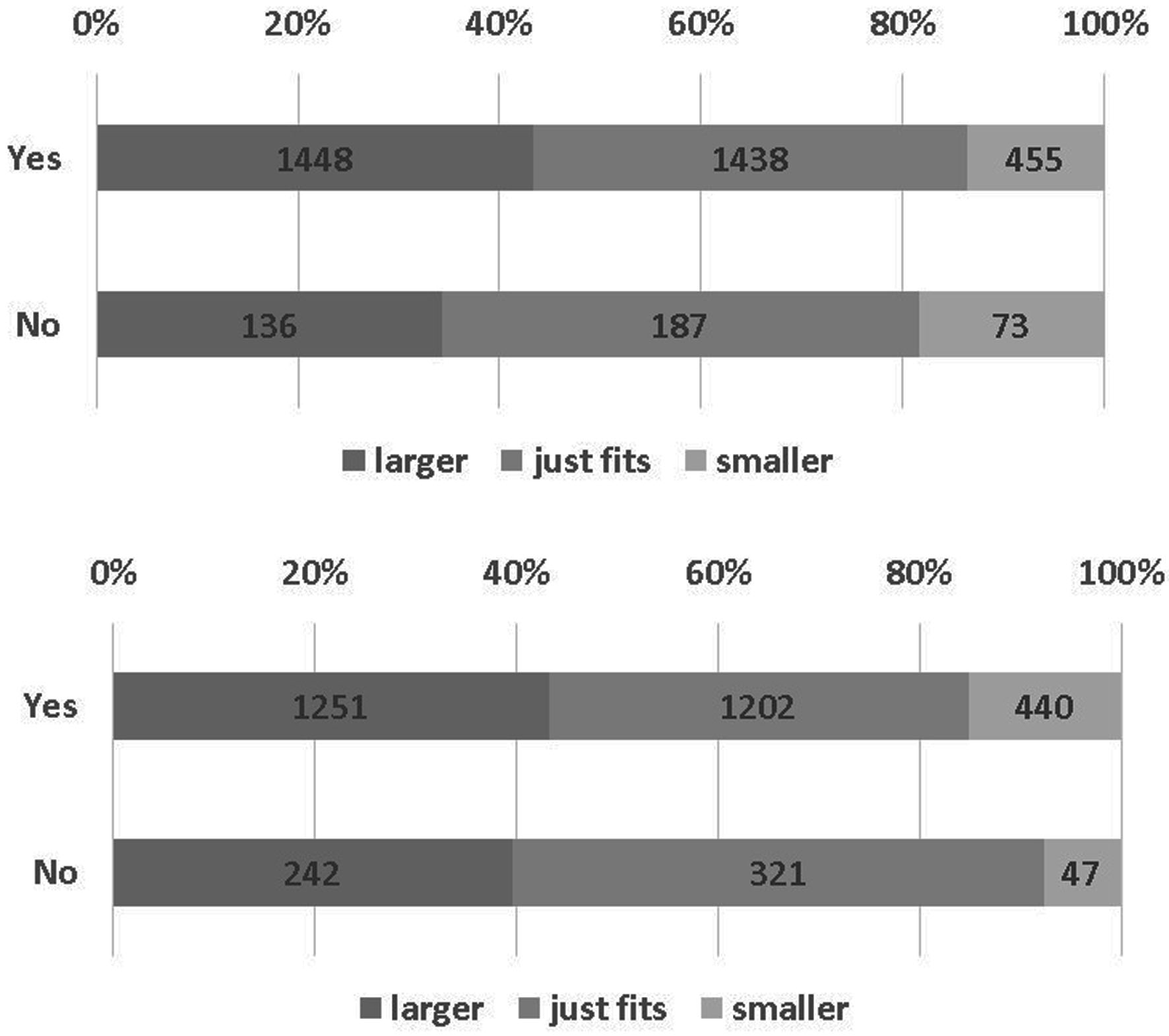 Click for large image | Figure 1. Answers to the questionnaire and the results of YUBI-WAKKA test (Chi-square test). Question 1 (upper): Did you explain your patients how to do the YUBI-WAKKA test? P < 0.001 by Chi-square test. Question 2 (lower): Did your patients do the YUBI-WAKKA test under observation of medical staff? P < 0.001 by Chi-square test. It indicates that the null hypothesis was rejected between the distributions of the two groups. |
When analyzing the baseline data (Table 3), BH in the smaller group was higher than the larger group, while BW and WC were smaller. BP was lower among women. Less MetSs were seen among individuals with smaller (calves), who showed lower HbA1c levels, lower TG, more HDL-C, and lower CCr with higher eGFR, lower ALT, UA, and higher AMY than individuals with larger calves. Lower LDL-C and CK were only observed in men with smaller calves. Lower Cr was only seen in women with smaller calves. The tendency between sex was opposite for gGTP and ALP.
 Click to view | Table 3. The Comparison of the Baseline Data Between “Larger” and “Smaller” Groups |
In total, 51 examinee results changed two ranks between the baseline and the second year, from larger (calves) to smaller (calves). We analyzed these cases by comparison to the 997 paired data from the “non-sarcopenic” unchanged test result group (larger to larger). Factors related to this change were analyzed by logistic regression analysis. In multivariate analysis (Table 4), increased Hb and increased ALT in women were related to this sarcopenic (larger to smaller calves) change. Lower UA at the baseline in men and lower and decreased BMI in women were also attributed to this change.
 Click to view | Table 4. Multivariate Logistic Regression Analysis of the Related Factors to the Change of “Larger” to “Smaller” Calves Than Finger-Rings From the Baseline to Second Year (Forced Entry Method) |
| Discussion | ▴Top |
Administration manner of YUBI-WAKKA (finger-ring) test
The YUBI-WAKKA (finger-ring) test was described in the original paper [1] as a self-screening tool; however, we expected it to be performed in a half-self-screened manner as one of the annual health checkup items under medical staff observation in an ordinary primary care setting. In our study, the medical staff only read the explanation and were not trained in a face-to-face manner for this test. Thus, the way by which the test was administered differed between medical facilities (Fig. 1). As such, five out of 35 (14.3%) facilities answered that they administrated this test to their examinees without explanation nor observation, accounting for 10.6% and 17.4% of all the participants in 2017 and 2018, respectively. Hence, the examinees tended to choose the intermediate option (“just fits”) and might have hesitated to choose a more extreme option, especially in the case of larger calves than finger-rings. The “YUBI-WAKKA” (finger-ring) test should be administered under medical staff supervision as it increases both its sensitivity and specificity. In comparison to the original paper [1], the smaller (calves) population rate was the same as ours at 14-15% (Table 1). However, the larger (calves) population in our study was lower at approximately 40%, compared to 53% [1]. A reason for the lower detection of the larger group population might be because of the different backgrounds of the participants (health checkup examinees vs. local residents). Our examinees might have had more chronic diseases or a preconceived belief that they should be “lean”. Therefore, we only chose the extreme positive group (smaller calves) and excluded the just fits group to compare to the normal group (larger calves).
The detection of “sarcopenic” individuals
YUBI-WAKKA (finger-ring) test does not distinguish subcutaneous fat and intramuscular fat from muscle mass or directly relate to muscle strength. A report by the European Working Group on Sarcopenia in Older People (EWGSOP) [7] defined sarcopenia as requiring one of the following: low muscle mass, low muscle strength, or low physical performance. Meanwhile, the first report about the YUBI-WAKKA (finger-ring) test [1] suggested that when focusing on the prognostic value of physical disabilities and mortality, a positive test result can be considered to reflect “sarcopenic” muscle mass loss.
In our study, serum Cr in women and CK in men tended to be higher in the larger (calves) group (Table 3). Hence, these values were considered to be related to muscle mass. The larger (calves) group tended to have lower estimation of GFR, when eGFR was calculated with Cr. As CCr estimation was considered to be influenced by BW, CCr was estimated to be higher in the larger group. AMY was always tended to be higher in the smaller (calves) group; however, this was not significant in multivariable analysis in our present and previous studies [2, 3]. Some studies reported elevated AMY among patients in the intensive care unit (ICU) [8] and those with eating disorders [9]. The researchers speculated that this was caused by gastric emptying abnormalities as AMY is not always secreted from the pancreas. However, functional dyspepsia is especially prevalent among the Japanese population, which can cause relatively elevated AMY.
YUBI-WAKKA (finger-ring) test-retest concordance after 1 year of consecutive tests
The distribution of the YUBI-WAKKA (finger-ring) test results did not totally differ in the 2017 and 2018 (Table 1). The smaller (calves) rate was 15% among the 65 to 74 years old age group. The index of test-retest variability such as Spearman’s correlation coefficient (0.55) and kappa-value (0.469 for men and 0.419 for women) in 2 years was moderate. The concordant rate in between examinees in 1 year (Table 2) was the highest in the larger (calves) group (72.8%), which included normal, non-sarcopenic individuals. The concordance was lower in the just fits (63.5%) and smaller (calf) (52.0%) groups. The tendency did not differ between sexes. As there was 1-year time interval between tests, we cannot distinguish whether changes were the result of physical change or judgmental errors. According to the definition of normal as larger calves, the 73%, distribution replication seemed to be rational.
The change of YUBI-WAKKA (finger-ring) test in 1 year
There were 51 examinees with sarcopenic change out of 1,048 of the larger (calf) group (4.9%) in the 2017 pairs data. From the multivariate analysis (Table 4), UA in men and increased BMI in women were the protective factors against sarcopenic change. Factors that influenced BW were quite reasonable and had an independent relationship. In our previous reports [2, 3], UA repeatedly showed a negative relationship with sarcopenic change in univariate analysis. However, UA could not be an independent factor in multivariate analysis. A report on kidney transplant patients [10] described that UA levels were positively associated with muscle mass and strength, but not with functional capacity. Among Japanese elderly women [11], UA had a positive relationship with handgrip strength and UA was considered as a biomarker of muscle mass and strength.
Because Hb was often described as a biomarker of sarcopenia, the relationship was naturally considered as negative [12]. However, Hb (also dHb after 1 year in the present study) was independently positive for sarcopenia in our studies [2, 3]. Not many chronic kidney disease individuals were included, as mean eGFR was 72.8 mL/min/1.73 m2 (standard deviation 14.7) even in the smaller (calves) group of women. Also, no apparent differences related to kidney function between groups in univariate analysis were noted. Higher/increasing Hb may be the result of using erythropoietin or iron, or using sodium-glucose co-transporter 2 inhibitor (SGLT2i). Subcutaneous edema might be taken into consideration, and smaller group might be more dehydrated, having thinner calves and be more hemo-concentrated. Smoking may be another reason for the elevated Hb with sarcopenia. No reports indicated a positive relationship between elevated Hb and sarcopenia or smaller muscle mass.
Although ALT (GPT) and AST (GOT) are both hepatic enzymes, ALT (GPT) is more specific to the liver. The ALT/AST ratio has commonly been used as a biomarker for insulin resistance [13] and sarcopenia [14, 15]. Similar to both of our studies [2, 3], univariate analysis showed that ALT was not significantly related to sarcopenia, but positively correlated using multivariate analysis [14, 15]. ALT may be related to insulin resistant individuals and/or liver fibrosis, such as non-alcoholic steatohepatitis (NASH) [16], and might be an indicator of chronic inflammation, another possible factor related to sarcopenia. In our previous study, even after adjusting for BW, MetS was a positive factor of sarcopenia in our cross-sectional study [3]. However, this was not significant in the present study. Thus, we propose that ALT may be a surrogate marker of insulin resistance.
Limitations
The age groups of annual checkup examinees were limited to < 75 years in this study because of the system of National Health Insurance. Thus, the population of participants with sarcopenia under 75 years old was small. Moreover, we only had data of baseline and 1 year later. Although we obtained about 10,000 data per year, to extract positively (sarcopenic) changed data and to compare negative unchanged (normal) data, the number to analyze became small (to less than 1,000). Therefore, we need additional years of data and a population older than 75 years to see the causal relationship between factors and the test results. In addition, the information of social or physical activities, smoking, drinking habits, etc. is needed to analyze “sarcopenia” as it has been defined. We are planning to obtain these background data at the same time in annual checkups.
Conclusions
We found that low UA in men and low or reducing BW and increasing Hb and ALT were possible signs of sarcopenia. Although the results of the YUBI-WAKKA (finger-ring) test were not exactly precise or accurate as other tests, such as skeletal muscle index using dual X-ray absorptiometry or bioelectrical impedance analysis, our results and their change after 1 year were considered to be reliable. We believe that it is also reasonable enough to use this test in the clinic as it requires minor effort and can aid in determining the high-risk elderly population in the community that require intervention.
Acknowledgments
We would like to thank Prof. Katsuya Iijima, who developed the YUBI-WAKKA test, for advising us and permitting us to use the test. We also thank Mr. Junichi Murata for the statistical analysis and the Medical Association members, examinees, and the local government of Tama City.
Financial Disclosure
The TAMA MED project-Frail is supported by the Tama City Medical Association. The sponsors had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Conflict of Interest
EK received remuneration from Daiichi-Sankyo, Bristol-Myers Squibb, and Ono Pharmaceutical.
Informed Consent
The Tama City government and Tama City Medical Association informed examinees that their checkup data may be anonymously analyzed and published for public health research and that they could opt out or refuse to grant their consent.
Author Contributions
All six of the authors contributed of the design of this study, HF, EK and TK analyzed and interpreted the data, drafted and revised the work. HF wrote the manuscript. All authors approved this manuscript for publication and agree to be accountable for all aspects of the work.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
BH: body height; BW: body weight; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; FPG: fasting plasma glucose; RBC: red blood cell; Hb: hemoglobin; ALB: albumin; HDL: high-density lipoprotein; LDL: low-density lipoprotein; TG: triglyceride; Cr: creatinine; eGFR: estimated glomerular filtration rate; CCr: creatinine clearance; CK: creatinine kinase; AST: asparagine aminotransferase; ALT: alanine transaminase; gGTP: gamma glutamyl transpeptidase; ALP: alkaline phosphatase; AMY: amylase; UA: uric acid; GPT: glutamic pyruvic transaminase; GOT: glutamic oxaloacetic transaminase
| References | ▴Top |
- Tanaka T, Takahashi K, Akishita M, Tsuji T, Iijima K. "Yubi-wakka" (finger-ring) test: A practical self-screening method for sarcopenia, and a predictor of disability and mortality among Japanese community-dwelling older adults. Geriatr Gerontol Int. 2018;18(2):224-232.
doi pubmed - Fujii H, Kodani E, Kaneko T, Nakamura H, Sasabe H, Tamura Y. "Yubi-wakka" (Finger-Ring) test: a tool to detect prefrailty in elderly populations, a pilot study. J Clin Med Res. 2019;11(9):623-628.
doi pubmed - Fujii H, Kodani E, Kaneko T, Nakamura H, Sasabe H, Tamura Y. Sarcopenia and coexistent risk factors detected using the 'Yubi-wakka' (finger-ring) test in adults aged over 65 years in the public annual health check-up in Tama City, Tokyo: a cross-sectional study. BMJ Open. 2022;12(12):e061613.
doi pubmed - Kodani E, Kaneko T, Fujii H, Nakamura H, Sasabe H, Tamura Y, Shimizu W. Prevalence and incidence of atrial fibrillation in the general population based on national health insurance special health checkups - TAMA MED Project-AF. Circ J. 2019;83(3):524-531.
doi pubmed - Kodani E, Kaneko T, Fujii H, Nakamura H, Sasabe H, Tamura Y, Shimizu W. Impact of chronic kidney disease classification on new-onset atrial fibrillation in the general population - the TAMA MED Project-AF and CKD. Circ J. 2020;84(10):1693-1700.
doi pubmed - Kaneko T, Kodani E, Fujii H, Nakamura H, Sasabe H, Tamura Y, Tsuruoka S. Medical and dental visits of chronic kidney disease-diagnosed participants analyzed from the specific health checkups results in Japan: TAMA MED Project-CKD. J Clin Med Res. 2020;12(2):115-121.
doi pubmed - Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412-423.
doi pubmed - Muniraj T, Dang S, Pitchumoni CS. Pancreatitis or not? Elevated lipase and amylase in ICU patients. J Crit Care. 2015;30(6):1370-1375.
doi pubmed - Sato Y, Fukudo S. Gastrointestinal symptoms and disorders in patients with eating disorders. Clin J Gastroenterol. 2015;8(5):255-263.
doi pubmed - Floriano JP, Nahas PC, de Branco FMS, Dos Reis AS, Rossato LT, Santos HO, Limirio LS, et al. Serum uric acid is positively associated with muscle mass and strength, but not with functional capacity, in kidney transplant patients. Nutrients. 2020;12(8):2390.
doi pubmed - Kawamoto R, Ninomiya D, Kasai Y, Kusunoki T, Ohtsuka N, Kumagi T, Abe M. Serum uric acid is positively associated with handgrip strength among japanese community-dwelling elderly women. PLoS One. 2016;11(4):e0151044.
doi pubmed - Picca A, Coelho-Junior HJ, Calvani R, Marzetti E, Vetrano DL. Biomarkers shared by frailty and sarcopenia in older adults: A systematic review and meta-analysis. Ageing Res Rev. 2022;73:101530.
doi pubmed - Zhao L, Cheng J, Chen Y, Li Q, Han B, Chen Y, Xia F, et al. Serum alanine aminotransferase/aspartate aminotransferase ratio is one of the best markers of insulin resistance in the Chinese population. Nutr Metab (Lond). 2017;14:64.
doi pubmed - He Y, Ding F, Yin M, Zhang H, Hou L, Cui T, Xu J, et al. High serum AST/ALT ratio and low serum INS*PA product are risk factors and can diagnose sarcopenia in middle-aged and older adults. Front Endocrinol (Lausanne). 2022;13:843610.
doi pubmed - Ma W, Hu W, Liu Y, He L. Association between ALT/AST and muscle mass in patients with type 2 diabetes mellitus. Mediators Inflamm. 2022;2022:9480228.
doi pubmed - Seko Y, Mizuno N, Okishio S, Takahashi A, Kataoka S, Okuda K, Furuta M, et al. Clinical and pathological features of sarcopenia-related indices in patients with non-alcoholic fatty liver disease. Hepatol Res. 2019;49(6):627-636.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


