| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 9, September 2022, pages 348-356
A Retrospective Study on the Relationship Between Cognitive Function and Social Function in Patients With Schizophrenia
Takamitsu Shimadaa, b, d , Genyo Kobayashib, Yoshihiro Saekib, Chikako Mizukoshib, Kazuo Chikazawab, Katsutoshi Nokurab, Mitsuru Hasegawab, Tamami Maedac, Yoshiki Maedab, c, Yasuhiro Kawasakia
aDepartment of Neuropsychiatry, Kanazawa Medical University, Uchinada, Kahoku-gun, Ishikawa 920-0293, Japan
bMedical Corporation, Sekijinkai Okabe Hospital, Kanazawa, Ishikawa 921-8114, Japan
cMedical Corporation Okabe Clinic, Kanazawa, Ishikawa 921-8025, Japan
dCorresponding Author: Takamitsu Shimada, Department of Neuropsychiatry, Kanazawa Medical University, Uchinada, Kahoku-gun, Ishikawa 920-0293, Japan
Manuscript submitted July 19, 2022, accepted September 12, 2022, published online September 29, 2022
Short title: Factors Affecting Social Functioning
doi: https://doi.org/10.14740/jocmr4798
| Abstract | ▴Top |
Background: Social dysfunction is associated with decreased activity, employment difficulties, and poor prognosis in patients with schizophrenia. Cognitive functions, such as attention and processing speed, have been implicated in the social functions of schizophrenia patients; however, the relationship between cognitive functions and social functions remains unclear. Thus, understanding the factors that influence social functioning can aid the development of therapeutic strategies for schizophrenia. Herein, we retrospectively analyzed factors that influence social functioning in patients with schizophrenia.
Methods: Patient background, intelligence quotient (IQ) scores, Japanese version of the Brief Assessment of Cognition in Schizophrenia (BACS-J) scores, the dose of antipsychotic drugs, Positive and Negative Syndrome Scale (PANSS) scores, and the factors influencing each subscale of the Japanese version of the Social Functioning Scale (SFS-J) were evaluated using univariate and multivariate analyses. The Bonferroni correction was applied to evaluate the correlation between each factor in the univariate analysis. In multivariate analysis, independent variables were selected using a stepwise method. In each model, considering the sample size, the maximum number of variables extracted using the stepwise method was set to three. We then calculated the standard partial regression coefficient (standard β) between the SFS-J subscale scores and each factor.
Results: Data from 36 patients were analyzed. The average age, illness duration, and total length of hospitalization were 57.8 years, 34.8 years, and 196.7 months, respectively. Of the seven significant correlations with the SFS-J subscale in the univariate analysis, only three were significant in the multivariate analysis model. According to the multivariable model, BACS-J verbal fluency positively correlated with SFS-J withdrawal, interpersonal communication, and employment/occupation. Moreover, BACS-J token motor and educational history were positively correlated with SFS-J recreation and SFS-J employment/occupation, respectively. PANSS scores, IQ scores, and doses of antipsychotic drugs did not show clear associations with SFS-J scores.
Conclusions: In conclusion, there were significant correlations between BACS-J subscale scores for cognitive functioning and SFS-J subscale scores for social functioning in patients with schizophrenia.
Keywords: Brief assessment of cognition in schizophrenia; Cognitive function; Social functioning scale; Social function; Schizophrenia
| Introduction | ▴Top |
Schizophrenia is a chronic psychiatric disorder with a relatively high incidence and lifetime prevalence of 0.87% [1]. The core symptoms of schizophrenia include positive symptoms such as hallucinations and delusions, negative symptoms such as decreased motivation and apathy, cognitive dysfunction, and social dysfunction. Social dysfunction refers to an impaired ability to properly perform daily social activities and maintain one’s social life [2], and decreased social functioning has been reported in patients with schizophrenia and mental disorders [3-6]. Notably, social dysfunction is associated with recurrence [7], decreased activity [8], difficulty in employment/occupation [9], increased medical costs [10], and poor prognosis in schizophrenia patients. Thus, understanding the factors that influence social functioning can aid the development of therapeutic strategies for schizophrenia.
Several studies have investigated the cognitive and social functioning of patients with schizophrenia. Improvements in cognitive function have been reported to affect social function in schizophrenia [11-14]. According to Green et al, functional prognosis in schizophrenia is influenced by cognitive functions, such as attention, language, memory, and information processing [15]. Velligan et al reported that the cognitive function of verbal memory affects community outcomes, while executive functioning affects employment/occupation and activities of daily living [16].
The Brief Assessment of Cognition in Schizophrenia (BACS) is a tool used to assess cognitive function in patients with schizophrenia [17-19]. Tominaga et al demonstrated that BACS scores for attention and information processing speed are significantly correlated with social functioning [20]. Additionally, Sumiyoshi et al [21] reported a simple correlation between social functioning as evaluated using the Social Functioning Scale (SFS) [17] and cognitive functioning as evaluated using the BACS. In contrast, Addington et al and Zuo et al found no significant relationship between cognitive and social function in patients with schizophrenia [22, 23]. Furthermore, in a meta-analysis of 73 studies on schizophrenia, Ventura et al reported that the association between cognitive function and functional outcomes in schizophrenia was mediated by the severity of negative symptoms [24]. As described above, there is no consensus on the relationship between cognitive and social functioning in schizophrenia.
Social functioning is affected by various factors, such as age, medication [25, 26], cognitive functions [3], thalamic volume reduction [27], social factors, and lifestyle habits [28]. Green et al reported that 20-60% of the functional prognosis in patients with schizophrenia can be explained by cognitive function [29]. Both cognitive and social functions contain various domains, and there may be links between some domains involved in cognitive and social functioning. Accordingly, we hypothesized that there is a relationship between some domains of cognitive and social functions and conducted a study on patients with schizophrenia.
| Materials and Methods | ▴Top |
Patients
In this retrospective study, we analyzed the data of patients who were admitted to Okabe Hospital from April 2018 to December 2019 and met the diagnostic criteria for schizophrenia as outlined in the Diagnostic and Statistical Manual of Mental Disorders, fifth Edition (DSM-5). All patients included in this study were diagnosed with schizophrenia by at least two experienced psychiatrists. This study included patients with data on sex, age, duration of illness, educational history, length of hospitalization, Positive and Negative Syndrome Scale (PANSS) scores [30, 31], Japanese adult reading test of 50 kanji characters (JART50) scores, a chlorpromazine-equivalent dose of antipsychotic drugs (CPZ-equivalent dose), and Japanese version of the BACS (BACS-J) subscale scores. The exclusion criteria were atypical headache, head injury with loss of consciousness, chronic lung disease, kidney disease, chronic liver disease, active cancer, cerebrovascular disease, thyroid disease, epilepsy, substance-related disorders, steroid use, and intellectual disability.
Ethical considerations
This study was conducted in accordance with the ethical principles of the Declaration of Helsinki and complied with the ethical guidelines for medical research in humans provided by the Ministry of Health, Labor, and Welfare in Japan. This study was approved by the Ethics Committee of Okabe Hospital (approval no. 5: August 5, 2021).
Participants were not required to provide informed consent because this retrospective analysis used anonymous clinical data. We provided an opt-out document on the website of Okabe Hospital to allow the study subjects to decline the use of their data.
Basic data and assessments
Schizophrenia symptoms were evaluated using the PANSS, which includes seven items for positive and negative symptoms and 16 items for general psychopathology [19, 20]. The JART50 was used to perform a premorbid intelligence quotient (IQ) evaluation. Moreover, the JART50 evaluates an individual’s ability to read 50 kanji characters and has been confirmed to be compatible with the Wechsler Adult Intelligence Scale (WAIS-III) [32, 33]. The CPZ-equivalent dose was calculated using the method described by Inada et al [34].
SFS
Social functioning was assessed using the self-reported Japanese version of the SFS (SFS-J) [35]. It assesses social functioning in several areas and is specifically designed for schizophrenia patients [17]. The SFS has seven subscales: 1) withdrawal (time spent alone, initiation of conversation, and social avoidance), with a score range of 0 - 15 points; 2) interpersonal communication (number of friends/having a romantic partner, and quality of communication), with a score range of 0 - 12 points; 3) independence-performance (performance of skills necessary for independent living), with a score range of 0 - 39 points; 4) independence-competence (ability to perform skills necessary for independent living), with a score range of 0 - 39 points; 5) recreation (engagement in a range of common hobbies, interests, pastimes, etc.), with a score range of 0 - 45 points; 6) prosocial activities (engagement in a range of common social activities such as sports), with a score range of 0 - 66 points; and 7) employment/occupation (engagement in productive employment or a structured program with daily activities), with a score range of 0 - 10 points. The total score was the sum of the seven domain scores, ranging from 0 to 226 points. A higher score indicates a higher level of social functioning.
BACS
The BACS-J was used to evaluate cognitive function, and the raw score was converted to a Z-score in accordance with the methods described by Kaneda et al [36, 37]. The BACS battery provides a brief, reliable, and valid test of global neuropsychological function [18, 19] and is widely used in schizophrenia research [38]. The BACS battery consists of six subtests: 1) verbal memory, with a score range of 0 - 75 points; 2) digit sequencing (working memory), with a score range of 0 - 28 points; 3) token motor (motor speed), with a score range of 0 - 100 points; 4) verbal fluency, with a score range of 0 - Inf; 5) symbol coding (attention), with a score range of 0 - 110 points; and 6) tower of London (executive function), with a score range of 0 - 22 points. All tests were scored by two trained occupational therapists at Okabe Hospital.
Statistical analysis
Descriptive statistics are expressed as n (%) and mean ± standard deviation. Spearman correlation coefficients were used to evaluate the correlation between SFS-J scores and each variable. In the univariate analysis, Bonferroni correction was applied to reduce the risk of type I errors when assessing correlations. Moreover, the correlation between each variable and the SFS-J score was also examined using the standard partial regression coefficient (standard β). To assess standard β values, multiple regression analysis was performed using variables extracted from the following via a stepwise method: age, sex, educational history, duration of illness, the total length of hospitalization, PANSS scores on each subscale (positive and negative symptoms, comprehensive psychopathology), JART50 scores, CPZ-equivalent dose, and BACS-J subscale scores (verbal memory, digit sequencing, token motor, verbal fluency, symbol coding, and tower of London). In model 1, age, sex, educational history, duration of illness, the total length of hospitalization, JART50 score, and BACS-J score were included as independent variables. In model 2, all variables from model 1 were included along with a CPZ-equivalent dose. Model 3 included all variables from model 2 as well as the PANSS scores. We then calculated the degrees-of-freedom-adjusted R2 for the SFS-J subscales that were significantly related to the various variables in model 3. In each model, considering the sample size, the maximum number of variables extracted using the stepwise method was set to three. The significance level was set at < 0.05 on both sides. JMP ver. 13.2.1 was used for statistical analysis.
| Results | ▴Top |
Patient background characteristics
Of 148 inpatients with schizophrenia during the target period, 28 were excluded based on our initial exclusion criteria. Among the remaining 120 cases, 84 were excluded due to incomplete data, while the remaining 36 were analyzed (Fig. 1). The patients’ background characteristics are presented in Table 1. The average age, illness duration, and total length of hospitalization were 57.8 years, 34.8 years, and 196.7 months, respectively.
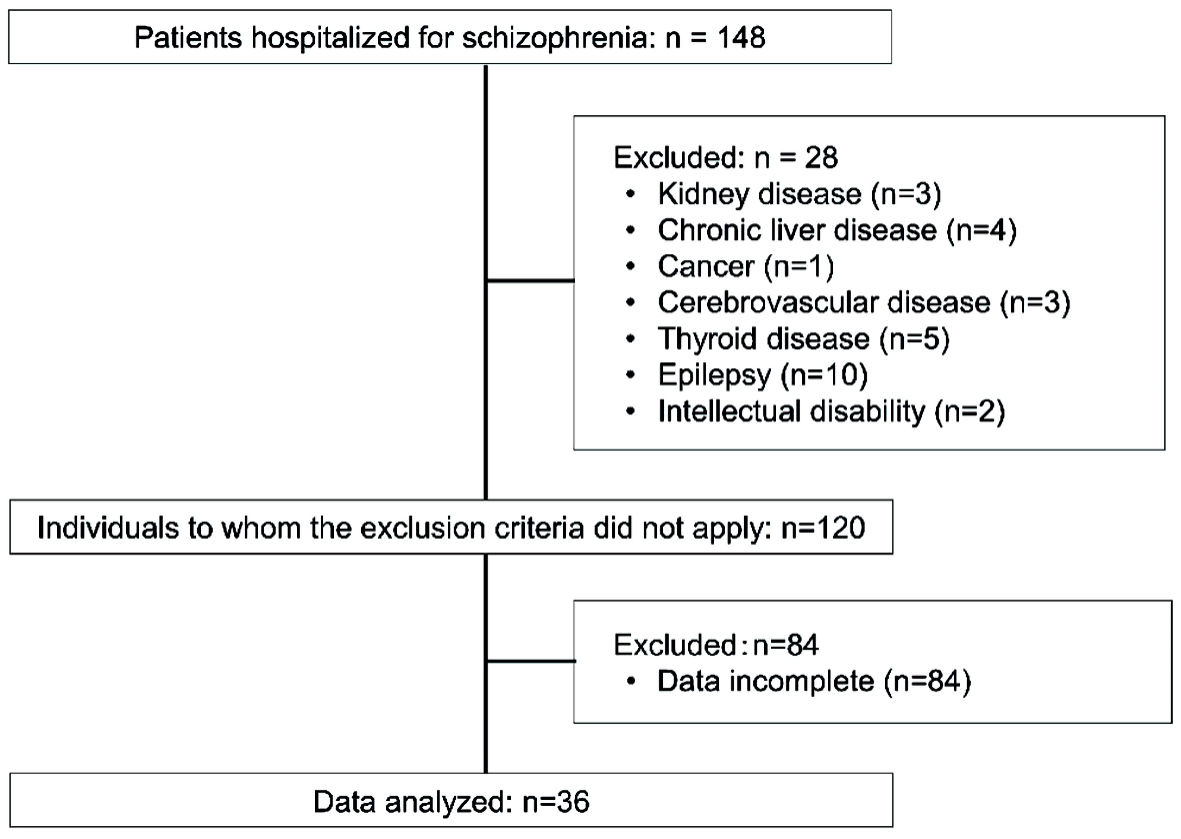 Click for large image | Figure 1. Flowchart of patient selection. |
 Click to view | Table 1. Demographic Variables |
Correlations between SFS-J scores and each variable
Bonferroni correction with a comparison number of 16 was applied to the P value of each correlation. The total length of hospitalization was negatively correlated with the SFS-J independence performance (r = -0.7119), independence-competence (-0.6086), recreation (-0.5385), and the total score (-0.6861) (Table 2). BACS-J verbal fluency was positively correlated with SFS-J withdrawal (0.6893) and employment/occupation (0.7239), and the tower of London was positively correlated with independence-performance (0.6941), independence-competence (0.7377), and the total score (0.7546). Furthermore, the BACS-J mean was positively correlated with the SFS-J total score (0.698).
 Click to view | Table 2. Correlations Between SFS-J Subscales and Clinical Variables |
Factors associated with SFS-J scores
There was a positive relationship between age and the SFS-J independence competence in models 2 and 3 (Table 3). All models showed positive relationships between educational history and SFS-J employment/occupation. The total length of hospitalization was negatively correlated with the SFS-J independence-performance and independence-competence in model 1, recreation in models 1 and 3, and total score in model 1. There was a positive relationship between the BACS-J token motor and SFS-J recreation in all models. Moreover, all models showed positive relationships between BACS-J verbal fluency and SFS-J withdrawal, interpersonal communication, and employment/occupation. No relationship was observed between BACS-J and SFS-J domains other than the above.
 Click to view | Table 3. Standard Partial Regression Coefficients for Each Variable and the SFS-J |
Table 4 shows the results of multiple regression analysis that showed a significant association with the SFS subscales in model 3. The degrees-of-freedom-adjusted R2 values for each model ranged from 0.271 to 0.623, indicating that each combination of independent variables had an impact on each subscale of the SFS.
 Click to view | Table 4. Effects of Each Factor in Model 3 on SFS-J Subscales |
| Discussion | ▴Top |
This retrospective study investigated the relationship between cognitive and social function domains in patients with schizophrenia. In univariate analysis, 10 variables exhibited a significant correlation with any subscale of the SFS-J. In the multivariate analysis, nine variables exhibited such correlations in model 1, six in model 2, and seven in model 3. Of the 10 significant correlations with the SFS-J subscale in the univariate analysis, only three were found to be significant in the multivariate analysis of model 3. These results suggest that various factors influence each other, making it difficult to determine their true relationship. In this study, the results from multiple regression models suggest BACS-J verbal fluency positively correlated with SFS-J withdrawal, interpersonal communication, and employment/occupation; a positive relationship between BACS-J token motor and SFS-J recreation; and a positive relationship between educational history and SFS-J employment/occupation. Besides the above domains, no relationship between cognitive and social functions was observed.
According to Tominaga et al, BACS symbol coding (processing speed) was associated with the total social functioning score, but not other cognitive domains [20]. Santosh et al reported that among cognitive functions, executive function, verbal working memory, attention, and verbal fluency are related to social functions [39]. These findings indicate that only some domains of cognitive function are related to the social function subscales, which is in line with our study. Similar to the results of our study, Bowie et al reported a significant relationship between vocabulary/language skills and interpersonal relationships in patients with schizophrenia [40]. Iwata et al reported a significant correlation between verbal fluency and interpersonal relationships in schizophrenia patients [41]. These reports are consistent with the results of our study and suggest a relationship between verbal fluency and social isolation and interpersonal relationships in patients with schizophrenia.
Moreover, this study revealed a relationship between verbal fluency and employment. A study conducted by Kang et al reported a significant correlation between the Schizophrenia Cognitive Rating Scale and the Social and Occupational Functioning Assessment Scale in patients with schizophrenia [42]. Furthermore, McGurk et al conducted cognitive function training for patients with severe psychiatric disorders, mainly schizophrenia, and found that the employment rate of the training group was significantly higher than the non-training group after 1 year [12]. The results of this study are consistent with the previous report demonstrating a relationship between cognitive function and employment. Previous studies have reported that verbal and nonverbal fluency affects divergent thinking in schizophrenia [43, 44]. Other studies have suggested that impairments in divergent thinking may be associated with impaired interpersonal communication and impaired social function [45]. This may be because impairments in verbal fluency can make verbal communication more difficult in patients with schizophrenia. Similarly, impaired verbal fluency may affect employment/occupation through impairments in verbal communication. These findings suggest the importance of verbal fluency in the social functioning of patients with schizophrenia.
Our analysis also indicated a positive relationship between the BACS-J token motor and SFS-J recreation. Previous studies have demonstrated a relationship between psychomotor skills and social problem-solving abilities [15]. Furthermore, Akiyama et al reported that the token motor task of the cognitive function evaluated using the BACS correlated with the SFS total score [46]. SFS-J recreation scores are based on basic daily activities, such as reading books, cooking, sewing, walking, playing games, and artistic/creative activities. Decreases in motor function may be related to decreases in work speed, which can affect activities such as sewing, playing games, and artistic activities. To our knowledge, the present study is the first to report a significant relationship between the BACS token motor and SFS recreation.
Social functioning is divided into intrapersonal and interpersonal functioning, which involve internal and external motivation, respectively [47]. SFS withdrawal and interpersonal relationships correspond to interpersonal functioning, while SFS recreation corresponds to intrapersonal functioning [47]. The results of our study indicate that cognitive function may be related to both interpersonal and intrapersonal functioning depending on the cognitive domain. However, the fact that the relationship between cognitive function and social function was limited to some subscales may be due to the lack of consideration of motivational data.
In this study, educational history positively associated with SFS-J employment/occupation. In school settings, cooperation and sociality are fostered through communication and other activities. Patients with limited education may face difficulties in employment owing to a decrease in opportunities to foster sociality. Additionally, a short educational history may lead to a decline in the abilities and skills required for employment. In contrast, SFS-J scores are not affected by the duration of illness or hospitalization, suggesting that social dysfunction in patients with schizophrenia is a core symptom that arises from the time of onset [4].
This study had several limitations. First, only 36 cases were included, and the sample size may have limited the scope of our analysis. Second, the variables included in the multivariate analysis were selected using a stepwise method under the limit of a maximum of three independent variables. Third, all patients were inpatients, and their characteristics may differ from those of the general population of schizophrenia patients. In schizophrenia, motivation has been believed to be an intervening factor between cognitive and social functioning [47], yet motivation was not taken into account in this study. Finally, no sample-size estimation was performed in this study. The results of this study should be interpreted considering these factors.
Conclusions
Under the examination conditions, significant relationships between BACS-J verbal fluency and SFS withdrawal, interpersonal communication, and employment/occupation were observed, as well as between BACS-J token motor and SFS recreation.
Acknowledgments
We would like to thank all participants of this study.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Participants were not required to provide informed consent because this retrospective analysis used anonymous clinical data. We provided an opt-out document on the website of Okabe Hospital to allow the study subjects to decline the use of their data.
Author Contributions
Takamitsu Shimada contributed to the conception and design of the study, wrote the first draft of the manuscript, and contributed to the editing of the final manuscript. Genyo Kobayashi, Yoshihiro Saeki, Chikako Mizukoshi, Kazuo Chikazawa, Katsutoshi Nokura, Mitsuru Hasegawa, Tamami Maeda, Yoshiki Maeda and Yasuhiro Kawasaki were involved in the literature review and corrections. All authors have read and approved the final manuscript.
Data Availability
Any inquiries regarding supporting data availability in this study should be directed to the corresponding author.
| References | ▴Top |
- Perala J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsa E, Pirkola S, Partonen T, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64(1):19-28.
doi pubmed - Gu Y, Peng H, Dai J, Gao H, Yang X, Sheng J, Zhang C. Evaluation of paliperidone on social function in patients with chronic schizophrenia. Gen Psychiatr. 2018;31(2):e000011.
doi pubmed - Yasuyama T, Ohi K, Shimada T, Uehara T, Kawasaki Y. Differences in social functioning among patients with major psychiatric disorders: Interpersonal communication is impaired in patients with schizophrenia and correlates with an increase in schizotypal traits. Psychiatry Res. 2017;249:30-34.
doi pubmed - Grant C, Addington J, Addington D, Konnert C. Social functioning in first- and multiepisode schizophrenia. Can J Psychiatry. 2001;46(8):746-749.
doi pubmed - Porcelli S, Van Der Wee N, van der Werff S, Aghajani M, Glennon JC, van Heukelum S, Mogavero F, et al. Social brain, social dysfunction and social withdrawal. Neurosci Biobehav Rev. 2019;97:10-33.
doi pubmed - Chen P, Hong W. Neural circuit mechanisms of social behavior. Neuron. 2018;98(1):16-30.
doi pubmed - Rajkumar S, Thara R. Factors affecting relapse in schizophrenia. Schizophr Res. 1989;2(4-5):403-409.
doi - Ohi K, Kataoka Y, Shimada T, Kuwata A, Okubo H, Kimura K, Yasuyama T, et al. Meta-analysis of physical activity and effects of social function and quality of life on the physical activity in patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2019;269(5):517-527.
doi pubmed - Johnstone EC, Macmillan JF, Frith CD, Benn DK, Crow TJ. Further investigation of the predictors of outcome following first schizophrenic episodes. Br J Psychiatry. 1990;157:182-189.
doi pubmed - McCrone P, Thornicroft G, Parkman S, Nathaniel-James D, Ojurongbe W. Predictors of mental health service costs for representative cases of psychosis in south London. Psychol Med. 1998;28(1):159-164.
doi pubmed - Harvey PD, Balzer AM, Kotwicki RJ. Training engagement, baseline cognitive functioning, and cognitive gains with computerized cognitive training: A cross-diagnostic study. Schizophr Res Cogn. 2020;19:100150.
doi pubmed - McGurk SR, Mueser KT, Pascaris A. Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial. Schizophr Bull. 2005;31(4):898-909.
doi pubmed - Barlati S, Deste G, De Peri L, Ariu C, Vita A. Cognitive remediation in schizophrenia: current status and future perspectives. Schizophr Res Treatment. 2013;2013:156084.
doi pubmed - Dubreucq J, Gabayet F, Ycart B, Faraldo M, Melis F, Lucas T, Arnaud B, et al. Improving social function with real-world social-cognitive remediation in schizophrenia: Results from the RemedRugby quasi-experimental trial. Eur Psychiatry. 2020;63(1):e41.
doi pubmed - Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72(1):41-51.
doi pubmed - Velligan DI, Bow-Thomas CC, Mahurin RK, Miller AL, Halgunseth LC. Do specific neurocognitive deficits predict specific domains of community function in schizophrenia? J Nerv Ment Dis. 2000;188(8):518-524.
doi pubmed - Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The Social Functioning Scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853-859.
doi pubmed - Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68(2-3):283-297.
doi pubmed - Keefe RS, Harvey PD, Goldberg TE, Gold JM, Walker TM, Kennel C, Hawkins K. Norms and standardization of the Brief Assessment of Cognition in Schizophrenia (BACS). Schizophr Res. 2008;102(1-3):108-115.
doi pubmed - Tominaga T, Tomotake M, Takeda T, Ueoka Y, Tanaka T, Watanabe SY, Kameoka N, et al. Relationship between social and cognitive functions in people with schizophrenia. Neuropsychiatr Dis Treat. 2018;14:2215-2224.
doi pubmed - Sumiyoshi T, Nishida K, Niimura H, Toyomaki A, Morimoto T, Tani M, Inada K, et al. Cognitive insight and functional outcome in schizophrenia; a multi-center collaborative study with the specific level of functioning scale-Japanese version. Schizophr Res Cogn. 2016;6:9-14.
doi pubmed - Addington J, McCleary L, Munroe-Blum H. Relationship between cognitive and social dysfunction in schizophrenia. Schizophr Res. 1998;34(1-2):59-66.
doi - Zuo S, Byrne LK, Peng D, Mellor D, McCabe M, Zhang J, Huang J, et al. Symptom severity is more closely associated with social functioning status in inpatients with schizophrenia than cognitive deficits. Shanghai Arch Psychiatry. 2012;24(2):83-90.
- Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113(2-3):189-199.
doi pubmed - Dutescu MM, Popescu RE, Balcu L, Duica LC, Strunoiu LM, Alexandru DO, Pirlog MC. Social functioning in schizophrenia clinical correlations. Curr Health Sci J. 2018;44(2):151-156.
- Ohnishi T, Kobayashi H, Yamaoka T, Toma T, Imai K, Wakamatsu A, Noguchi K. The effects of paliperidone palmitate 1 month on the employment status and social functioning of patients with schizophrenia. Innov Clin Neurosci. 2020;17(1-3):36-44.
- Koshiyama D, Fukunaga M, Okada N, Yamashita F, Yamamori H, Yasuda Y, Fujimoto M, et al. Role of subcortical structures on cognitive and social function in schizophrenia. Sci Rep. 2018;8(1):1183.
doi pubmed - Porcelli S, Kasper S, Zohar J, Souery D, Montgomery S, Ferentinos P, Rujescu D, et al. Social dysfunction in mood disorders and schizophrenia: Clinical modulators in four independent samples. Prog Neuropsychopharmacol Biol Psychiatry. 2020;99:109835.
doi pubmed - Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophr Bull. 2000;26(1):119-136.
doi pubmed - Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261-276.
doi pubmed - Igarashi Y, Hayashi N, Yamashina M, Otsuka N, Kuroki N, Anzai N, Kazamatsuri H. Interrater reliability of the Japanese version of the Positive and Negative Syndrome Scale and the appraisal of its training effect. Psychiatry Clin Neurosci. 1998;52(5):467-470.
doi pubmed - Matsuoka K, Uno M, Kasai K, Koyama K, Kim Y. Estimation of premorbid IQ in individuals with Alzheimer's disease using Japanese ideographic script (Kanji) compound words: Japanese version of National Adult Reading Test. Psychiatry Clin Neurosci. 2006;60(3):332-339.
doi pubmed - Fujino H, Sumiyoshi C, Sumiyoshi T, Yasuda Y, Yamamori H, Ohi K, Fujimoto M, et al. Performance on the Wechsler Adult Intelligence Scale-III in Japanese patients with schizophrenia. Psychiatry Clin Neurosci. 2014;68(7):534-541.
doi pubmed - Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry Clin Neurosci. 2015;69(8):440-447.
doi pubmed - Nemoto T, Fujii C, Miura Y, Chino B, Kobayashi H, Yamazawa R, Murakami M, et al. Reliability and validity of the Social Functioning Scale Japanese version (SFS-J). Jpn Bull Soc Psychiatry. 2008;17:188-195. (in Japanese)
- Kaneda Y, Sumiyoshi T, Keefe R, Ishimoto Y, Numata S, Ohmori T. Brief assessment of cognition in schizophrenia: validation of the Japanese version. Psychiatry Clin Neurosci. 2007;61(6):602-609.
doi pubmed - Kaneda Y, Sumiyoshi T, Nakagawa K, Ikezawa S, Oomori T, Furukori N, Kunugi H, et al. Evaluation of cognitive functions in a normal population in Japan using the brief assessment of cognition in schizophrenia Japanese version (BACS-J). Psychiatry. 2013;55:167-175. (in Japanese)
- Masuzawa T, Hashimoto T, Yotsumoto K. Subjectively-assessed cognitive impairment and neurocognition associations in schizophrenia inpatients. Schizophr Res Cogn. 2022;27:100218.
doi pubmed - Santosh S, Dutta Roy D, Kundu PS. Psychopathology, cognitive function, and social functioning of patients with schizophrenia. East Asian Arch Psychiatry. 2013;23(2):65-70.
- Bowie CR, Harvey PD. Communication abnormalities predict functional outcomes in chronic schizophrenia: differential associations with social and adaptive functions. Schizophr Res. 2008;103(1-3):240-247.
doi pubmed - Iwata K, Matsuda Y, Sato S, Furukawa S, Watanabe Y, Hatsuse N, Ikebuchi E. Efficacy of cognitive rehabilitation using computer software with individuals living with schizophrenia: A randomized controlled trial in Japan. Psychiatr Rehabil J. 2017;40(1):4-11.
doi pubmed - Kang EC, Kim SJ, Seo YS, Jung SS, Seo BJ, Ryu JW, Shim JC, et al. The Korean version of the schizophrenia cognition rating scale: reliability and validity. Psychiatry Investig. 2017;14(2):141-149.
doi pubmed - Nemoto T, Mizuno M, Kashima H. Qualitative evaluation of divergent thinking in patients with schizophrenia. Behav Neurol. 2005;16(4):217-224.
doi pubmed - Yamashita C, Mizuno M, Nemoto T, Kashima H. Social cognitive problem-solving in schizophrenia: associations with fluency and verbal memory. Psychiatry Res. 2005;134(2):123-129.
doi pubmed - Nemoto T, Kashima H, Mizuno M. Contribution of divergent thinking to community functioning in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31(2):517-524.
doi pubmed - Akiyama K, Saito S, Saito A, Ozeki Y, Watanabe T, Fujii K, Honda G, et al. Predictive value of premorbid IQ, negative symptoms, and age for cognitive and social functions in Japanese patients with schizophrenia: A study using the Japanese version of the Brief Assessment of Cognition in Schizophrenia. Psychiatry Res. 2016;246:663-671.
doi pubmed - Uchino T, Nemoto T, Kojima A, Takubo Y, Kotsuji Y, Yamaguchi E, Yamaguchi T, et al. Effects of motivation domains on social functioning in schizophrenia with consideration of the factor structure and confounding influences. J Psychiatr Res. 2021;133:106-112.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


