| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 14, Number 5, May 2022, pages 177-187
Obesity and the Other Independent Predictors in Elective Endotracheal Tube Intubations: A Narrative Review
Lakshmi Rekha Narraa, Ndausung Udongwoa, f, Jerry Lorren Dominicb, Shriya Doreswamyc, Anam Bhasird, Islam Elkherpitawya, Chinwe Ogedegbee
aDepartment of Internal Medicine, Jersey Shore University Medical Center, Neptune City, NJ, USA
bDivision of Critical Care and Trauma Surgery, Department of General Surgery, DHR Health Institute for Research and Development, Edinburg, TX, USA
cDepartment of Internal Medicine, Einstein Medical Center, Montgomery, PA, USA
dDepartment of Internal Medicine, Foundation University Medical College, Islamabad, Pakistan
eDepartment of Emergency Medicine, Hacekensack University Medical Center, Hackensack, NJ, USA
fCorresponding Author: Ndausung Udongwo, Department of Internal Medicine, Jersey Shore University Medical Center, Neptune City, NJ 077543, USA
Manuscript submitted April 16, 2022, accepted April 30, 2022, published online May 31, 2022
Short title: Risk Predictors of Difficult Airway in Obesity
doi: https://doi.org/10.14740/jocmr4727
- Abstract
- Introduction
- Methods
- Classification of Obesity
- Definitions of Difficult Airway and Difficult Intubation
- Assessing the Risk Factors for Difficult Airway and Intubations
- Discussion
- Limitations
- Conclusions
- References
| Abstract | ▴Top |
Obesity is one of the challenging elements in health care. Studies have shown that as the body mass index (BMI) increases, the risk of chronic conditions tends to increase due to altered physiologic and metabolic demands. In addition to underlying physiological changes, anatomical changes can lead to common procedural challenges, such as difficult intravenous (IV) cannulation, difficult airway, and difficult intubation, which makes their preoperative and postoperative care challenging for the anesthesiologists. According to previous studies, there is no single best predictor for difficult airway or intubations and no designed protocol for choosing an intubation technique in obese patients. Some of the preoperative risk factors and techniques such as the modified Mallampati class, sternomental distance, thyromental distance, neck circumference, indirect mirror laryngoscopy, BMI, and intraoperative risk factors such as inappropriate positioning of the patient, suboptimal medication dosing, inappropriate laryngoscopy device acted as independent predictors for difficult airway and difficult intubation. Analyzing each element’s importance and making suitable decisions for the individual will reduce the complications and prepare for unplanned emergencies in the operating room. This review is convincing with previous studies that obesity itself is not an independent predictor. Instead, as a preoperative risk factor, and till date, sternomental distance and the number of intubation attempts were demonstrated as significant independent predictors for adverse events. All the other independent factors and considerations were discussed, which can help with further research.
Keywords: Obesity; Intubation; Body mass index; Mallampati score; Difficult airway; Intubation difficulty scale
| Introduction | ▴Top |
Nearly more than a third of the world’s population is affected by obesity [1]. It is the most common risk factor for chronic conditions such as hypertension, diabetes, coronary artery disease, and hyperlipidemia. It predisposes to other comorbidities such as malignancies, cerebrovascular accidents, and increased mortality [2]. Certain sub-specialties such as emergency medicine and anesthesiology face common procedural challenges in obese individuals, including intravenous (IV) cannulations and endotracheal intubations. In this review, we focused on factors affecting endotracheal tube intubations in obese individuals. Many studies have shown that considering certain factors before intubation may ease unplanned scenarios and complications. In previous literatures, it is noticed that obesity itself is not a sole independent predictor, instead, several other factors play a role in difficult intubations [3, 4]. This article’s primary goal is to emphasize research gaps, the significance of bedside clinical scores, and grades despite their limitations, examine their importance before choosing intubation techniques and summarizing statistically and clinically effective methods that reduced the number of failed intubations attempts and post-intubation complications [5].
| Methods | ▴Top |
Data were collected from online databases specifically PubMed, PubMed Central, British Journal of Anesthesia, American Society of Anesthesiologists (ASA) website, Google Scholar, and Up to date. MeSH/keywords used were ((“Obesity” (MeSH) AND “Intubation, Intratracheal” (MeSH)) AND (“Intubation, Intratracheal/Adverse Effects” (MeSH)) OR “Intubation, Intratracheal/Complications” (MeSH)). The total number of articles yielded was 91. Inclusion criteria: human adults > 18 years of age. In our final paper, we were able to use 50 papers relevant to the article title, which included randomized control trials, review articles, prospective and retrospective observational studies, multicenter prospective observational studies.
| Classification of Obesity | ▴Top |
“Obesity is defined as excessive fat accumulation which acts as a risk factor to health”, and body mass index (BMI) is a major tool used worldwide for classifying the severity of obesity [1]. “BMI is known as an individual’s body weight divided by height in square meters” [1]. Although it has its limitations, as it cannot determine an individual’s body fat percentage, it is easy to use as a diagnostic tool in measuring the severity of obesity [1]. According to the studies, cut-off values for BMI are given in Table 1 [6].
 Click to view | Table 1. Commonly Used Cut-Off Values for BMI |
| Definitions of Difficult Airway and Difficult Intubation | ▴Top |
Many studies have outcomes that depend upon the definition of difficult airway and intubation, also depend on anesthesiologists’ understanding of difficult intubation. Defining a difficult airway is challenging. According to the ASA, it is defined as a clinical scenario where a well-trained anesthesiologist has complex issues with facemask ventilation or direct laryngoscopy, or tracheal intubation [7]. According to the ASA, the 2003 updated definition of difficult tracheal intubation reads “when insertion of the endotracheal tracheal tube with conventional laryngoscopy requires repeated attempts” [8].
| Assessing the Risk Factors for Difficult Airway and Intubations | ▴Top |
It is a well-known fact that specific clinical scores and predictors can be used in obese individuals while evaluating and classifying the degree of risk of difficult airway and intubation. Some of them can be performed besides, whereas others can be achieved and correlated in the operating room.
Preoperative bedside evaluation
Traditional preoperative measurements include modified Mallampati classification (MMS), performed in all the individuals who are scheduled for elective surgery [9, 10]. MMS is inclusive of four classes, and its significance is described later in this review.
MMS
Class I: complete visualization of the palate, including hard and soft, uvula, and faucial pillars. Class II: cranial part of faucial pillars, hard and soft palate, the entire uvula is visible. Class III: visualization of the entire palate (hard and soft) and root of the uvula only. Class IV: visualization of hard palate only.
Other independent preoperative factors
According to the studies evaluated, it is noticed that other than MMS and extended Mallampati class (EMS), the following factors are considered independent predictors that played a role in predisposing the individuals for difficult airway and intubation [11]: 1) large neck circumference [12]; 2) short thyromental distance (TMD) [10, 13]; 3) short sternomental distance (SMD) [12]; 4) thick tongue/fat accumulation in cheeks, and minimal mobility of neck and jaw [12]; 5) view seen in indirect mirror laryngoscopy (IML) [14].
Intraoperative correlation and assessment
Although there are no precise scales to re-evaluate the patient in the operating room, certain classifications and scales can still be used to correlate the significance of risk factors in difficult airways and intubations. The most commonly used classification includes Cormack-Lehane classification, which categorizes airway view under direct laryngoscopy. Apart from the traditional Cormack and Lehane grading system, the intubation difficulty scale (IDS), which includes seven characteristics, is being used by many providers to correlate the difficult airway.
Cormack-Lehane classification for direct laryngoscopy view
The Cormack-Lehane classification [15] includes grade 1, entire glottis is visualized; grade 2, glottis or arytenoids are partially visualized (2(a), glottis is partially visualized; 2(b), arytenoids are visualized); grade 3, visualization of epiglottis only; and grade 4, none of them are visible.
IDS
Difficulty in intubation is considered if it meets at least five characteristics [16]: 1) number of intubation attempts; 2) additional operators; 3) substitutable intubation techniques; 4) position and mobility of the vocal cords; 5) Cormack and Lehane’s laryngoscopy grade; 6) use of external laryngeal pressure; 7) a requirement of lifting force with the laryngoscope. Anything below < 5 is considered to be easy to intubate.
| Discussion | ▴Top |
Unsuccessful intubation can lead to complications like post-intubation hematomas, vocal cord injuries, and tracheal ruptures. While managing the difficult airway in obese individuals, they are more prone to a severe drop in oxygen saturation due to low residual capacity or esophageal intubation with delayed recognition. These predispose to post-intubation hypoxemia, dysrhythmia, and cardiac arrest are the most challenging adverse events leading to perioperative morbidity and mortality. Despite an enormous amount of research, no precise predictors for difficult airway or a protocol for choosing an intubation technique in obese patients have been established. Choosing a technique by analyzing perioperative and intraoperative factors and having an alternative method for unplanned scenarios will reduce the intraoperative and postoperative complication rates in those specific populations. Over the years, there has been several articles published on the risk factors associated with difficult intubation (Table 2) [5, 12, 13, 17-23].
 Click to view | Table 2. The Studies Mentioned in the Manuscript With Each Independent Study Result and the Significance of Risk Factors in Difficult Intubations |
In this review, we precisely summarize the criteria that should be considered in choosing the intubation technique for overweight and obese patients. Primarily we divided the considerations into two categories: 1) preoperative risk factors and predictors; and 2) intraoperative risk factors and considerations (Fig. 1) [5, 12, 14, 17, 20, 21, 24-28].
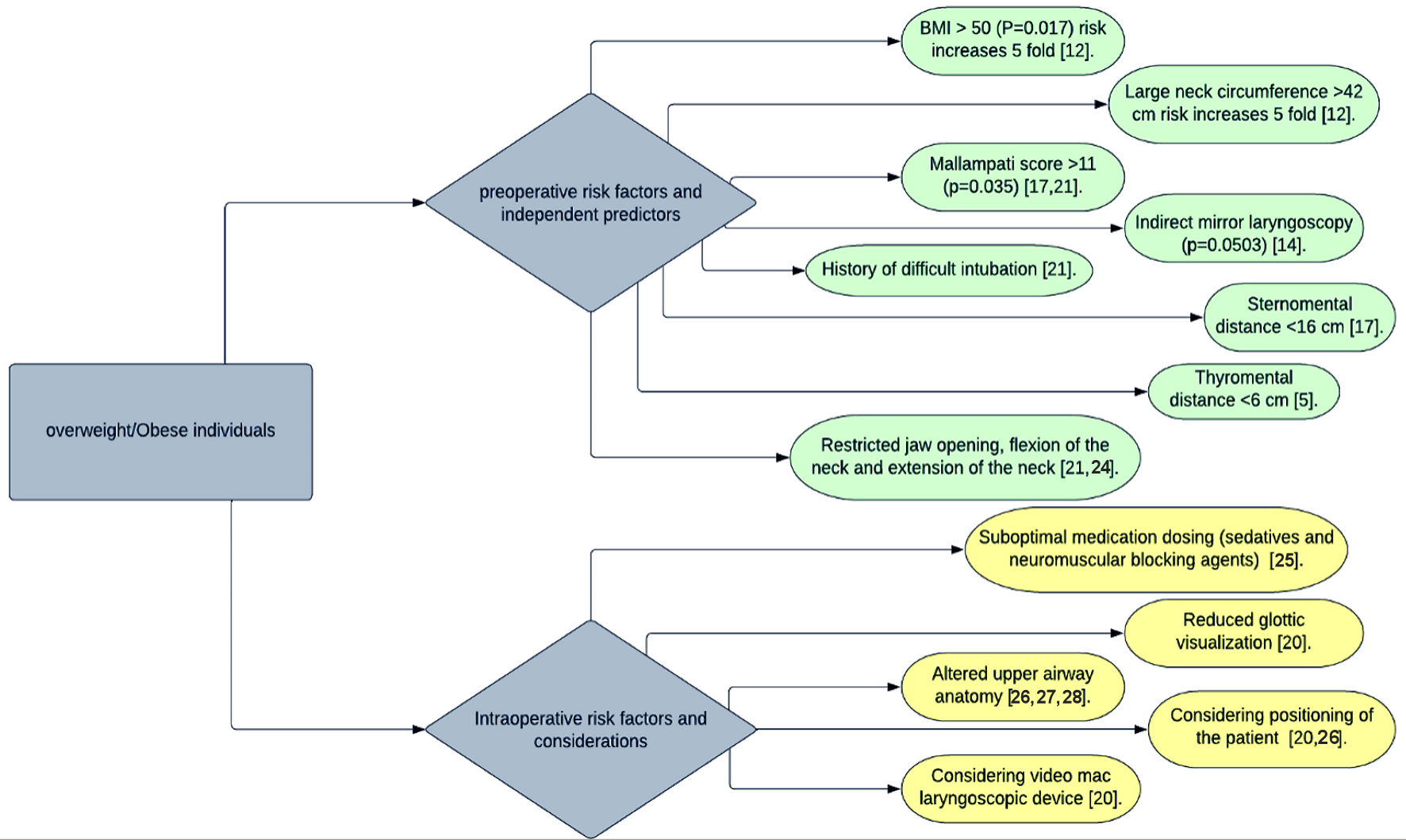 Click for large image | Figure 1. Diagram illustrating preoperative and intraoperative risk factors of intubation in overweight/obese individuals. |
Preoperative risk analysis
Mallampati score
Mallampati score is a noninvasive score first introduced in 1985 by Mallampati, which has three grading classes initially [29]. It measures the disproportion of the tongue size to pharyngeal size. To date, it has been used as a standard test with some modifications in assessing the airway. Most providers use a modified version by Samsoon and Young, including four grades of MMS. They are assigned according to the degree of tongue masking the visibility of pharyngeal structures [29]. It is considered that Mallampati grading III and IV are challenging to intubate, whereas I and II are easy.
A study was done by Juvin et al [30] stated that MMS grade III and IV has been shown as the only independent predictive risk factor for difficult intubation. Still, the specificity remains at 62%, and the positive predictive value remains at 29%. In contrast, a study done by Mashour et al [11] and reviewed by Walls et al [31] stated that despite the reduction in Mallampati grading while evaluating on craniocervical extension (P < 0.0001), EMS has improved the prediction for difficult laryngoscopy with an increase in specificity from 76% to 83%, while sensitivity remains the same. Therefore, studies have recommended the EMS test in the traditional evaluation [11, 31]. Conversely, a study was done by Menon et al [32] stated that there is no significant difference between EMS and MMS. The potential limitation in this finding does not correlate with the Cormack-Lehane classification [32]. Despite the studies done by Hanouz et al [33] and Ouchi et al [34], these are not performed solely in obese individuals. Results have shown that modified Mallampati test (MMT) evaluated in the supine position, has a superior hand in correlating with the Cormack-Lehane classification [33, 34]. In addition, the study of Ouchi et al [34] has shown MMT with tongue protrusion, supine position, and phonation has shown a significant correlation (P = 0.004) with the Cormack-Lehane test.
Mallampati score is the vital predictor for difficult airways, but it is not always consistent as per the studies reviewed. More studies and research are needed to analyze EMS’s predictability compared to MMS, specifically obese individuals [11, 29, 33, 34]. Although there are other scores such as Wilson’s score and intubation prediction score used in predicting the difficult intubation, their sensitivity and specificity become challenging, and there is not enough evidence to conclude that applying other scores would increase the predictability outcomes in obese individuals.
SMD and TMD
Besides MMS, SMD and TMD have significant predictive value in anticipating difficult airways. SMD is measured from the suprasternal notch to the mentum with mouth closed and head extended position. In contrast, TMD is the distance between the mentum and the top of the thyroid cartilage’s notch [22]. Despite TMD’s inaccuracy, it is still considered an independent risk factor in preoperative risk analysis as it can indicate the mandibular space. It helps determine the laryngeal axis (LA) alignment within the pharyngeal axis (PA) when the atlanto-occipital joint is extended [35].
As SMD indicates neck mobility, studies have shown that shorter distances lead to potential difficulty in intubation and laryngoscopies [36]. For instance, in studies done by Ozdilek et al [17] and Cierniak et al [5], it has been shown that SMD of < 16 cm and < 12 cm has been noted to be independent predictors for difficult airways. Also, Cierniak et al [5] have demonstrated that TMD < 6 cm has resulted in a difficult airway in obese patients. As the precise cut-off values are still inconclusive and observed to be individualized for each observed study, both SMD and TMD can lead to a wide range of sensitivity and specificity.
Despite the limitations to the sensitivity and specificity, studies have shown that combining tests such as MMS with SMD and TMD would lead to higher predictive value and validity than that of SMD and TMD alone [37]. Although this helps and alerts physicians for anticipated difficulties, they do not play a significant role in choosing the appropriate intubation technique. In recent times, TMD is receiving significant challenges from authors who think that TMD is not the real cause for difficult laryngoscopy in obese patients and state that TMD can be irrelevant [38]. Although SMD’s shorter distance would result in limited neck mobility, the predictive bedside tests have always been inconclusive. Further research is required for the applicability of these tests to improve the prediction of difficult intubation.
Neck circumference
In recent times besides the traditional predictors, neck circumference has been shown as a positive factor for anticipated difficult airway. Studies done by Riad et al [12], Gonzalez et al [13], and Brodsky et al [22] stated a linear correlation between neck circumference and difficult airway. Convincingly, Riad et al [12] and Gonzalez et al [13] have stated that neck circumference > 43 cm has a linear correlation (P = 0.044); and the results of Brodsky et al [22] have shown neck circumference > 40 - 60 cm has shown increased 5-fold risk in difficult intubation. Although the positive correlation is a driving factor to measure neck circumference, a study done by Siriussawakul et al [39], and Kim et al [10] stated that the ratio of neck circumference to TMD has significantly improved the prediction for difficult laryngoscopy and difficult intubation instead of neck circumference alone. Limited evidence has been there to emphasize the neck circumference, and the results have been inconclusive. There are not enough studies to prove the precise measurement as factors such as gender, and the racial difference can play a role. Further research is required to specify the accurate neck circumference measurement and get the precise measurement to anticipate the difficult airway. Although it may not be a single best reliable predictor, this can still be measured in addition to the existent predictors to improve the prediction of the difficult airway.
IML
In recent advances, a preoperative ultrasound of the neck and invasive airway assessment with fiberoptic bronchoscope is considered in high-risk individuals before elective intubation, as they can precisely visualize the airway’s complexity. On the other hand, the cost of the procedure and its invasiveness can be challenging. A Study done by Budde et al stated that compared to BMI, Wilson score, neck circumference, Mallampati score, and IML, IML has demonstrated statistical significance (P = 0.0503) in predicting a difficult airway. In contrast, other factors were close to (P = 0.0952) [14].
The study has proven that IML can be an effective, simple technique that can significantly correlate to Cormack-Lehane classification. Although this study has its limitations, only 60 patients and eight were excluded due to excessive gag reflex, affecting the eventual conclusion. Still, this simple technique can be done bedside to predict the difficult airway. Not enough studies were available to establish IML as a traditional test while assessing the bedside predictors. Still, this test can be explored in large populations to determine its significance and its correlation in various high-risk populations, reducing the invasiveness of other procedures and improving the predictability of difficult airways.
BMI
Contrary to common notion, obesity is not the sole independent predictor of difficult intubation. Shimonov et al [19] revealed that reducing BMI > 30% reduced Mallampati score but did not affect laryngoscopy grade. Brodsky et al [22] stated that BMI and obesity are not independent predictors of difficult intubation. Reviewing the respective studies’ results, our results are convincing with the previous studies that the other independent predictors play a significant role than BMI itself.
Intraoperative risk analysis
Positioning of the patient
In the operating room, risk analysis starts from the proper positioning of the patient. To date, sniffing positioning has attained the best view to ease intubation [24]. Sniffing position can be achieved when the patient is in the supine position with neck flexion of at 35 degrees and atlanto-occipital extension, also termed as a head extension (-15 degrees to horizontal position). The anatomical explanation behind it is convincing, as it is stated that the neck flexion would result in the alignment of the PA and the LA. In contrast, the head extension would achieve the oral axis’s alignment with PA and LA axis, improving the glottic visualization and providing the ease of intubation [24]. Although the anatomical axis alignment is less likely to be used in a critical situation, instead of alignment of external auditory meatus to sternal notch is noted as the reference point to confirm the sniffing position. The other factors that can play a role along with the position are the size of the blade, lifting force, an anesthesiologist’s experience; individuals with varied head and neck anatomy may confound the benefits and drawbacks of specific positioning of the patient [24, 40, 41].
However, it has potential limitations where specific subgroups of patients are not benefitted from the sniffing position alone; further head extension is required to improve the glottic view [24]. To achieve the reference point in obese individuals is challenging. Studies done by Lee et al [42] and Lebowitz et al [43] stated that ramped position had shown significant improvement in attaining glottic visualization. However, its significance in these studies is not exclusively studied in obese individuals. Although it is widely accepted in obese individuals, it is still controversial in analyzing the outcomes. More studies are required to investigate the ramp methods as stacking and removing the blankets in critical time constraints is challenging [44]. A recent study performed by Hasanin et al [23] stated that compared to the ramped position, the modified ramped position by using a unique pillow has shown a significant correlation with Cormack and Lehane grade and shown the significant improvement in glottic visualization by reducing the amount of time to achieve it, and reduced the duration of intubation which can eventually improve the outcomes in the obese individuals.
Preoxygenation and optimal medication dosing
Preoxygenation
As obese patients have existing lung function changes such that they have a low functional residual capacity and are more prone to desaturation episodes, preoxygenation is a critical element to prevent the desaturation episodes in obese individuals [45]. When preoxygenation is performed in the semi-upright position, it has shown some significant benefits in obese patients [46]. The occurrence of desaturation depends on the length of the preoxygenation and the patient oxygen consumption and residual pool of oxygen in obese patients. Studies have shown that passive oxygenation with nasal cannula while performing the laryngoscopy can prevent the immediate occurrence of desaturation episodes [47].
Optimal medication dosing
The principle behind using induction drugs is to attain a rapid onset of action and minimal fat solubility. The entire pharmacodynamics and kinetics of each drug are beyond the scope of this review. As obese patients are more prone to certain drug sensitivity and can land up in respiratory depression regardless of the technique chosen, certain drugs such as anxiolytics (benzodiazepines), opioids are used in caution. As for tailoring, the dosages depend on the lean and the total body weight. For instance, most benzodiazepines are tailored according to the total body weight. In contrast, the propofol is tailored according to the lean body weight [25], and neuromuscular blocking agent (NMBA) is dosed up on using ideal body weight except for succinylcholine. Therefore, following the evidence-based dosing regimens when performing the traditional intubation is highly recommended for the best possible outcomes.
Altered airway anatomy
Despite all the predictors’ significance, they often underestimate the challenges, and there can be some unknown difficulties while attaining an airway in obese individuals. Obese patients have physiologic changes not only in their external airway anatomy but also in their oropharynx and larynx. It is worth noting that airway problems in obese patients are higher in individuals with obstructive sleep apnea (OSA) than those with high BMI. OSA individuals have shown higher rates of airway collapsibility under sleep and anesthesia [26]. Literature has shown that the distribution of body fat plays a vital role in predicting airway changes. For instance, android base fat distribution (central fat distribution) positively correlates with changes in the airway, which can lead to a difficult airway than that of a specific BMI value itself [27].
Imaging studies such as magnetic resonance imaging (MRI) and ultrasound of the neck have shown that increased parapharyngeal wall thickness with other structures, including tongue, uvula, tonsillar pillars, and tonsils, has a narrow pharyngeal inlet and can lead to limited mobility of pharyngeal structures while maneuvering for laryngoscopy [28], whereas occipital deposition has shown to have restricted ramp position of the individual. It is crucial to note that airway anatomy can play a role in positioning the patient for intubation. As the external factors can give a tinge of predictability for difficult airways, it is still worth considering the risk factor and preparing for an alternative intubation procedure.
Considering appropriate laryngoscopy device
Choosing an appropriate laryngoscopy device that can give optimal glottic visualization is essential in attaining successful intubation. Each type of device has its advantages. The principal in choosing the laryngoscopic device is to ease the intubation with fewer attempts in a short amount of time with a more precise glottic view. According to the study done by Yumul et al [20] in 120 obese adults with BMI > 30, they compared all three video laryngoscopy devices with standard Macintosh devices. The study showed that Video Mac demonstrated significant benefits compared to Glidescope and McGrath video laryngoscopes.
Video Mac showed the following significant benefits: 1) reduction in time to visualize the glottis; 2) successful placement of the endotracheal tube; 3) reduced number of intubation attempts; 4) reduced use of other ancillary devices; 5) reduced time required for confirmation of intubation by measuring end-tidal CO2.
The survey done by Cierniak et al [5] revealed that 80% of obese individuals were easy to intubate. Still, the individuals with difficult airways have had complications due to more intubation attempts than the actual difficult airway. Conversely, the study done by Yakushiji et al revealed that as BMI increases, there was a linear relationship with failed first attempt intubation, so it is worth it that proper positioning of the patient and choosing an appropriate laryngoscopy device which can reduce the number of attempts will reduce the complications [18].
Applied skills
Apart from the patient factors, there are other factors to consider, such as applied skills which infer adequate medical knowledge in handling the difficult airways and intubations. As it is an invasive procedure and tough to practice in a real clinical scenario, some studies stated that having a continuous stimulatory workshop on handling the difficult airways might enhance the trainee experience. Despite the generalized skills such as having a quick decision-making capacity, leadership, and team collaboration which are essential to achieve the best possible outcomes, further research is required to prove that having these skills can enhance patient outcomes.
| Limitations | ▴Top |
Our study is limited to elective traditional intubation scenarios and did not include any information about rapid or delayed sequence and awake intubation scenarios. It is focused on preoperative considerations and risk factors only in elective surgeries but not focused on emergency intubation scenarios, head and neck malignancies, facial abnormalities, severe psychiatric disorders, details of medication dosing, pregnant women, pediatric populations, gender-based differences, differences in trainee’s applied skills. Also, our study did not focus on differentiating the advantages and disadvantages of commercially available head elevation pillows, different types of endotracheal tubes, different types of laryngoscopy devices available instead, patient demographics and their ASA influence on the difficult airway or difficult intubation. We focused on generalized benefit of achieving the appropriate positioning and usage of Video Mac devices.
| Conclusions | ▴Top |
Most obese patients are easy to intubate. A certain subgroup of patients is more prone to the difficult airway. They tend to have quick desaturation episodes due to the restrictive pattern of the lung with low functional residual capacity. Delayed intubation in such patients may lead to hypoxemic injuries such as cerebrovascular accidents and myocardial injuries, leading to perioperative morbidity and mortality. Extensive workup and high predictability of bedside tests are required to prevent such events and handle the difficult airway. It is noticed that current bedside tests have no perfect reliability, and the study results are convincing with previous studies stating that there is no single best predictor for difficult airways. There have been conflicting results with each independent predictor, as significant inter-observer variability is noted. Our review has concluded that BMI itself is not a sole independent predictor, as literature has shown that reducing BMI has reduced Mallampati class but not in laryngoscopy grade. Even though SMD has a more predictable value, a combination of preoperative predictors while assessing the patient’s airway has shown significant improvement in predictability and validity of the bedside tests in the anticipated difficult airway. Therefore, we highly recommend the combination of tests to improve the management of the difficult airway.
Although further research is required to demonstrate the correlation between intubation attempts and patients’ outcomes, the most important causative factor for intubation-related adverse events is shown by the number of intubation attempts. Considering the intraoperative settings, every element right from the patient’s positioning to intubation has its importance. Appropriate positioning of the patient, adequate preoxygenation, and choosing the right laryngoscopy device can improve the glottic visualization within the required time and eventually reduce intubation attempts. Irrespective of patient-centered factors, trainees’ skills also play a significant role in improving patients’ outcomes. Our study recommends that frequent simulation training with team collaboration might improve the handling of difficult airway emergencies. Our study suggests further research into the newer predictors for underlying risks such as IML, neck ultrasound, the influence of pre-intubation checklists, team collaboration, and trainees’ applied skills can help draw optimal difficult airway management protocols in the high-risk populations.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Author Contributions
Each author has been individually involved in and has made substantial contributions to conceptions and designs, acquisition of data, analysis, interpretation of data, drafting, and editing the manuscript. Lakshmi Rekha Narra, Ndausung Udongwo, Jerry Dominic, Shriya Doreswamy, Anam Bhasir, Islam Elkherpitawy, and Chinwe Ogedegbe have performed literature search, drafted the manuscript and did critical editing. Lakshmi Rekha Narra has contributed to the illustrations. Lakshmi Rekha Narra, Ndausung Udongwo, and Chinwe Ogedegbe have carefully supervised this manuscript preparation and writing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33(7):673-689.
doi pubmed - Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207(6):928-934.
doi pubmed - Collins JS, Lemmens HJ, Brodsky JB. Obesity and difficult intubation: where is the evidence? Anesthesiology. 2006;104(3):617; author reply 618-619.
doi - Lundstrom LH, Moller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009;110(2):266-274.
doi pubmed - Cierniak M, Sobczak R, Timler D, Wieczorek A, Borkowski B, Gaszynski T. The degree of intubation difficulties and the frequency of complications in obese patients at the Hospital Emergency Department and the Intensive Care Unit: Case-control study. Medicine (Baltimore). 2016;95(52):e5777.
doi pubmed - Purnell JQ. Definitions, classification, and epidemiology of obesity. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al., eds. Endotext. South Dartmouth (MA), 2000.
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Hagberg CA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-270.
doi pubmed - American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98(5):1269-1277.
doi pubmed - Huang HH, Lee MS, Shih YL, Chu HC, Huang TY, Hsieh TY. Modified Mallampati classification as a clinical predictor of peroral esophagogastroduodenoscopy tolerance. BMC Gastroenterol. 2011;11:12.
doi pubmed - Kim WH, Ahn HJ, Lee CJ, Shin BS, Ko JS, Choi SJ, Ryu SA. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth. 2011;106(5):743-748.
doi pubmed - Mashour GA, Kheterpal S, Vanaharam V, Shanks A, Wang LY, Sandberg WS, Tremper KK. The extended Mallampati score and a diagnosis of diabetes mellitus are predictors of difficult laryngoscopy in the morbidly obese. Anesth Analg. 2008;107(6):1919-1923.
doi pubmed - Riad W, Vaez MN, Raveendran R, Tam AD, Quereshy FA, Chung F, Wong DT. Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: A prospective observational study. Eur J Anaesthesiol. 2016;33(4):244-249.
doi pubmed - Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth Analg. 2008;106(4):1132-1136, table of contents.
doi pubmed - Budde AO, Desciak M, Reddy V, Falcucci OA, Vaida SJ, Pott LM. The prediction of difficult intubation in obese patients using mirror indirect laryngoscopy: A prospective pilot study. J Anaesthesiol Clin Pharmacol. 2013;29(2):183-186.
doi pubmed - Yentis SM, Lee DJ. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia. 1998;53(11):1041-1044.
doi pubmed - Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, Lapandry C. The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87(6):1290-1297.
doi pubmed - Ozdilek A, Beyoglu CA, Erbabacan SE, Ekici B, Altindas F, Vehid S, Koksal GM. Correlation of neck circumference with difficult mask ventilation and difficult laryngoscopy in morbidly obese patients: an observational study. Obes Surg. 2018;28(9):2860-2867.
doi pubmed - Yakushiji H, Goto T, Shirasaka W, Hagiwara Y, Watase H, Okamoto H, Hasegawa K, et al. Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: An analysis of the multicenter prospective observational study in Japan. PLoS One. 2018;13(4):e0195938.
doi pubmed - Shimonov M, Schechter P, Boaz M, Waintrob R, Ezri T. Does body mass index reduction by bariatric surgery affect laryngoscopy difficulty during subsequent anesthesia? Obes Surg. 2017;27(3):737-739.
doi pubmed - Yumul R, Elvir-Lazo OL, White PF, Sloninsky A, Kaplan M, Kariger R, Naruse R, et al. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J Clin Anesth. 2016;31:71-77.
doi pubmed - Sheff SR, May MC, Carlisle SE, Kallies KJ, Mathiason MA, Kothari SN. Predictors of a difficult intubation in the bariatric patient: does preoperative body mass index matter? Surg Obes Relat Dis. 2013;9(3):344-349.
doi pubmed - Brodsky JB, Lemmens HJ, Brock-Utne JG, Vierra M, Saidman LJ. Morbid obesity and tracheal intubation. Anesth Analg. 2002;94(3):732-736; table of contents.
doi pubmed - Hasanin A, Tarek H, Mostafa MMA, Arafa A, Safina AG, Elsherbiny MH, Hosny O, et al. Modified-ramped position: a new position for intubation of obese females: a randomized controlled pilot study. BMC Anesthesiol. 2020;20(1):151.
doi pubmed - El-Orbany M, Woehlck H, Salem MR. Head and neck position for direct laryngoscopy. Anesth Analg. 2011;113(1):103-109.
doi pubmed - Members of the Working Party, Nightingale CE, Margarson MP, Shearer E, Redman JW, Lucas DN, Cousins JM, et al. Peri-operative management of the obese surgical patient 2015: Association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Anaesthesia. 2015;70(7):859-876.
doi pubmed - Wadhwa A, Singh PM, Sinha AC. Airway management in patients with morbid obesity. Int Anesthesiol Clin. 2013;51(3):26-40.
doi pubmed - Horner RL, Mohiaddin RH, Lowell DG, Shea SA, Burman ED, Longmore DB, Guz A. Sites and sizes of fat deposits around the pharynx in obese patients with obstructive sleep apnoea and weight matched controls. Eur Respir J. 1989;2(7):613-622.
- Ezri T, Gewurtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, Susmallian S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58(11):1111-1114.
doi pubmed - Ilper H, Franz-Jager C, Byhahn C, Klages M, Ackermann HH, Zacharowski K, Kunz T. [Update Mallampati : Theoretical and practical knowledge of European anesthetists on basic evaluation of airways]. Anaesthesist. 2018;67(10):738-744.
doi pubmed - Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, Desmonts JM. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003;97(2):595-600.
doi pubmed - Walls RM, Frcpc, Faaem. Extended vs. standard Mallampati scoring for morbidly obese patients. Anesth Analg. 2008. https://www.jwatch.org/em200812240000003/2008/12/24/extended-vs-standard-mallampati-scoring-morbidly.
- Menon SM, Sampangiramaiah S, Mathew M. Cross sectional observational study performed to see for relation of Mallampati score and extended Mallampati score with body mass index. J Clin Diagn Res. 2017;11(5):UG01-UG03.
doi pubmed - Hanouz JL, Bonnet V, Buleon C, Simonet T, Radenac D, Zamparini G, Fischer MO, et al. Comparison of the Mallampati classification in sitting and supine position to predict difficult tracheal intubation: a prospective observational cohort study. Anesth Analg. 2018;126(1):161-169.
doi pubmed - Ouchi K, Hosokawa R, Yamanaka H, Nakajima Y, Nakamura Y, Kishimoto J. Mallampati test with phonation, tongue protrusion and supine position is most correlated with Cormack-Lehane test. Odontology. 2020;108(4):617-625.
doi pubmed - Schiff JH, Walther A, Krier C, Hagberg CA. Chapter 51 - complications of managing the airway. In: Hagberg CA (ed), Benumof and Hagberg's Airway Management, third edition. W.B. Saunders. 2013; p. 1047-1069.e6. https://www.sciencedirect.com/science/article/pii/B9781437727647000518.
doi - Prakash S, Mullick P, Bhandari S, Kumar A, Gogia AR, Singh R. Sternomental distance and sternomental displacement as predictors of difficult laryngoscopy and intubation in adult patients. Saudi J Anaesth. 2017;11(3):273-278.
doi pubmed - Patel B, Khandekar R, Diwan R, Shah A. Validation of modified Mallampati test with addition of thyromental distance and sternomental distance to predict difficult endotracheal intubation in adults. Indian J Anaesth. 2014;58(2):171-175.
doi pubmed - Ghatge S, Hagberg CA. Chapter 17 - does the airway examination predict difficult intubation? In: Fleisher LA (ed). Evidence-based practice of anesthesiology, second edition. W.B. Saunders. 2009; p. 101-115. https://www.sciencedirect.com/science/article/pii/B9781416059967000171.
doi - Siriussawakul A, Rattana-arpa S, Jirachaipitak S, Chatsiriphattana A, Nimmannit A, Wong-in N. The performance of the neck circumference for a difficult laryngoscopy in obese patients. J Med Assoc Thai. 2016;99(5):484-490.
- Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S, Imrie D, et al. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003;98(1):23-27.
doi pubmed - Liess BD, Scheidt TD, Templer JW. The difficult airway. Otolaryngol Clin North Am. 2008;41(3):567-580.
doi pubmed - Lee JH, Jung HC, Shim JH, Lee C. Comparison of the rate of successful endotracheal intubation between the "sniffing" and "ramped" positions in patients with an expected difficult intubation: a prospective randomized study. Korean J Anesthesiol. 2015;68(2):116-121.
doi pubmed - Lebowitz PW, Shay H, Straker T, Rubin D, Bodner S. Shoulder and head elevation improves laryngoscopic view for tracheal intubation in nonobese as well as obese individuals. J Clin Anesth. 2012;24(2):104-108.
doi pubmed - Greenland KB. More on ramped position and 25-degree head up positions. Br J Anaesth. 2016;117(5):674-675.
doi pubmed - Law JA, Broemling N, Cooper RM, Drolet P, Duggan LV, Griesdale DE, Hung OR, et al. The difficult airway with recommendations for management—part 2—the anticipated difficult airway. Can J Anaesth. 2013;60(11):1119-1138.
doi pubmed - Dixon BJ, Dixon JB, Carden JR, Burn AJ, Schachter LM, Playfair JM, Laurie CP, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;102(6):1110-1115; discussion 1115A.
doi pubmed - Gleason JM, Christian BR, Barton ED. Nasal cannula apneic oxygenation prevents desaturation during endotracheal intubation: an integrative literature review. West J Emerg Med. 2018;19(2):403-411.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


