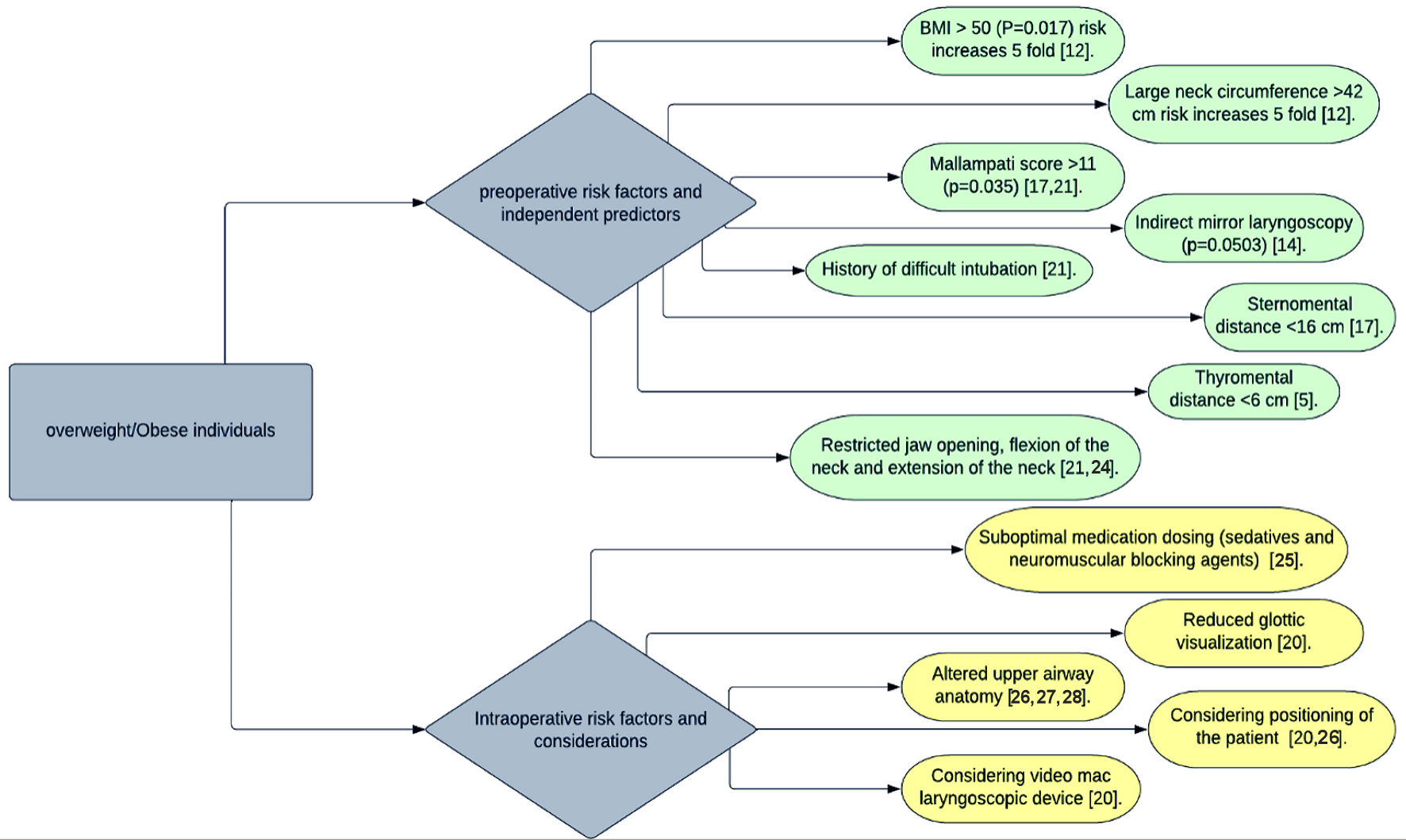
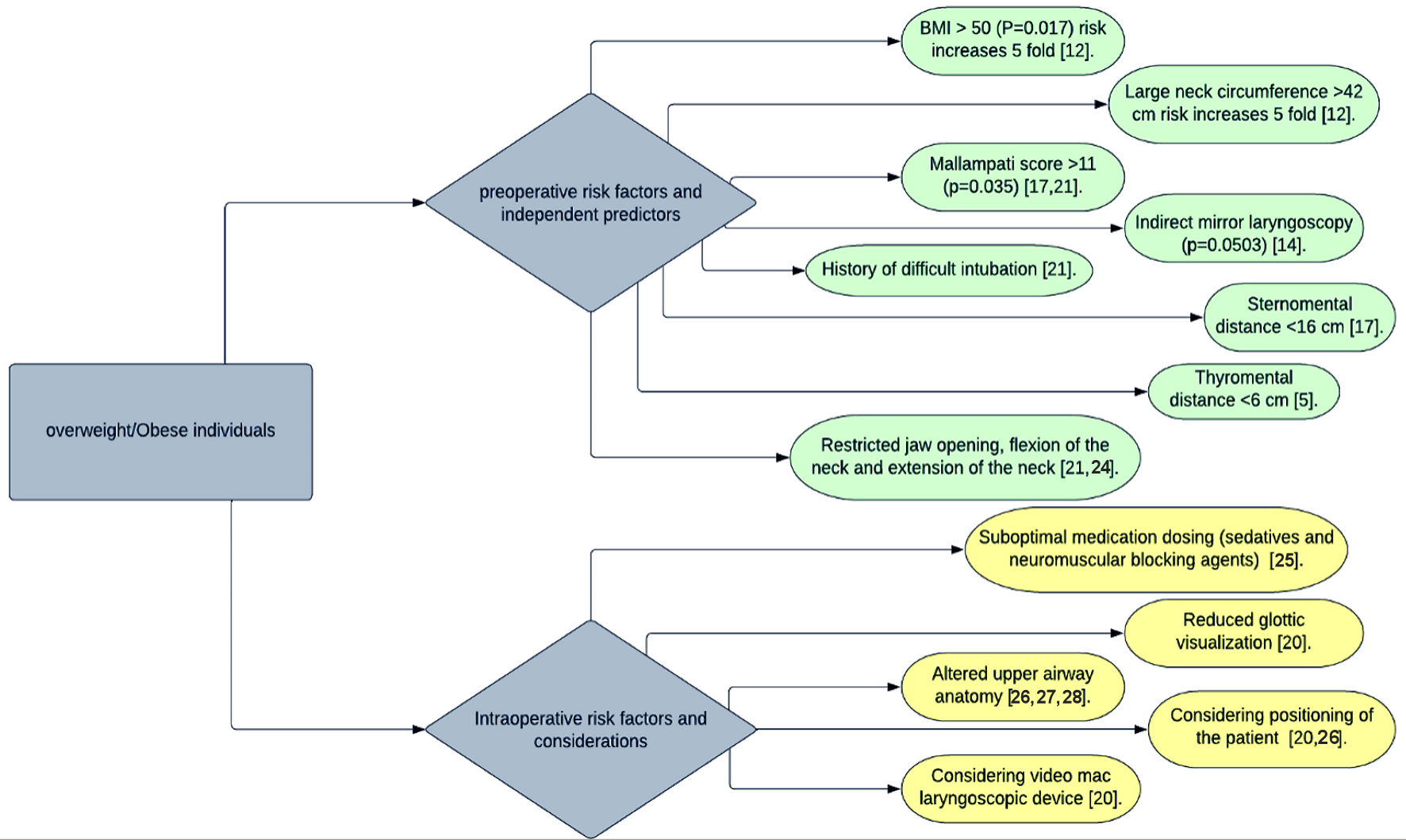
Figure 1. Diagram illustrating preoperative and intraoperative risk factors of intubation in overweight/obese individuals.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 14, Number 5, May 2022, pages 177-187
Obesity and the Other Independent Predictors in Elective Endotracheal Tube Intubations: A Narrative Review
Figure
Tables
| Obesity class | BMI reference range (kg/m2) |
|---|---|
| BMI: body mass index. | |
| Normal BMI | 18.5 - 24.9 |
| Overweight | 25.0 - 29.9 |
| Obese class 1/class 2 | 30.0 - 34.9/35.0 - 39.9 |
| Extreme or morbid obesity (class 3) | ≥ 40 |
| Author | Study type | Intervention | Number of subjects | Results | Conclusion |
|---|---|---|---|---|---|
| SMD: sternomental distance; DL: direct laryngoscope; TMD: thyromental distance; VL: video laryngoscopy; IDS: Intubation Difficulty Scale; CI: confidence interval. | |||||
| Ozdilek et al, 2018 [17] | Prospective observational study | Using the Comrack-Lehane classification, a direct laryngoscopy grade was given on morbidly obese subjects who underwent elective surgery. | 120 subjects including 37 males and 83 females | Incidence of difficult laryngoscopy: 10.8% males and 4.8% of females | Mallamapti score > II, SMD < 16, inadequate flexion of the neck were significant predictors for difficult laryngoscopy in males; whereas in females only Mallampati > II was a significant predictor. |
| Yakushiji et al, 2018 [18] | Multicenter prospective observational study | Direct laryngoscopies and endotracheal tube intubations | 6,889 subjects 5,370 lean (77%) 1,177 overweight (17%) 342 obese (4%) | As the BMI increases, the rate of success was reduced. 70.9% in lean patients (95% CI: 69.7% - 72.1%) 66.4% in overweight patients (95% CI: 63.7% - 69.1%) 59.3% in obese patients (95% CI: 53.9% - 64.6%) | In both adjusted and unadjusted models, obesity and overweight were related to lower success rates of first intubation attempts and was associated with a high risk of adverse events (P < 0.0001). |
| Shimonov et al [19] | Retrospective study | Direct laryngoscopy and endotracheal intubations for elective surgeries in patients who have reduced 30% of their BMI through bariatric surgeries, specifically laparoscopic sleeve gastrectomy, and laparoscopic band insertion. In this study, difficult airway was graded as Mallampati class III and IV, laryngoscopy grade > 2, and the need for unplanned fiberoptic intubation. | Out of 629 patients who underwent bariatric surgeries, 62 patients were eligible. | The study showed a significant decrease in Mallampati class (P = 0.000), and no change in laryngoscopy grade (P = 0.419). | After a 30% reduction of BMI value between the two surgical procedures, it was observed that there was a significant decrease in Mallampati class but no change in laryngoscopy grade and no record of unplanned fiberoptic intubation. |
| Yumul et al [20] | Randomized controlled trials | Comparing three different VL devices (Video Mac VL, Glidescope VL, McGrath VL) to standard direct laryngoscope (DL) in subjects who are undergoing elective bariatric surgery. | 121 individuals with BMI > 30 | The success rate for first attempt intubation greatly differed between standard DL and all three VLs. Standard DL showed 74% success rate Video Mac, Glidescope showed 93% success rate and McGrath group showed 70% success. In comparing three video devices, Video Mac and McGrath were equal in efficacy in obtaining glottic view, whereas the efficacy of Video Mac and Glidescope was equal in the number of intubation attempts (P ≤ 0.05) and use of ancillary intubation devices. | Compared to standard DL, the use of all three VL reduced the time needed to attain successful endotracheal intubation and augmented the visualization of the glottis in the obese surgical population. |
| Cierniak et al, 2016 [5] | Prospective observational study | Direct laryngoscopy and endotracheal intubation | Out of 153 subjects, 48 individuals with BMI > 35 were eligible for this study. | TMD < 6 cm, SMD < 12.5 cm were observed as independent predictors for difficult airway in obese individuals. FRONT score showed poor relation to a difficult airway. Video laryngoscopy was used to efficiently analyze the difficult airway by using a particular scale. | Besides SMD and TMD being strong predictors, the incidence of post-intubation hematomas was high in obese individuals, due to increased number of intubation attempts (58% of obese individuals have two intubation attempts compared to only 35% of obese patients intubated successfully in the first attempt). |
| Riad et al, 2016 [12] | Prospective observational study | Direct laryngoscopy and endotracheal intubation. Difficult intubation was considered an IDS of at least five characteristics. Any value below five was considered easy. | Out of 104 individuals with BMI > 40, 88 were women, and 16 were men. | This study yielded that neck circumference greater than 42 cm (P = 0.044) and BMI greater than 50 kg/m2 (P = 0.017) are proven to be independent predictors of difficult intubation. | Besides neck circumference > 42 cm and BMI > 50 kg/m2 as independent predictors, they increased the 5-fold risk for difficult intubation. It is shown that 13% of morbidly obese patients have difficult tracheal intubation. |
| Sheff et al, 2012 [21] | Retrospective observational study | Direct laryngoscopies and endotracheal intubation in morbidly obese patients, scheduled for laparoscopic Roux-en-Y gastric bypass surgery. | 912 individuals | 830 (91%) had an uneventful intubation; 57 (6.3%) had a difficult intubation; 25 (2.7%) underwent planned fiberoptic intubation. Study has shown that following are independent predictors: 1) Mallampati class IV (P = 0.035); 2) abnormal TMD (P = 0.001); 3) restricted mobility of the jaw (P = 0.018); 4) history of difficult intubation (P = 0.002). | Difficult intubations were not associated with an increase in BMI (P = .073). Mallampati class IV, restricted jaw mobility, abnormal TMD, a history of difficult intubation were significant predictors for difficult intubations. |
| Gonzalez et al, 2008 [13] | A prospective randomized study | Direct laryngoscopies and endotracheal tube intubation. Comparison of incidence of difficult intubation between obese and lean populations. Difficult intubation is termed as IDS > 5, anything < 5 classified as easy to intubate. | Out of 131 individuals, 70 were obese with BMI > 30 and 61 lean patients BMI < 30 | The study showed that difficult tracheal intubation is more common in obese (14.3%) than in lean patients (3%); P value = 0.03. | IDS > 5, with large neck circumference, higher BMI, abnormal TMD, and higher Mallampati score were shown to be independent risk factors. |
| Brodsky et al, 2002 [22] | Prospective observational study | Outcomes of tracheal intubation in morbidly obese patients (BMI > 40 kg/m2) Direct laryngoscopy grade and intubation attempts were recorded | 100 morbidly obese individuals | 12 patients with higher Mallampati score and larger neck circumference had problematic intubation. | BMI and obesity were not independent predictors for difficult intubations. Higher Mallampati score and larger neck circumference increases the difficulty of intubation. |
| Hasanin et al, 2020 [23] | A randomized controlled pilot study | Outcomes of the modified ramped position of the patient while performing direct laryngoscopy and endotracheal tube intubation. | 60 obese female individuals | 14 (47%) individuals in the ramped group required repositioning to insert laryngoscope. One individual (3%) required repositioning in the modified ramped group. | Modified ramped position yielded better results in reducing time for glottic visualization and endotracheal tube insertion as well as better Comrack-Lehane grade. |