| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 9, Number 4, April 2017, pages 366-373
Current Metabolic Status Affects Urinary Liver-Type Fatty-Acid Binding Protein in Normoalbuminuric Patients With Type 2 Diabetes
Hiroyuki Itoa, c, Hitomi Yamashitab, Mina Nakashimab, Akifusa Takakib, Chiduko Yukawab, Suzuko Matsumotoa, Takashi Omotoa, Masahiro Shinozakia, Shinya Nishioa, Mariko Abea, Shinichi Antokua, Mizuo Mifunea, Michiko Toganea
aDepartment of Diabetes, Metabolism and Kidney Disease, Edogawa Hospital, Tokyo, Japan
bLaboratory Department, Edogawa Hospital, Tokyo, Japan
cCorresponding Author: Hiroyuki Ito, Department of Diabetes, Metabolism and Kidney Disease, Edogawa Hospital, 2-24-18, Higashi-koiwa, Edogawa-ku, Tokyo 133-0052, Japan
Manuscript accepted for publication February 07, 2017
Short title: Urinary L-FABP in Type 2 Diabetes
doi: https://doi.org/10.14740/jocmr2934w
| Abstract | ▴Top |
Background: We aimed to study the association between urinary liver-type fatty acid-binding protein (L-FABP), a biomarker of tubulointerstitial injury, and the clinical characteristics of normoalbuminuric and albuminuric patients with type 2 diabetes in order to detect the factors affecting urinary L-FABP.
Methods: Urinary L-FABP levels were measured in 788 patients with type 2 diabetes and again in 666 patients at 6 months after the initial measurement. The association between the urinary L-FABP level and the clinical parameters was investigated in a retrospective cross-sectional study and a subsequent observation.
Results: The HbA1c (odds ratio (OR): 1.42; 95% confidence interval (CI): 1.11 - 1.79; P < 0.01), systolic blood pressure (OR: 1.03; 95% CI: 1.01 - 1.05; P < 0.01) levels and estimated glomerular filtration rate (OR: 0.98; 95% CI: 0.96 - 1.00; P = 0.01) were significantly associated with the high levels of urinary L-FABP (> 8.4 μg/gCr) in normoalbuminuric patients. However, a logistic regression analysis revealed that use of renin-angiotensin system (RAS) inhibitors (OR: 2.22; 95% CI: 1.16 - 4.89; P = 0.02), urinary albumin-to-creatinine ratio (ACR) (OR: 1.01; 95% CI: 1.00 - 1.01; P < 0.01) and serum HDL-cholesterol concentration (OR: 0.33; 95% CI: 0.11 - 0.89; P = 0.03) were significantly associated in albuminuric patients. In the follow-up observation, the change in urinary L-FABP was found to be significantly (P < 0.01) influenced by the change in the HbA1c level in both the normoalbuminuric and albuminuric patients.
Conclusions: High urinary L-FABP is associated with part of the current metabolic abnormalities, including high levels of HbA1c and systolic blood pressure among normoalbuminuric patients with type 2 diabetes.
Keywords: Urinary liver-type fatty-acid binding protein; Diabetic nephropathy; Biomarker; Tubulointerstitial injury
| Introduction | ▴Top |
Liver-type fatty acid-binding protein (L-FABP) is a 14-kDa protein which is expressed in the hepatocytes and the proximal tubular cells of the kidneys, and participates in fatty acid metabolism in the cytoplasm [1-3]. Urinary L-FABP has been reported to be secreted from proximal tubules during oxidative stress or in the event of ischemia. Urinary L-FABP is thus considered to be a biomarker for predicting the prognosis of kidney function in renal diseases such as acute kidney injury [4-6] and non-diabetic chronic kidney diseases [7].
Tubulointerstitial damage has been described as an important step in the progression of diabetic nephropathy [8-10]. Several studies have demonstrated that urinary L-FABP is already elevated at the early stage of diabetic nephropathy in patients with type 2 diabetes [11-13]. This is similar to the elevation that is observed in other biomarkers for tubulointerstitial injury, including kidney injury molecule (KIM)-1, neutrophil gelatinase-associated lipocalin (NGAL) and interleukin-18 [13]. Kamijo-Ikemori et al demonstrated that a high level of urinary L-FABP predicted the progression of diabetic nephropathy in 104 patients with type 2 diabetes based on a 4-year observation period [12]. In a 12-year follow-up study of 618 type 2 diabetic patients without overt nephropathy, Araki et al reported that renal dysfunction progressed among subjects with elevated levels of urinary L-FABP [14]. Because similar results were also observed in patients with type 1 diabetes [15, 16], urinary L-FABP is currently recognized as an early predictor for renal dysfunction associated with diabetic nephropathy. However, it remains unclear why the urinary L-FABP level is elevated at the early stage of diabetic nephropathy in comparison to normal individuals.
We aimed to investigate the association between urinary L-FABP and clinical characteristics of normoalbuminuric and albuminuric patients with type 2 diabetes in order to identify the factors that affect urinary L-FABP using a cross-sectional study and subsequent follow-up observation.
| Materials and Methods | ▴Top |
Subjects
The urinary L-FABP levels were measured in random spot urine samples as part of the standard routine care patients with diabetes in the Department of Diabetes, Metabolism and Kidney Disease of Edogawa Hospital, Tokyo, Japan. All of the clinical data, including the urinary L-FABP levels that were used in the present retrospective cross-sectional study and in the subsequent follow-up period were extracted from the patients’ medical records. After excluding 19 subjects with type 1 diabetes, five subjects with chronic glomerulonephritis and two subjects with tubulointerstitial nephritis, 788 Japanese patients with type 2 diabetes, who underwent consecutive treatments in our department between August and November 2014, were included in the cross-sectional study. Urinary L-FABP was determined again in 666 patients who continued to visit our department for 6 months after the initial measurement.
Measurement of urinary L-FABP
An enzyme-linked immunosorbent assay was performed to measure the urinary L-FABP concentration using a commercial kit (CIMIC Holdings Co., Ltd, Tokyo, Japan), which is widely used in Japan [7, 11, 12, 17, 18], at an external laboratory (SRL Co., Tokyo, Japan). The patients were categorized based on their levels of urinary L-FABP. The high urinary L-FABP group included patients in whom the L-FABP level was corrected by a urinary creatinine level of > 8.4 μg/gCr, while the low urinary L-FABP group included patients in whom the L-FABP level was corrected by a urinary creatinine level of ≤ 8.4 μg/gCr, based on a previous study [18] and the manufacturer’s data [19]. Values under the detection limit of < 3.0 ng/mL were described as 0 μg/gCr in the present study.
Confounding factors
Hypertension was defined as a systolic blood pressure ≥ 140 mm Hg and/or a diastolic blood pressure ≥ 90 mm Hg. The participants currently using antihypertensive medications were also classified as positive for hypertension. Hyper LDL-cholesterolemia was defined as either a serum concentration of LDL-cholesterol ≥ 3.62 mmol/L, or the current use of lipid-lowering agents. The estimated glomerular filtration rate (eGFR) was calculated using the formula which is recommended by the Japanese Society of Nephrology [20]. Albuminuria was defined as a urinary albumin-to-creatinine ratio (ACR) ≥ 30 mg/gCr in random spot urine. Hyperuricemia was defined by a serum uric acid level > 416 μmol/L or as patients using urate-lowering agents.
The ankle-brachial pressure index (ABI), brachial-ankle pulse wave velocity (baPWV) and intima-media thickness of carotid artery (cIMT) measured via ultrasonographic examinations, as indicators of atherosclerotic diseases, were measured as described previously [21, 22].
Diabetic retinopathy, peripheral neuropathy, cerebrovascular disease, coronary heart disease and peripheral artery were also diagnosed as described previously [21-25].
Ethics
This study was conducted according to the principles expressed in the Declaration of Helsinki. The Ethics Committees of Edogawa Hospital approved the protocol for this study and waived the need for written informed consent, because the data were analyzed anonymously for this retrospective study based on the data stored in the hospital database (approval number: 2015-20).
Statistical analysis
All data were shown as mean ± SD. The Wilcoxon rank sum test, Wilcoxon signed-rank test, Kruskal-Wallis test and χ2 test were used for among-group comparisons of the continuous and categorical variables. The odds ratio (OR) and respective 95% confidence intervals (95% CIs) were determined to examine the strength of the relationship between clinical characteristics of the patients and the prevalence of high urinary L-FABP by a logistic regression analysis. Independent variables in the logistic regression analysis were determined according to a forward stepwise selection. Differences with a value of P < 0.05 (two-tailed) were considered to be statistically significant. The JMP statistical software package, version 8.0 (SAS Institute, Cary, NC, USA), was used to perform all of the analyses.
| Results | ▴Top |
Table 1 shows the clinical characteristics of the study subjects. Albuminuria and high urinary L-FABP were observed in 322 (41%) and 143 (18%) of the subjects, respectively. Both the urinary L-FABP concentration (2.3 ± 5.2 μg/gCr, 5.7 ± 11.9 μg/gCr and 27.6 ± 34.9 μg/gCr in subjects with an ACR < 30 mg/gCr (n = 466), 30 mg/gCr ≤ ACR < 300 mg/gCr (n = 218) and 300 mg/gCr ≤ ACR (n = 104), respectively) and the frequency of high urinary L-FABP (8%, 19% and 63% in subjects with an ACR < 30 mg/gCr, 30 mg/gCr ≤ ACR < 300 mg/gCr and 300 mg/gCr ≤ ACR, respectively) became significantly higher (P < 0.0001) with the progression of ACR.
 Click to view | Table 1. The Clinical Characteristics of the Patients |
Table 2 shows the comparisons of clinical characteristics between the high and normal urinary L-FABP groups among normoalbuminuric (ACR < 30 mg/gCr) and albuminuric (ACR ≥ 30 mg/gCr) patients with type 2 diabetes. In the normoalbuminuric patients, the HbA1c level was significantly higher in the high urinary L-FABP group than in the normal urinary L-FABP group. Biguanides use, systolic blood pressure, the HbA1c level and the eGFR were selected as significant variables among the significant independent variables or the variables that tended to differ between the high L-FABP and normal L-FABP groups (Table 2) after a forward stepwise selection. A logistic regression analysis revealed that systolic blood pressure, HbA1c level and eGFR were significantly associated with high urinary L-FABP in the normoalbuminuric patients (Table 3). In the albuminuric patients, use of renin-angiotensin system (RAS) inhibitors, urinary ACR and serum HDL-cholesterol concentration were found to be significantly associated with high urinary L-FABP.
 Click to view | Table 2. Comparisons of the Clinical Characteristics in the High and Normal Urinary L-FABP Groups Among Normoalbuminuric and Albuminuric Patients With Type 2 Diabetes |
 Click to view | Table 3. ORs of Clinical Characteristics for High Urinary L-FABP in Normoalbuminuric and Albuminuric Patients With Type 2 Diabetes |
Among the normoalbuminuric patients, the surrogate markers for atherosclerotic diseases and the prevalence of diabetic vascular complications did not differ between the patients of the high and normal urinary L-FABP groups. Among the albuminuric patients, however, diabetic retinopathy, peripheral neuropathy, cerebrovascular disease and peripheral artery disease were found to be significantly more frequent in the high urinary L-FABP group than in the normal urinary L-FABP group (Table 2). Furthermore, among the albuminuric patients, the ABI and baPWV values tended to be lower and higher, respectively, in the high urinary L-FABP group than in the normal urinary L-FABP group.
After 6 months of observation, the urinary L-FABP concentration was significantly elevated in the normoalbuminuric group and the eGFR was significantly reduced in the albuminuric group (Table 4). The urinary L-FABP concentration showed a tendency to increase in the albuminuric group. The change in urinary L-FABP (ΔL-FABP) demonstrated a significantly positive association (P < 0.01) with the change in the HbA1c values of both normoaluminuric and albuminuric patients (Fig. 1). The ΔL-FABP was not significantly associated with the changes in systolic blood pressure (n = 400, r2 = 0.005, P = 0.18) and eGFR (n = 403, r2 = 0.004, P = 0.23) among the normoalbuminuric patients. Additionally, the ΔL-FABP was not significantly associated with the change in serum HDL-cholesterol concentration (n = 87, r2 = 0.02, P = 0.15) among albuminuric patients. During the observation period, the frequency of subjects who newly developed diabetic macroangiopathies was not significantly different between the subjects with high (two of 80; 2.5%) and normal (two of 182; 1%) urinary L-FABP among the albuminuric patients (P = 0.39).
 Click to view | Table 4. Comparison of the Clinical Characteristics of Subjects Who Were Observed for 6 Months |
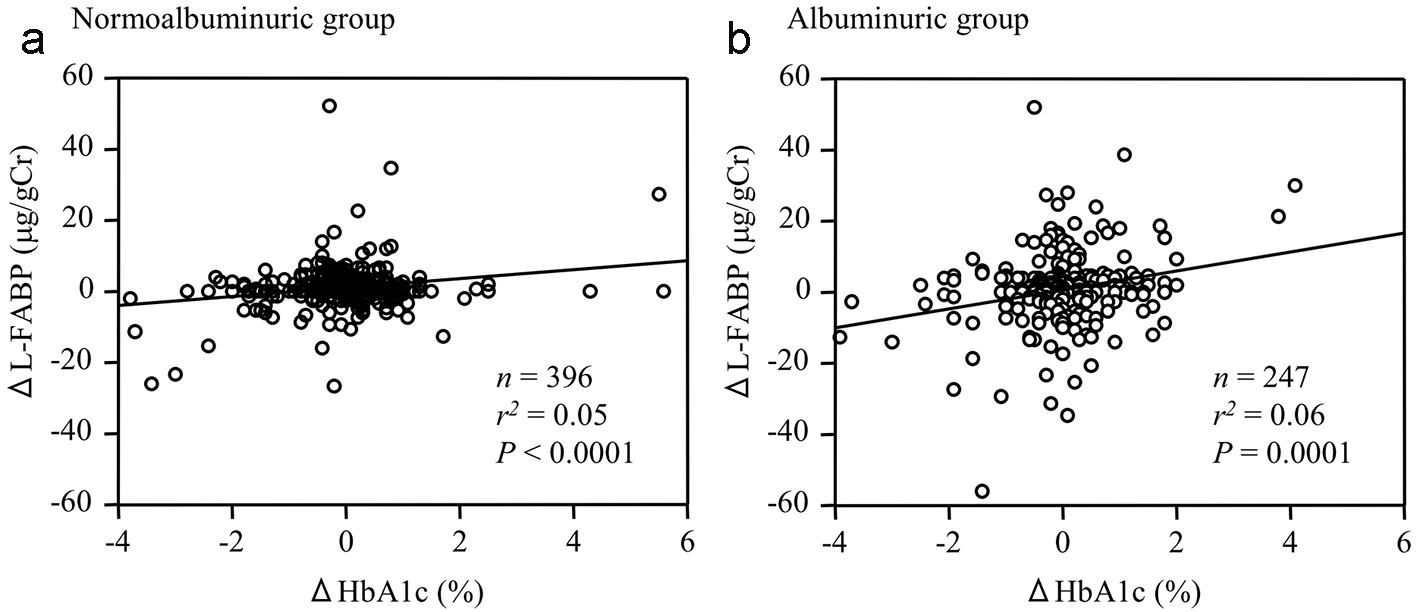 Click for large image | Figure 1. The relationship between the changes in urinary L-FABP (ΔL-FABP) and HbA1c level (ΔHbA1c) during the 6-month observation period among (a) normoalbuminuric and (b) albuminuric patients with type 2 diabetes. |
| Discussion | ▴Top |
In the present study, the levels of HbA1c and systolic blood pressure were significantly associated with urinary L-FABP in the normoalbuminuric patients with type 2 diabetes. Furthermore, the changes in the HbA1c level were significantly related to the changes in urinary L-FABP during the observation period. These results demonstrate that the effect of short-term glycemic control on the level of urinary L-FABP occurs independently of the therapies that are applied to treat hyperglycemia, especially in normoalbuminuric patients with type 2 diabetes. To the best of the authors’ knowledge, the current study is the first report to focus on the relationship between the metabolic status and urinary L-FABP in diabetic patients without albuminuria. This association is considered to be one of the reasons why the urinary L-FABP level at the early stage of diabetic nephropathy is higher than in normal subjects [11-15]. Furthermore, these results may indicate a mechanism that good glycemic control protects kidney function in patients with type 2 diabetes [26, 27].
It has been established that albuminuria secondary to glomerular injury is a biomarker for early diabetic nephropathy. Albuminuria is generally caused after long-term exposure to risk factors for diabetic nephropathy, such as hyperglycemia and hypertension [28, 29]. Meanwhile, tubulointerstitial injury may occur due to short-term metabolic abnormalities, because a significant association was found between part of the current metabolic status and the urinary L-FABP level among the normoalbuminuric patients of the present study. In addition to the direct injury to the glomeruli caused by hyperglycemia, the accumulation of preceding tubulointerstitial damage induced by short-term metabolic abnormalities, may lead to glomerular damage. Kamijo-Ikemori et al showed that hyperglycemia increased the expression of L-FABP in the proximal tubules and its urinary excretion in human L-FABP transgenic mice [18]. Recently, Hasegawa et al reported that sirtuin 1 (Sirt 1), which plays an important role in organ protection against age-related diseases, was downregulated in the proximal tubules prior to albuminuria in streptozotocin-induced and obese diabetic mice [30]. The authors also demonstrated that Sirt1 deficiency caused the dysfunction of the podocytes in the glomeruli via the overexpression of claudin-1, which is a major constituent of the tight junction complexes, and finally plays a role in the initial change of albuminuria. This mechanism differs from the classical concept of diabetic nephropathy in that glomerular injury which occurs secondary to hyperglycemia and hypertension plays a central role in the progression of renal injury. However, high urinary L-FABP, which was associated with HbA1c and blood pressure levels in the normoalbuminuric patients of the current study, may indicate the presence of tubulointerstitial damage prior to the glomerular injury in patients with type 2 diabetes. Urinary L-FABP shows a strong correlation with the peritubular blood flow and is a sensitive biomarker for microcirculation failure in the renal proximal tubules [31]. Thus in the present study, cytotoxic factors, such as energy deficiency in the proximal tubular cells and peritubular ischemia caused by hyperglycemia or hypertension might have been clinically expressed as high levels of urinary L-FABP. Because our results obtained from the follow-up period suggested that urinary L-FABP elevation is treatable by the correction of hyperglycemia, urinary L-FABP may be a biomarker for the renoprotective effects of the therapeutic intervention to treat some of the metabolic abnormalities that occur concomitantly with diabetes.
Few clinical studies have investigated the relationship between the blood glucose level and urinary L-FABP. Ishimitsu et al reported that there was a significant positive correlation between urinary L-FABP and the level of fasting blood glucose in health-check participants without overt diabetes or glomerulonephritis [32]. However, other cross-sectional studies have indicated that urinary L-FABP is not associated with the HbA1c level in patients with type 2 diabetes [17, 33]. This lack of association is considered to be caused by the different study subjects as their study populations included diabetic patients with various stages of diabetic nephropathy. Because urinary L-FABP is strongly associated with the degree of ACR [11-17], similarly to our present results, the relationship between urinary L-FABP and the patients’ current metabolic status may have been underestimated in these previous studies. Nakamura et al reported that the level of urinary L-FABP was significantly reduced by the administration of pioglitazone (n = 17), but not by glibenclamide (n = 18), voglibose (n = 17) or nateglinide (n = 18) in patients with type 2 diabetes and microalbuminuria [34]. The authors also reported that the administration of telmisartan, an angiotensin II receptor antagonist (ARB), led to a reduction of the urinary L-FABP level in the patients with diabetic nephropathy [35, 36]. It was also demonstrated that the administration of olmesartan [37], another ARB, lisinopri [38], an angiotensin-converting enzyme inhibitor, and azelnidipine [39], a calcium channel blocker, reduced the level of urinary L-FABP in patients with type 2 diabetes. Thus, although the changes in systolic blood pressure were not found to be associated with the changes in urinary L-FABP in the present study, the reduction in urinary L-FABP may be caused by the control of hypertension. The use of RAS inhibitors was associated with a high urinary L-FABP level among albuminuric patients in the present study. This is considered to be caused by causal effects of the present cross-sectional study because RAS inhibitors are commonly prescribed for diabetic patients with albuminuria and/or renal impairment to prevent the progression of nephropathy and the development of macroangiopathies.
In the present study, both the level of urinary L-FABP and the frequency of high urinary L-FABP increased with the progression of albuminuria. These results were similar to those of previous studies [11-17]. Also in line with previous studies was the finding that diabetic micro- and macroangiopathies were more frequently found in albuminuric patients with high urinary L-FABP than in those with normal urinary L-FABP [14, 20]. The surrogate markers for atherosclerotic diseases showed abnormalities in the patients with high of urinary L-FABP and albuminuria. Therefore, among albuminuric patients with type 2 diabetes, high urinary L-FABP is considered to be associated with increased levels of vascular damage. Intensive examinations for atherosclerosis should be considered in albuminuric patients with type 2 diabetes, especially individuals with high urinary L-FABP. During the observation period, the frequency of subjects who developed diabetic macroangiopathies was not significantly different between the subjects with high and normal urinary L-FABP levels among the albuminuric patients in the present study. This is considered to be due to the short observation period and small number of subjects who developed cardiovascular events.
The present study is associated with limitations that should be kept in mind when considering the results. First, our data do not address the causal effects of the findings, because a cross-sectional analysis was performed. We only showed that there was an association between high urinary L-FABP and part of the metabolic status in the patients with type 2 diabetes. However, the coefficients of determination between the ΔL-FABP and ΔHbA1c values were low (Fig. 1). Furthermore, we did not investigate the impact of antidiabetic or antihypertensive medications during the observation period. There may be other factors that affect the urinary L-FABP concentration, such as the drugs that are used during the observation period. A prospective study is therefore necessary to confirm our results. Second, ACR and L-FABP were measured from single random spot urine samples, thus, there might have been some variation in the measured values. Such variability should be considered to confirm the diabetic nephropathy group staged by ACR because it is recommended that an evaluation should be performed in two or more samples. Despite these limitations, it is considered to be noteworthy that the present results obtained from the relatively larger number of the subjects broaden our interpretation of the significance of urinary L-FABP in patients with type 2 diabetes.
In conclusion, our results suggest that high urinary L-FABP is associated with high levels of HbA1c and systolic blood pressure in normoalbuminuric patients and more frequent diabetic vascular complications in albuminuric subjects.
Acknowledgments
The authors thank Tomoko Koyanagi in the secretarial section of Edogawa Hospital for her valuable help with data collection.
Funding
The authors did not receive funding for this work.
Competing Interests
All authors declare that there are no competing interests.
Grant Support
None.
| References | ▴Top |
- Sweetser DA, Heuckeroth RO, Gordon JI. The metabolic significance of mammalian fatty-acid-binding proteins: abundant proteins in search of a function. Annu Rev Nutr. 1987;7:337-359.
doi pubmed - Veerkamp JH, Peeters RA, Maatman RG. Structural and functional features of different types of cytoplasmic fatty acid-binding proteins. Biochim Biophys Acta. 1991;1081(1):1-24.
doi - Kamijo-Ikemori A, Sugaya T, Ichikawa D, Hoshino S, Matsui K, Yokoyama T, Yasuda T, et al. Urinary liver type fatty acid binding protein in diabetic nephropathy. Clin Chim Acta. 2013;424:104-108.
doi pubmed - Portilla D, Dent C, Sugaya T, Nagothu KK, Kundi I, Moore P, Noiri E, et al. Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2008;73(4):465-472.
doi pubmed - Matsui K, Kamijo-Ikemori A, Sugaya T, Yasuda T, Kimura K. Usefulness of urinary biomarkers in early detection of acute kidney injury after cardiac surgery in adults. Circ J. 2012;76(1):213-220.
doi pubmed - Cho E, Yang HN, Jo SK, Cho WY, Kim HK. The role of urinary liver-type fatty acid-binding protein in critically ill patients. J Korean Med Sci. 2013;28(1):100-105.
doi pubmed - Kamijo A, Sugaya T, Hikawa A, Yamanouchi M, Hirata Y, Ishimitsu T, Numabe A, et al. Clinical evaluation of urinary excretion of liver-type fatty acid-binding protein as a marker for the monitoring of chronic kidney disease: a multicenter trial. J Lab Clin Med. 2005;145(3):125-133.
doi pubmed - Nath KA. Tubulointerstitial changes as a major determinant in the progression of renal damage. Am J Kidney Dis. 1992;20(1):1-17.
doi - Ziyadeh FN. Significance of tubulointerstitial changes in diabetic renal disease. Kidney Int Suppl. 1996;54:S10-13.
pubmed - Singh DK, Winocour P, Farrington K. Mechanisms of disease: the hypoxic tubular hypothesis of diabetic nephropathy. Nat Clin Pract Nephrol. 2008;4(4):216-226.
doi pubmed - Suzuki K, Babazono T, Murata H, Iwamoto Y. Clinical significance of urinary liver-type fatty acid-binding protein in patients with diabetic nephropathy. Diabetes Care. 2005;28(8):2038-2039.
doi pubmed - Kamijo-Ikemori A, Sugaya T, Yasuda T, Kawata T, Ota A, Tatsunami S, Kaise R, et al. Clinical significance of urinary liver-type fatty acid-binding protein in diabetic nephropathy of type 2 diabetic patients. Diabetes Care. 2011;34(3):691-696.
doi pubmed - Kim SS, Song SH, Kim IJ, Yang JY, Lee JG, Kwak IS, Kim YK. Clinical implication of urinary tubular markers in the early stage of nephropathy with type 2 diabetic patients. Diabetes Res Clin Pract. 2012;97(2):251-257.
doi pubmed - Araki S, Haneda M, Koya D, Sugaya T, Isshiki K, Kume S, Kashiwagi A, et al. Predictive effects of urinary liver-type fatty acid-binding protein for deteriorating renal function and incidence of cardiovascular disease in type 2 diabetic patients without advanced nephropathy. Diabetes Care. 2013;36(5):1248-1253.
doi pubmed - Nielsen SE, Sugaya T, Hovind P, Baba T, Parving HH, Rossing P. Urinary liver-type fatty acid-binding protein predicts progression to nephropathy in type 1 diabetic patients. Diabetes Care. 2010;33(6):1320-1324.
doi pubmed - Panduru NM, Forsblom C, Saraheimo M, Thorn L, Bierhaus A, Humpert PM, Groop PH. Urinary liver-type fatty acid-binding protein and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care. 2013;36(7):2077-2083.
doi pubmed - Maeda Y, Suzuki A, Ishii J, Sekiguchi-Ueda S, Shibata M, Yoshino Y, Asano S, et al. Level of urinary liver-type fatty acid-binding protein is associated with cardiac markers and electrocardiographic abnormalities in type-2 diabetes with chronic kidney disease stage G1 and G2. Heart Vessels. 2015;30(3):362-368.
doi pubmed - Kamijo-Ikemori A, Sugaya T, Sekizuka A, Hirata K, Kimura K. Amelioration of diabetic tubulointerstitial damage in liver-type fatty acid-binding protein transgenic mice. Nephrol Dial Transplant. 2009;24(3):788-800.
doi pubmed - CIMIC HOLDINGS Co. Ltd. [Online] Available at: https://www.fabp.jp/assets/files/documents/renischem_ifu1.pdf, 2012 Accessed on 17 January 2017
- Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982-992.
doi pubmed - Ito H, Komatsu Y, Mifune M, Antoku S, Ishida H, Takeuchi Y, Togane M. The estimated GFR, but not the stage of diabetic nephropathy graded by the urinary albumin excretion, is associated with the carotid intima-media thickness in patients with type 2 diabetes mellitus: a cross-sectional study. Cardiovasc Diabetol. 2010;9:18.
doi pubmed - Ito H, Oshikiri K, Mifune M, Abe M, Antoku S, Takeuchi Y, Togane M, et al. The usefulness of the revised classification for chronic kidney disease by the KDIGO for determining the frequency of diabetic micro- and macroangiopathies in Japanese patients with type 2 diabetes mellitus. J Diabetes Complications. 2012;26(4):286-290.
doi pubmed - Ito H, Takeuchi Y, Ishida H, Otawa A, Shibayama A, Antoku S, Abe M, et al. Mild anemia is frequent and associated with micro- and macroangiopathies in patients with type 2 diabetes mellitus. J Diabetes Investig. 2010;1(6):273-278.
doi pubmed - Ito H, Omoto T, Abe M, Matsumoto S, Shinozaki M, Nishio S, Antoku S, et al. Relationships between the duration of illness and the current status of diabetes in elderly patients with type 2 diabetes mellitus. Geriatr Gerontol Int. 2017;17(1):24-30.
doi pubmed - Ito H, Nakashima M, Meguro K, Furukawa H, Yamashita H, Takaki A, Yukawa C, et al. Flow Mediated Dilatation Is Reduced with the Progressive Stages of Glomerular Filtration Rate and Albuminuria in Type 2 Diabetic Patients without Coronary Heart Disease. J Diabetes Res. 2015;2015:728127.
doi pubmed - Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837-853.
doi - Zoungas S, Chalmers J, Neal B, Billot L, Li Q, Hirakawa Y, Arima H, et al. Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med. 2014;371(15):1392-1406.
doi pubmed - Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63(1):225-232.
doi pubmed - Katayama S, Moriya T, Tanaka S, Yajima Y, Sone H, Iimuro S, Ohashi Y, et al. Low transition rate from normo- and low microalbuminuria to proteinuria in Japanese type 2 diabetic individuals: the Japan Diabetes Complications Study (JDCS). Diabetologia. 2011;54(5):1025-1031.
doi pubmed - Hasegawa K, Wakino S, Simic P, Sakamaki Y, Minakuchi H, Fujimura K, Hosoya K, et al. Renal tubular Sirt1 attenuates diabetic albuminuria by epigenetically suppressing Claudin-1 overexpression in podocytes. Nat Med. 2013;19(11):1496-1504.
doi pubmed - Yamamoto T, Noiri E, Ono Y, Doi K, Negishi K, Kamijo A, Kimura K, et al. Renal L-type fatty acid - binding protein in acute ischemic injury. J Am Soc Nephrol. 2007;18(11):2894-2902.
doi pubmed - Ishimitsu T, Ohta S, Saito M, Teranishi M, Inada H, Yoshii M, Minami J, et al. Urinary excretion of liver fatty acid-binding protein in health-check participants. Clin Exp Nephrol. 2005;9(1):34-39.
doi pubmed - von Eynatten M, Baumann M, Heemann U, Zdunek D, Hess G, Nawroth PP, Bierhaus A, et al. Urinary L-FABP and anaemia: distinct roles of urinary markers in type 2 diabetes. Eur J Clin Invest. 2010;40(2):95-102.
doi pubmed - Nakamura T, Sugaya T, Kawagoe Y, Ueda Y, Koide H. Effect of pioglitazone on urinary liver-type fatty acid-binding protein concentrations in diabetes patients with microalbuminuria. Diabetes Metab Res Rev. 2006;22(5):385-389.
doi pubmed - Nakamura T, Sugaya T, Koide H. Angiotensin II receptor antagonist reduces urinary liver-type fatty acid-binding protein levels in patients with diabetic nephropathy and chronic renal failure. Diabetologia. 2007;50(2):490-492.
doi pubmed - Nakamura T, Fujiwara N, Sato E, Ueda Y, Sugaya T, Koide H. Renoprotective Effects of Various Angiotensin II Receptor Blockers in Patients with Early-Stage Diabetic Nephropathy. Kidney Blood Press Res. 2010;33(3):213-220.
doi pubmed - Abe M, Oikawa O, Okada K, Soma M. Urinary angiotensin-converting enzyme 2 increases in diabetic nephropathy by angiotensin II type 1 receptor blocker olmesartan. J Renin Angiotensin Aldosterone Syst. 2015;16(1):159-164.
doi pubmed - Nielsen SE, Sugaya T, Tarnow L, Lajer M, Schjoedt KJ, Astrup AS, Baba T, et al. Tubular and glomerular injury in diabetes and the impact of ACE inhibition. Diabetes Care. 2009;32(9):1684-1688.
doi pubmed - Abe M, Maruyama N, Okada K, Matsumoto S, Matsumoto K, Soma M. Additive antioxidative effects of azelnidipine on angiotensin receptor blocker olmesartan treatment for type 2 diabetic patients with albuminuria. Hypertens Res. 2011;34(8):935-941.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


