| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 6, Number 5, October 2014, pages 388-391
Recurrent Arterial and Venous Thromboemboli as Initial Presentation of Acute Promyelocytic Leukemia
Felix Trottier-Telliera, Madeleine Durandb, Christophe Kolanc, Robert Wistaffc, Paul Van Nguyenc, Mikhael Laskineb, d
aUniversite de Montreal, Montreal, Canada
bDepartment of Medicine, Hopital Hotel-Dieu, CRCHUM, Montreal, Canada
cDepartment of Medicine, Hopital Hotel-Dieu, CHUM, Montreal, Canada
dCorresponding Author: Mikhael Laskine, Department of Medicine, Hotel-Dieu Hospital, Centre Hospitalier de l’Universite de Montreal, 3840 St-Urbain Street, Door 4-411, Montreal, Quebec H2W 1T8, Canada
Manuscript accepted for publication May 15, 2014
Short title: Recurrent Arterial and Venous Thromboemboli
doi: https://doi.org/10.14740/jocmr1864w
| Abstract | ▴Top |
We report a case of a 52-year-old Caucasian woman diagnosed with a synchronic arterial and venous thrombosis as an initial presentation of an acute promyelocytic leukemia (APL). After the diagnosis, the patient was treated with all trans-retinoic acid and arsenic chemotherapy concomitant to systemic anticoagulation. This treatment regimen led to a complete remission and absence of relapse of the thrombosis or APL during the follow-up. To our knowledge, this presentation is the second case in the literature. We use this opportunity to emphasize the importance of performing a complete medical evaluation in cases of unusual thromboembolic events.
Keywords: Acute promyelocytic leukemia; All trans-retinoic acid and arsenic treatment; Arterial and venous thrombosis; Systemic anticoagulation
| Introduction | ▴Top |
Vascular thromboemboli are among the most common medical problems presenting in the adult population. Large-scale retrospective studies show an incidence of first-time venous thromboemboli (combined deep venous thrombosis (DVT) and pulmonary embolism (PE)) of 1.92 per 1,000 persons per year with a recurrence rate of 7.7% per year [1]. Arterial events are even more common, with a prevalence for adult populations of 3-10% for peripheral artery disease and 2.8% for stroke [2, 3]. Although often considered distinct pathological entities, arterial and venous thrombosis have much in common. They share risk factors such as age, obesity, diabetes and hereditary or acquired thrombophilias [4, 5]. Current studies also suggest that a history of venous thromboembolic disease represents a significant risk of future cardiovascular disease, suggesting that arterial and venous thromboembolisms share common pathways [6, 7]. Nonetheless, very few diseases present with both arterial and venous thromboembolisms. Among these, classical causes include antiphospholipid syndrome, heparin-induced thrombocytopenia (HIT), Bechet’s syndrome, neoplasia-associated thrombosis, and myeloproliferative disorders. In this case report, we describe an unusual combined arterial and venous thrombosis and we emphasize on the medical evaluation required by such a case.
| Case Report | ▴Top |
A 52-year-old female presented to the emergency department for acute pain and numbness in the left arm. She was known for arterial hypertension and gout, and was a former 30 pack-year smoker and obese (BMI 37). Two weeks prior to this presentation, she had been diagnosed with extensive DVT of unknown origin of the right leg (popliteal, tibial posterior and great saphenous veins) with bilateral legs superficial venous thrombosis. She was started on enoxaparin 1 mg/kg SC BID.
On arrival, she complained of intense left hand pain that suddenly developed a few hours earlier, accompanied by progressive left hand weakness. She denied having night sweats, fever, recurrent infections or bleeding. She had noted a slight subjective weight loss and fatigue in the last 6 weeks. No neurological, mucocutaneous or visual symptoms were reported. She was compliant with her medication.
She was hemodynamically stable. A complete physical examination was unremarkable, except for the exquisite left hand pain with coldness, pallor and pulselessness up to the elbow.
Acute left hand ischemia was suspected and an angiography scanner was performed. It confirmed the diagnosis of acute thrombosis of the left axillary artery and chronic thrombosis of the left subclavian artery with occlusive emboli in distal left ulnar artery. She underwent local arterial thrombolysis and then was started on IV heparin with fast symptoms improvement.
Local thrombolysis was performed twice again over the next 10 days because of recurrent episodes of left arm ischemia with thrombi progression in the brachial, radial and ulnar arteries. The decision to switch to IV argatroban was made due to repeated episodes of thrombosis with therapeutic levels of IV heparin, thus suspecting a “heparin resistance” (Fig. 1).
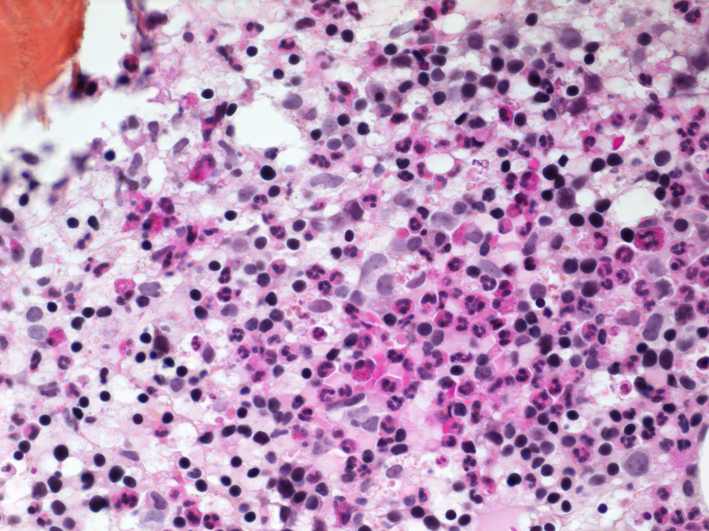 Click for large image | Figure 1. CAT scan showing thrombosis of the left subclavian and axillary arteries. |
The patient was sent home with a consolidation treatment of arsenic and ATRA. No signs of recurrence were observed after two cycles of consolidation. At the time of discharge, the cause of the recurrent thrombosis was clearly identified as APL. This pathology is known for its strong thrombogenic potential and it led to multiple recurrent thrombosis while on therapeutic dose of IV heparin with suspicion of “heparin resistance”. Once APL was confirmed to be in complete remission, the cause of these severe thrombosis was therefore controlled and the patient was switched back to LMWH enoxaparin 1.5mg/kg DIE SC for long-term anticoagulation. There was no recurrence of thromboembolic events thereafter.
| Discussion | ▴Top |
APL is a hematopoietic neoplasia of the acute myeloid leukemia (AML) group. This disorder is characterised by an excess of atypical promyelocytes in the bone marrow and peripheral blood. The cytogenetic anomaly t(15:17) is a classic finding and is used for diagnostic confirmation of APL according to the WHO classification system of AML [8]. This translocation induces a fusion between promyelocytic leukemia (PML) gene and retinoic acid receptor alpha (RARalpha) gene creating a PML-RARalpha gene inducing excessive medullary production of promyelocytes through a PML-RARalpha protein. Five to twenty percent of AML cases are classified as APL [9]. The natural evolution of APL is very aggressive with median survival of less than 1 month, but recent advances in therapy with combined treatment of ATRA and arsenic provide excellent response with complete remission up to 90-95% of patients [10]. By binding to RARalpha moiety of the PML-RARA oncoprotein, ATRA leads to differentiation from promyelocytic malignant cells to mature neutrophils while arsenic binds to the PML moiety and induces apoptosis and partial differentiation of the promyelocytes cells [11, 12].
APL has been associated with important coagulopathy, which can present by bleeding or thrombosis. Hemorrhagic complications have been recognized for decades as an important clinical feature of APL and as the leading cause of early mortality [13]. The pathogenesis of APL coagulopathy is incompletely understood. Initially attributed to DIC, recent publications have shown a complex interaction of coagulation activation and hyperfibrinolysis in APL considerably different from DIC [14]. Thrombosis complications, although increasingly identified as part of the APL coagulopathy spectrum, are less understood and underreported compared with bleedings. Nevertheless, elevated white blood cell count, presence of FLT3-ITD and expression of CD2 were found to be associated with an increased risk of thrombosis [15]. Pathogenesis hypotheses of APL-related thrombosis are direct expression of tissue factor and cancer procoagulant and prothrombogenic cytokines production by abnormal promyelocytes. Concerns have been raised since it was observed that APL thrombosis events are more frequently reported since the introduction of ATRA. Although not fully understood, direct effects of ATRA that might promote thrombosis include increased production of endothelial thrombogenic stimulating cytokines by the APL cells and increased adhesion of the APL cells to endothelial cells [16].
Both venous and arterial thromboembolic events have been described with APL. A recent review article reported 94 cases of major APL-related thrombosis [17]. The majority (84%) of these thrombosis occurred before or during induction therapy and 55% were arterial compared with 45% venous. The most frequent locations of thrombosis were DVT/PE (28.7%), cardiac events (26.6%) and strokes (21.3%) for a combined total of 76.6% of the thrombotic events. Of note, five patients presented acute limb ischemia and six patients presented with multiple thrombotic events including two combined venous and arterial thrombosis (one splenic infarct and DVT and one acute limb ischemia and PE). In only one of these two cases, thrombosis was the initial complain.
Therefore, the case presented in this paper was a rare presentation of APL. To our knowledge, it is only the second case reported of acute arterial thrombosis combined with DVT/EP as a presentation of APL. Unfortunately, the diagnosis was delayed by the absence of blast cells in peripheral blood on initial examination. Nevertheless, treatment was rapidly successful for the APL per se and for the thromboembolic events once the combined ATRA and arsenic induction protocol was started.
As stated above, obesity has been recognized as an important risk factor for both venous and arterial thrombosis. The patient presented here had class II obesity, which could certainly contribute to the clinical thrombosis. As the medical investigation demonstrated, the obesity was not the primary cause of the thrombotic events and it would be highly unlikely that long standing obesity would be the main cause of brutal recurrent thrombosis.
In conclusion, venous and arterial thromboembolic events are among the most common medical challenges encountered by internal medicine teams. A complete investigation such as the one described in this case report would be a resource misuse if applied to a majority of thromboembolic cases. However, a search for the cause of a thrombosis should always be undertaken and must be tailored to each patient’s presentation. This investigation could go from anamnesis only to extensive laboratory and imaging procedures. We believe it is our role as internists to offer a thorough medical evaluation when challenged with recurrent or unusual presentation of thromboembolic arterial or venous events. In this context, some of the most important etiologies to investigate would include solid and hematologic neoplasia, vasculitis, thrombophilias, HIT syndrome and antiphospholipid syndrome. An accurate diagnosis is of prime value since these various pathologies present widely different prognosis and often require specific management besides anticoagulation.
We feel this case report is a perfect example to stress the importance of a rigorous and complete investigation that some thromboembolic events call for. The goal of this paper is to help medical teams keep a high level of suspicion when facing unusual thromboembolic events and improve the knowledge concerning APL-related coagulopathy and its increased risk of thrombosis.
Grant Support
No.
| References | ▴Top |
- Cushman M, Tsai AW, White RH, Heckbert SR, Rosamond WD, Enright P, Folsom AR. Deep vein thrombosis and pulmonary embolism in two cohorts: the longitudinal investigation of thromboembolism etiology. Am J Med. 2004;117(1):19-25.
doi pubmed - Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45(Suppl S):S5-67.
doi pubmed - Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM,
et al . Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6-e245.
doi pubmed - Tsai AW, Cushman M, Rosamond WD, Heckbert SR, Polak JF, Folsom AR. Cardiovascular risk factors and venous thromboembolism incidence: the longitudinal investigation of thromboembolism etiology. Arch Intern Med. 2002;162(10):1182-1189.
doi pubmed - Ageno W, Becattini C, Brighton T, Selby R, Kamphuisen PW. Cardiovascular risk factors and venous thromboembolism: a meta-analysis. Circulation. 2008;117(1):93-102.
doi pubmed - van Schouwenburg IM, Gansevoort RT, Mahmoodi BK, Visser MM, Kluin-Nelemans HC, Lijfering WM, Veeger NJ. Increased risk of arterial thromboembolism after a prior episode of venous thromboembolism: results from the Prevention of REnal and Vascular ENd stage Disease (PREVEND) Study. Br J Haematol. 2012;159(2):216-222.
doi pubmed - Becattini C, Vedovati MC, Ageno W, Dentali F, Agnelli G. Incidence of arterial cardiovascular events after venous thromboembolism: a systematic review and a meta-analysis. J Thromb Haemost. 2010;8(5):891-897.
pubmed - Jaffe ES, Harris NL, Stein H, Vardiman JW, editors. World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press; Lyon, France; 2001.
- Yamamoto JF, Goodman MT. Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002. Cancer Causes Control. 2008;19(4):379-390.
doi pubmed - Lo-Coco F, Avvisati G, Vignetti M, Thiede C, Orlando SM, Iacobelli S, Ferrara F,
et al . Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med. 2013;369(2):111-121.
doi pubmed - Elliott S, Taylor K, White S, Rodwell R, Marlton P, Meagher D, Wiley J,
et al . Proof of differentiative mode of action of all-trans retinoic acid in acute promyelocytic leukemia using X-linked clonal analysis. Blood. 1992;79(8):1916-1919.
pubmed - Shao W, Fanelli M, Ferrara FF, Riccioni R, Rosenauer A, Davison K, Lamph WW,
et al . Arsenic trioxide as an inducer of apoptosis and loss of PML/RAR alpha protein in acute promyelocytic leukemia cells. J Natl Cancer Inst. 1998;90(2):124-133.
doi pubmed - Cordonnier C, Vernant JP, Brun B, Heilmann MG, Kuentz M, Bierling P, Farcet JP,
et al . Acute promyelocytic leukemia in 57 previously untreated patients. Cancer. 1985;55(1):18-25.
doi - Breen KA, Grimwade D, Hunt BJ. The pathogenesis and management of the coagulopathy of acute promyelocytic leukaemia. Br J Haematol. 2012;156(1):24-36.
doi pubmed - Breccia M, Avvisati G, Latagliata R, Carmosino I, Guarini A, De Propris MS, Gentilini F,
et al . Occurrence of thrombotic events in acute promyelocytic leukemia correlates with consistent immunophenotypic and molecular features. Leukemia. 2007;21(1):79-83.
doi pubmed - Barbui T, Finazzi G, Falanga A. The impact of all-trans-retinoic acid on the coagulopathy of acute promyelocytic leukemia. Blood. 1998;91(9):3093-3102.
pubmed - Rashidi A, Silverberg ML, Conkling PR, Fisher SI. Thrombosis in acute promyelocytic leukemia. Thromb Res. 2013;131(4):281-289.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


