| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Letter to the Editor
Volume 5, Number 3, June 2013, pages 247-248
Subjective Signs of Rhegmatogenous Retinal Detachment Associated With Acute Posterior Vitreous Detachment
Ken-ichi Satoa, b, Shin-ichi Nishimuraa
aDepartment of Ophthalmology, Nikko Memorial Hospital, 1-5-13 Shintomi-cho, Muroran, Hokkaido, Japan
bCorresponding author: Ken-ichi Sato, Department of Ophthalmology, Nikko Memorial Hospital, 1-5-13 Shintomi-cho, Muroran 051-8501, Japan
Manuscript accepted for publication January 04, 2013
Short title: Subjective signs of Rhegmatogenous Retinal Detachment
doi: https://doi.org/10.4021/jocmr1243w
| To the Editor | ▴Top |
Despite recent anatomical successes of surgical treatment for rhegmatogenous retinal detachment (RRD), reattachment fails in 1.1-2.5% of cases [1-3]. In addition, even in cases of reattachment, some patients continue to show poor functional results [1, 2]. Prevention of RRD is therefore undoubtedly desirable. We retrospectively examined subjective signs in patients who underwent surgery for RRD to determine whether they could have received prophylactic laser treatment [4] at an early stage of retinal tear only or minimal retinal detachment.
Subjects were 34 consecutive patients (34 eyes; 10 females; mean age ± SD: 58 ± 11 years) who presented with RRD associated with acute posterior vitreous detachment (PVD) on initial visit to Nikko Memorial Hospital. All patients subsequently underwent pars plana vitrectomy between April 2009 and March 2012; 3 were excluded due to complications related to obvious vitreous hemorrhage. Cases with traumatic or atopic RRD were not included. At the initial visit, patients were interviewed about subjective visual symptoms.
Informed consent was obtained from all subjects prior to surgery and the study adhered to the tenets of the Declaration of Helsinki.
Fourteen patients (41%) visited the hospital because of floaters only or visual field disturbance following floaters; the remainder visited due to visual field disturbance, presumably caused by RRD, with no experience of floaters. Only one patient complained of photopsia with initial floaters. Of those who initially experienced floaters, 2 patients took more than one month from onset to experiencing visual field disturbance (Fig. 1); this late-visit group was significantly younger than the other patients (P = 0.007, Welch’s t test).
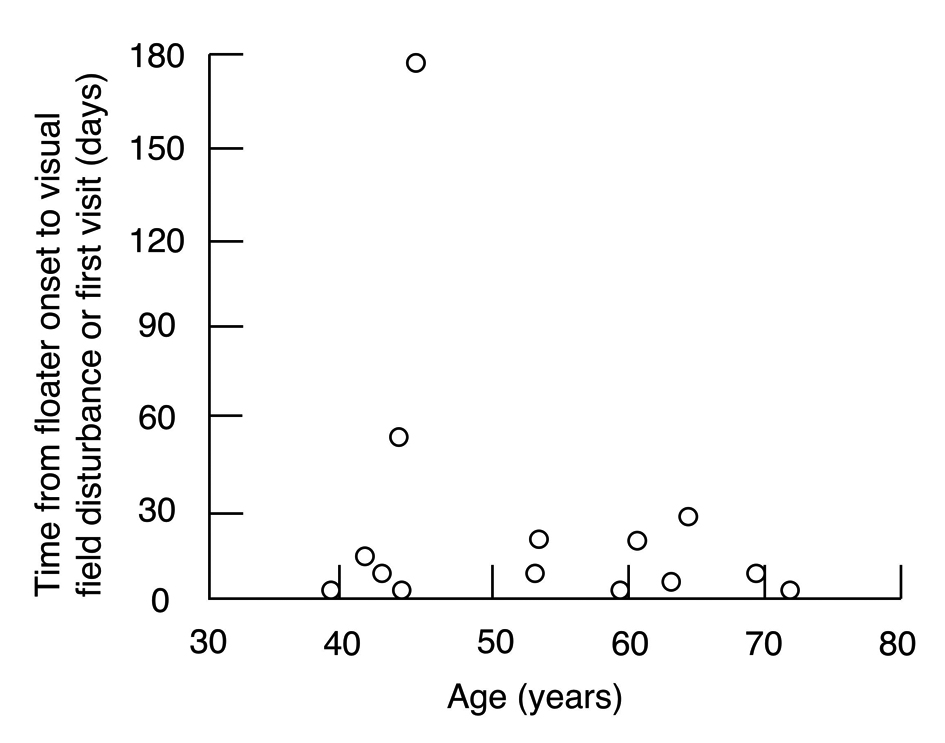 Click for large image | Figure 1. Correlation between age and time from onset of floaters to experiencing visual field disturbance. |
A significant proportion of patients with acute PVD complain of monocular floaters [5]. In the present study, we therefore considered the onset of floaters to be a potential sign of acute PVD. Patients also showing apparent vitreous hemorrhage on initial visit were excluded from the study because associated floaters may bias the patients’ actions in seeking a consultation.
Of the patients without preceding floaters, approximately 60% visited due to visual field disturbance caused by RRD. As a result, it was too late to perform prophylactic laser treatment by the time the subjective symptoms led to consultation.
In some of the relatively young patients with preceding floaters, there was quite a long period of time from onset of the initial floater to experiencing visual field disturbance. Since vitreous syneresis has yet to advance in the young generally [6], the tamponade effect of gel-state vitreous or weak vitreous contractions may result in late-onset RRD. Thus, consultation immediately after the onset of floaters might enable prophylactic laser photocoagulation to be performed at an early stage when only retinal tear or minimal retinal detachment has occurred. This suggests the importance of awareness of this state among the relatively young.
Several studies suggest that patients with symptomatic PVD do not necessarily need scheduled reexamination if there are no pigmented cells in the vitreous, vitreous hemorrhage, or retinal hemorrhage at initial fundus examination [7-9]. Nevertheless, considering the potential for late-onset retinal breaks or RRD, it may be worth patients younger than 50 to schedule a follow-up examination after initial consultation.
The study had certain limitations. This was a single-center study and there were a limited number of patients. A larger scale study is warranted to verify the results.
Grant Support
None.
| References | ▴Top |
- Heimann H, Zou X, Jandeck C, Kellner U, Bechrakis NE, Kreusel KM, Helbig H,
et al . Primary vitrectomy for rhegmatogenous retinal detachment: an analysis of 512 cases. Graefes Arch Clin Exp Ophthalmol. 2006;244(1):69-78.
pubmed - Schneider EW, Geraets RL, Johnson MW. Pars plana vitrectomy without adjuvant procedures for repair of primary rhegmatogenous retinal detachment. Retina. 2012;32(2):213-219.
pubmed - Kinori M, Moisseiev E, Shoshany N, Fabian ID, Skaat A, Barak A, Loewenstein A,
et al . Comparison of pars plana vitrectomy with and without scleral buckle for the repair of primary rhegmatogenous retinal detachment. Am J Ophthalmol. 2011;152(2):291-297 e2.
pubmed - Kazahaya M. Prophylaxis of retinal detachment. Semin Ophthalmol. 1995;10(1):79-86.
pubmed - Hollands H, Johnson D, Brox AC, Almeida D, Simel DL, Sharma S. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302(20):2243-2249.
pubmed - Le Goff MM, Bishop PN. Adult vitreous structure and postnatal changes. Eye (Lond). 2008;22(10):1214-1222.
pubmed - Richardson PS, Benson MT, Kirkby GR. The posterior vitreous detachment clinic: do new retinal breaks develop in the six weeks following an isolated symptomatic posterior vitreous detachment? Eye (Lond). 1999;13(Pt 2):237-240.
pubmed - van Overdam KA, Bettink-Remeijer MW, Klaver CC, Mulder PG, Moll AC, van Meurs JC. Symptoms and findings predictive for the development of new retinal breaks. Arch Ophthalmol. 2005;123(4):479-484.
pubmed - Coffee RE, Westfall AC, Davis GH, Mieler WF, Holz ER. Symptomatic posterior vitreous detachment and the incidence of delayed retinal breaks: case series and meta-analysis. Am J Ophthalmol. 2007;144(3):409-413.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


