| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Case Report
Volume 15, Number 10-11, December 2023, pages 456-460
Cardiac Amyloidosis Patient With Cardiac Conduction Disturbances
Keisuke Hosonoa, Shunsuke Kiuchia, b, Takanori Ikedaa
aDivision of Cardiovascular Medicine, Department of Internal Medicine, Toho University Faculty of Medicine, Ota-ku, Tokyo 143-8541, Japan
bCorresponding Author: Shunsuke Kiuchi, Division of Cardiovascular Medicine, Department of Internal Medicine, Toho University Faculty of Medicine, Ota-ku, Tokyo 143-8541, Japan
Manuscript submitted October 16, 2023, accepted November 30, 2023, published online December 9, 2023
Short title: CA Patient With Cardiac Conduction Disturbances
doi: https://doi.org/10.14740/jocmr5051
| Abstract | ▴Top |
Transthyretin cardiac amyloidosis (ATTR-CA) has recently been diagnosed more because of advances in diagnostic techniques, such as 99mTc-labeled pyrophosphate (99mTc-PYP) scintigraphy. ATTR-CA remains poorly diagnosed by many physicians, except for cardiologists and neurologists, and by patients. In this manuscript, we present a patient who was recommended to undergo a close examination but developed cardiac conduction disturbances and defects due to delays in the examination and treatment initiation. The patient was a 72-year-old Japanese man treated for hypertension at our hospital for approximately 30 years. The patient was diagnosed with left ventricular hypertrophy at 62 years old and hospitalized for heart failure at 68 years old. ATTR-CA was suspected by 99mTc-PYP scintigraphy performed at 70 years old, and a skin biopsy was performed. However, the skin biopsy did not confirm the diagnosis, and myocardial biopsy was recommended, which was declined by the patient. He finally consented to myocardial biopsy 2 years later, leading to the diagnosis of ATTR-CA at 72 years old. However, the patient had atrial fibrillation and a complete atrioventricular block. If ATTR-CA were widely recognized and understood, it might have been diagnosed and treated before the cardiac conduction disturbances appeared. It is essential to have an understanding and appropriate examinations for ATTR-CA based on sufficient explanation and consent.
Keywords: Transthyretin cardiac amyloidosis; Endomyocardial biopsy; 99mTc-labeled pyrophosphate scintigraphy; Left ventricular hypertrophy; Heart failure with preserved ejection fraction
| Introduction | ▴Top |
Recently, transthyretin cardiac amyloidosis (ATTR-CA) has been diagnosed more because of advances in diagnostic techniques, such as 99mTc-labeled pyrophosphate (99mTc-PYP) scintigraphy [1, 2]. Cardiac magnetic resonance (CMR) imaging and transthoracic echocardiographic strain measurements help in the diagnosis of ATTR-CA; however, proof of amyloid deposition by tissue biopsy, including endomyocardial biopsy (EMB), is necessary to confirm the diagnosis. The amyloid detection rate by biopsy from skin, gastrointestinal tract, and salivary glands varies from 14% to 100%, depending on the type of ATTR-CA. In this regard, the amyloid detection rate by EMB is estimated to be almost 100% [3]. EMB is a highly invasive technique; thus, some patients are hesitant to undergo this procedure. Additionally, we consider that many patients are still unaware of ATTR-CA, which may be a factor in their reluctance to undergo EMB. In this manuscript, we present a patient suspected of having ATTR-CA and recommended close examination; however, irreversible cardiac conduction disturbances occurred because of delays in the examination and treatment initiation.
| Case Report | ▴Top |
We present the case of a 72-year-old Japanese man who has been treated for hypertension at the Department of General Medicine for the 40 years of his life. He complained of palpitations at 58 years old; however, his troponin-I levels were under the detection limit. The symptoms had persisted for 4 years, but electrocardiogram (ECG) showed no abnormal findings (Fig. 1a). In contrast, transthoracic echocardiography (TTE) performed during the same time showed global left ventricular hypertrophy (LVH) of 13 mm, considered by the previous physician to be hypertensive changes, while the contractility was maintained (the left ventricular ejection fraction (LVEF) was 65.4%) (Fig. 1b). The patient had elevated brain natriuretic peptide (BNP) levels, reaching 385.2 pg/mL, at 68 years old. A few months later, the patient had dyspnea on exertion, and a chest X-ray showed accumulation of pleural effusion. ECG showed a new complete left bundle branch block (Fig. 1c). TTE showed left ventricular end-diastolic and end-systolic diameters and left atrial diameters of 55.5 mm, 41.4 mm, and 55.8 mm, respectively. The left ventricular wall was diffusely thickened (16 mm), and the LVEF was reduced to 49.6% (Fig. 1d). BNP showed elevated levels of 797.9 pg/mL, and the patient was diagnosed with congestive heart failure and referred to a cardiologist for the first time. The patient had a medical history of chronic kidney disease (CKD) since he was 60 years old. The patient had a creatinine level of 2.08 mg/dL and an estimated glomerular filtration rate of 25.9 mL/min/1.73 m2. Occult hematuria was negative, whereas proteinuria, although not quantitatively evaluated, was detected. Troponin-I during hospitalization was 0.25 ng/mL (normal range: < 0.014 ng/mL), and the patient underwent coronary artery angiography with a small amount of contrast medium because of CKD. Coronary artery stenosis was not detected, and EMB to differentiate a hypertrophic heart was not performed because the patient did not provide consent. Contrast-enhanced CMR could not be performed due to CKD; however, alpha-galactosidase A activity was normal, ruling out Fabry disease. After hospitalization, medication treatment, including beta-blockers, angiotensin II type 1a receptor blockers, and loop diuretics, rapidly improved heart failure signs and symptoms. Because the LVEF improved to 57.6% with only medication adjustment, the patient has been suspected of heart failure with preserved ejection fraction (HFpEF) due to hypertensive heart disease (HHD). Treatment was continued in the outpatient clinic. 99mTc-PYP scintigraphy became available at our hospital when the patient was 70 years old. Following the Kumamoto criteria [4], the patient had two positive results (left ventricular posterior wall thickness of 14.6 mm and QRS duration of 182 ms); therefore, we performed 99mTc-PYP scintigraphy, which showed strong accumulation in the myocardium (Fig. 2). No Bence-Jones protein was detected in the urine, and no M-protein was seen in the blood. Based on these results, ATTR-CA was highly suspected, and EMB and informed consent were recommended for patient; however, the patient did not accept EMB and accepted a less invasive skin biopsy. Skin biopsy showed no findings suggestive of amyloidosis. The patient requested a second opinion from another hospital and was advised to undergo EMB, as was recommended by the doctors at our hospital; however, the patient also did not accept it. Making a definitive diagnosis of ATTR-CA became difficult, and at 71 years old, the patient had a complete atrioventricular block and atrial fibrillation (Fig. 1e). We suggested pacemaker implantation for general malaise; however, the patient did not accept it. Skin biopsies were performed twice during the course of the disease, but no amyloid deposition was detected. The hospital where the patient was seen for a third opinion also recommended EMB, which was finally performed at 72 years old at that hospital. EMB results showed ATTR-CA; the patient was diagnosed as wild type by a genetic test. The diagnosis was confirmed 4 years after the cardiologist’s visit and 2 years after the positive 99mTc-PYP scintigraphy confirmation. He is currently starting treatment with tafamidis and is considering pacemaker implantation.
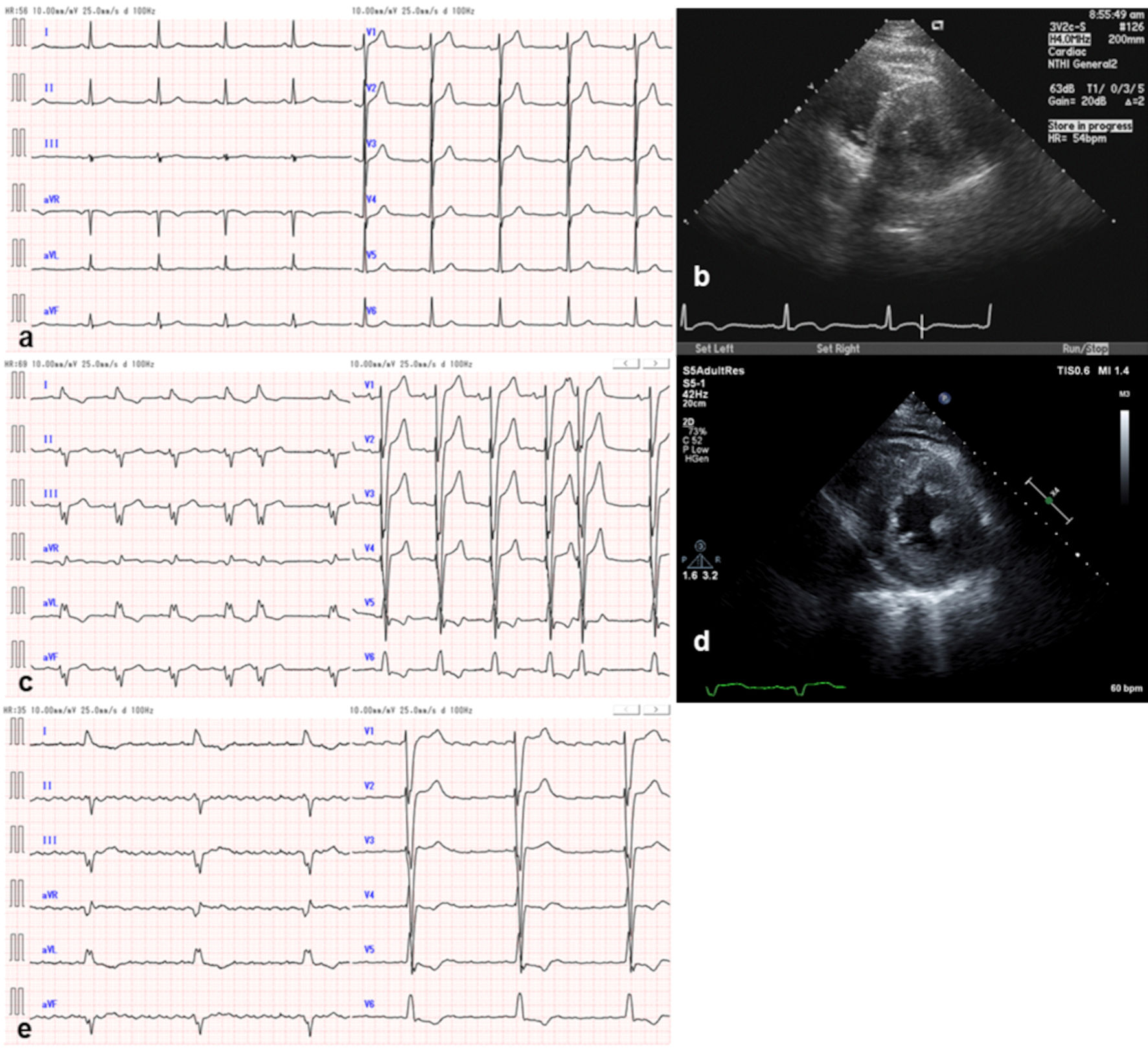 Click for large image | Figure 1. Electrocardiographic and transthoracic echocardiographic findings. At 62 years old, (a) PQ duration was 176 ms, QRS duration was 96 ms, and (b) global left ventricular wall thickness was approximately 13 mm. At 68 years old, (c) PQ duration was 198 ms, QRS duration was 174 ms, and (d) left ventricular wall thickness was approximately 16 mm. At 71 years old, (e) atrial fibrillation and complete atrioventricular block occurred; QRS duration was 190 ms. |
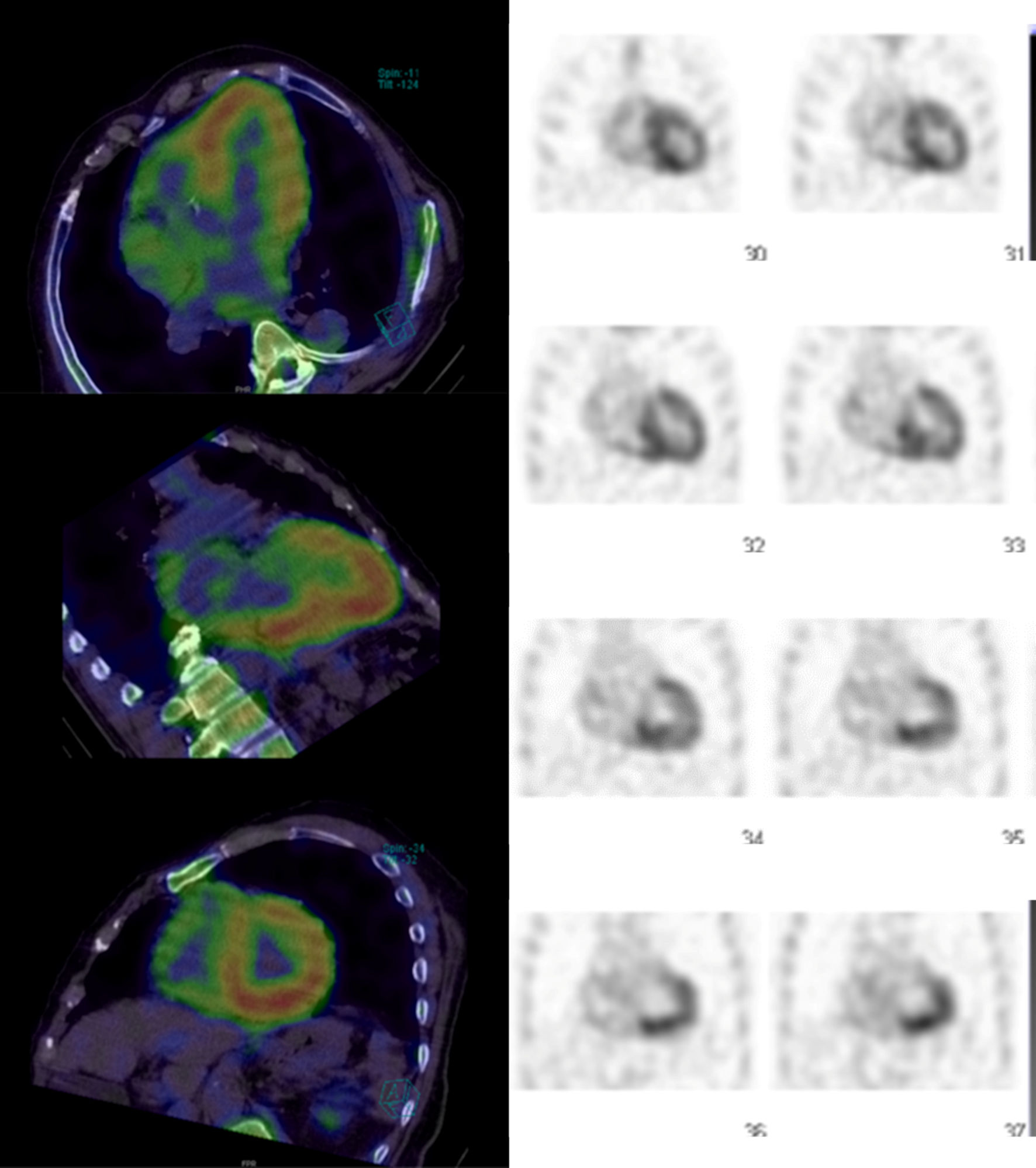 Click for large image | Figure 2. 99mTc-labeled pyrophosphate scintigraphy image. 99mTc-labeled pyrophosphate scintigraphy shows strong accumulation in the left ventricular wall. |
| Discussion | ▴Top |
Cardiac amyloidosis (CA) is a secondary cardiomyopathy caused by the accumulation of abnormal proteins, called amyloid, in the myocardium [5]. CA has three main types: acquired monoclonal immunoglobulin light chain amyloidosis (AL amyloidosis); variant transthyretin amyloidosis (ATTRv); and wild-type transthyretin amyloidosis (ATTRwt). The prevalence of ATTRwt, in particular, has increased dramatically because of the aged population and advances in diagnostic technology [1]. Additionally, it has been reported that 13% of elderly patients with HFpEF have been diagnosed with ATTR-CA [6]. HFpEF includes not only cases with a clinical diagnosis of HHD and hypertrophic cardiomyopathy, but also many cases of ATTR-CA [7]. In Japan, ATTRv is reported from all over the country, mainly from areas of concentration such as Nagano and Kumamoto prefectures; however, ATTRwt is reported from all over the country regardless of the area of concentration. Although not seen in the present case, carpal tunnel syndrome is a complication in 45% of patients with ATTRwt [8], and polyneuropathy is often seen in ATTRv [9], so these are leading us to suspect ATTR-CA. Transthyretin (TTR) is a soluble human plasma protein that can be converted into amyloid by dissociation of the homotetramer into monomers. The drug tafamidis binds to the TTR tetramer and dramatically slows dissociation, thereby efficiently inhibiting aggregation. Recently, a study found that tafamidis reduced all-cause mortality and cardiovascular-related hospitalizations and improved the quality of life of patients [10]. Adverse effects are considered relatively safe to administer because they are common, such as diarrhea, nausea, and headache. Based on these various reports, patients with HFpEF with LVH who have not been definitively diagnosed should be reconsidered for ATTR-CA, as tafamidis is the only oral medication effective against ATTR-CA, and cardioprotective medications, such as beta-blockers and renin-angiotensin-aldosterone system inhibitors, are ineffective. Additionally, tafamidis is a medication intended to suppress the progression of the disease; therefore, diagnosing ATTR-CA in the initial stages is necessary for early treatment. However, even if ATTR-CA is suspected promptly, tafamidis cannot be initiated unless tissue biopsy demonstrates amyloid deposition; if repeated tissue biopsies other than EMB cannot prove amyloid deposition, EMB with a high diagnostic probability should be considered. In contrast, EMB is highly invasive and not an easy test to perform. Therefore, evaluating the possibility of ATTR-CA and fully determining the indication of EMB by noninvasive examinations are necessary. If there is an indication for EMB, fully explaining its importance to the patients and obtaining consent are necessary. Increased awareness of ATTR-CA among non-cardiologists (including patients) may lead to early diagnosis and treatment. Although EMB helps diagnose ATTR-CA, it is often rejected because of concerns about its complications, such as ventricular perforation and ventricular conduction disturbances, as in this manuscript. Early EMB without delay is essential, based on the physician’s sufficient explanation of the need for EMB and the patient’s understanding, as delays in examination and the initiation of treatment can lead to disease progression.
Acknowledgments
None to declare.
Financial Disclosure
This manuscript was supported in part by Grabs-in-Acid (to S.K.) for scientific research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (19K084898).
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
The patient has consented to the submission of the case report to the journal.
Author Contributions
K.H. and S.K. contributed to the concept of this manuscript and the acquisition and evaluation of the data. K.H. drafted the manuscript. All authors provided critical revision of the manuscript and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ATTR-CA: transthyretin cardiac amyloidosis; 99mTc-PYP: 99mTc-labeled pyrophosphate; CMR: cardiac magnetic resonance; TTE: transthoracic echocardiography; EMB: endomyocardial biopsy; ECG: electrocardiogram; LVH: left ventricular hypertrophy; LVEF: left ventricular ejection fraction; BNP: brain natriuretic peptide; CKD: chronic kidney disease; HFpEF: heart failure with preserved ejection fraction; HHD: hypertensive heart disease; CA: cardiac amyloidosis; AL amyloidosis: acquired monoclonal immunoglobulin light chain amyloidosis; ATTRv: variant transthyretin amyloidosis; ATTRwt: wild-type transthyretin amyloidosis; TTR: transthyretin
| References | ▴Top |
- Dubrey SW, Falk RH. Amyloid heart disease. Br J Hosp Med (Lond). 2010;71(2):76-82.
doi pubmed - Bokhari S, Castano A, Pozniakoff T, Deslisle S, Latif F, Maurer MS. (99m)Tc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging. 2013;6(2):195-201.
doi pubmed pmc - Kitaoka H, Izumi C, Izumiya Y, Inomata T, Ueda M, Kubo T, Koyama J, et al. JCS 2020 Guideline on Diagnosis and Treatment of Cardiac Amyloidosis. Circ J. 2020;84(9):1610-1671.
doi pubmed - Marume K, Takashio S, Nishi M, Hirakawa K, Yamamoto M, Hanatani S, Oda S, et al. Combination of commonly examined parameters is a useful predictor of positive (99 m)Tc-Labeled pyrophosphate scintigraphy findings in elderly patients with suspected transthyretin cardiac amyloidosis. Circ J. 2019;83(8):1698-1708.
doi pubmed - Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation. 2005;112(13):2047-2060.
doi pubmed - Gonzalez-Lopez E, Gallego-Delgado M, Guzzo-Merello G, de Haro-Del Moral FJ, Cobo-Marcos M, Robles C, Bornstein B, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J. 2015;36(38):2585-2594.
doi pubmed - Gonzalez-Lopez E, Gagliardi C, Dominguez F, Quarta CC, de Haro-Del Moral FJ, Milandri A, Salas C, et al. Clinical characteristics of wild-type transthyretin cardiac amyloidosis: disproving myths. Eur Heart J. 2017;38(24):1895-1904.
doi pubmed - Sekijima Y, Yazaki M, Ueda M, Koike H, Yamada M, Ando Y. First nationwide survey on systemic wild-type ATTR amyloidosis in Japan. Amyloid. 2018;25(1):8-10.
doi pubmed - Sekijima Y, Ueda M, Koike H, Misawa S, Ishii T, Ando Y. Diagnosis and management of transthyretin familial amyloid polyneuropathy in Japan: red-flag symptom clusters and treatment algorithm. Orphanet J Rare Dis. 2018;13(1):6.
doi pubmed pmc - Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, Kristen AV, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379(11):1007-1016.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


