| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 5, May 2023, pages 255-261
Differences in Analgesia Methods for Open Gastrointestinal Surgery Are Not Associated With Initial Postoperative Ambulation
Yuta Mitobea, f, Takeshi Itoub, Yuri Yamaguchic, Tomomi Yoshiokad, Kenji Nakagawae
aGraduate School of Health and Welfare Science, International University of Health and Welfare, Tokyo, Japan
bDepartment of Anesthesia, St. Luke’s International Hospital, Tokyo, Japan
cDepartment of Nursing, Heisei Yokohama Hospital, Kanagawa, Japan
dDepartment of Nursing, Faculty of Health Science, Tokoha University, Shizuoka, Japan
eDepartment of Anesthesiology, International University of Health and Welfare, Mita Hospital, Tokyo, Japan
fCorresponding Author: Yuta Mitobe, Graduate School of Health and Welfare Science, International University of Health and Welfare, Tokyo, Japan
Manuscript submitted February 27, 2023, accepted May 4, 2023, published online May 31, 2023
Short title: Analgesia and Initial Postoperative Ambulation
doi: https://doi.org/10.14740/jocmr4899
| Abstract | ▴Top |
Background: A characteristic of modern medical care is the reduction in the length of hospital stay, and several facilities across Japan are working towards this goal. The presence of postoperative pain is correlated with the number of days to hospital discharge. Therefore, this study investigated the relationship between the analgesic methods used in clinical practice and the initial ambulation of postoperative laparotomy patients with severe postoperative worked incisional pain to enable better analgesic management in the future.
Methods: This retrospective study collected information from the medical records of 117 patients who underwent laparotomy between December 1, 2019, and October 13, 2020, at the Department of Gastroenterology of the International University of Health and Welfare Mita Hospital. Based on the failure or success of the ambulation process, the patients were divided into the delayed and successful groups, respectively.
Results: In the delayed group, patient-controlled epidural analgesia (PCEA) was used in 32 patients, intravenous patient-controlled analgesia (IV-PCA) was used in two patients, continuous worked incisional infiltration anesthesia was used in one patient, and transvenous acetaminophen was used in one patient for postoperative analgesia. In the successful group, PCEA was used in 66 patients, IV-PCA was used in 11 patients, continuous worked incisional infiltration anesthesia was used in three patients, and acetaminophen administered intravenously at patient’s request was used in one patient (P = 0.094).
Conclusions: No significant differences were observed between different postoperative analgesia methods, suggesting that there may be no association between postoperative ambulation and the postoperative analgesia method.
Keywords: Analgesia; Open gastrointestinal surgery; Initial postoperative ambulation
| Introduction | ▴Top |
Postoperative pain affects patients in various ways. The stress stimuli associated with pain stimulates the sympathetic nervous system, resulting in an increase in cardiac contractility, blood pressure, heart rate, and oxygen consumption in the myocardium. Excitation of the sympathetic nervous system also causes endocrine and metabolic effects, increased afterload, and disturbances in the coagulation/fibrinolytic system, could potentially cause cardiac failure and postoperative bleeding [1, 2]. The activation of sympathetic nerves by postoperative pain has various effects, including the suppression of gastrointestinal peristalsis and the promotion of antidiuretic hormone secretion. Postoperative pain also affects the sympathetic-adrenocortical system, and can result in renal damage, sleep disturbance, postoperative delirium, postoperative higher brain dysfunction [3], and suppression of the immune system [4] due to stress responses. In addition, postoperative pain is an unpleasant emotional experience for the patient. It hinders physical movement and delays bed release [5], impacting postoperative recovery [6, 7].
Intravenous patient-controlled analgesia (IV-PCA) is commonly used in Japan and involves the continuous transvenous administration of opioids using a patient-controlled analgesia (PCA) pump; additional doses can be administered by the patient when experiencing pain not relieved by continuous dose. However, opioids are associated with side effects such as drowsiness, nausea/vomiting, constipation, and respiratory depression.
In addition to IV-PCA, continuous epidural and patient-controlled epidural analgesia (PCEA), are also used for postoperative pain management in Japan. In PCEA, an epidural catheter is inserted such that local anesthetic alone or in combination with opioids is administered continuously through the catheter. Patients receiving PCEA should be off the bed while considering the onset of symptoms, such as hypotension, motor blockade, nausea/vomiting, and pruritus. Analgesia can be achieved with non-steroidal anti-inflammatory drugs (NSAIDs), or acetaminophen administered intravenously, orally, or rectally in the postoperative ambulation phase if IV-PCA or PCEA is not used.
With improvements in how we care for patients, the overall length of hospital stays has decreased. Many facilities in Japan are likewise working toward this goal. Postoperative analgesia is correlated with an early discharge from the hospital. According to previous studies, postoperative pain is more severe with open gastrectomy than with laparoscopic gastrectomy [7]. The superior quality of pain relief provided by epidural analgesia had a positive impact on out-of-bed mobilization, bowel function, and intake of food, with long-lasting effects on exercise capacity and health-related quality of life [8]. However, no studies have investigated the success or failure of analgesic methods and ambulation. Therefore, we aimed to investigate the relationship between analgesic methods used in clinical practice and the initial ambulation of postoperative patients after laparotomy and discuss the results to provide better analgesic management in the future.
| Materials and Methods | ▴Top |
Study design
This was a retrospective study in which information was collected from the medical records of patients who underwent laparotomy at the Department of Gastroenterology of the International University of Health and Welfare Mita Hospital between December 1, 2019, and October 13, 2020.
Study participants
Mita Hospital is certified as a designated cancer hospital. Our hospital is a medium-sized hospital with approximately 300 beds. Approximately 120 patients undergo laparotomy at the International University of Health and Welfare Mita Hospital per year. All patients who underwent gastrointestinal laparotomy were included in this study. A sample size of 128 cases was needed to perform a statistical analysis with a power of 0.8 using a t-test with an effect size of 0.5, a significance level of 0.05, and a power of 0.5 (the statistical analysis software EZR version 1.60). From the data collection period of this study, 149 cases were included. Patients with preoperative impairments in postural retention or ambulation, patients who were not allowed to be weaned by a physician, patients younger than 20 years or older than 80 years of age, patients who underwent surgery more than once during the study period, and patients who died during hospitalization were excluded from this study. Informed consent was obtained from all patients.
Survey items
The patient factors included age, preoperative activities of daily living (ADL), disease, surgical procedure, initial success or failure to wean the patient the day after the surgery, the number of days until the patient could walk independently after the surgery, intraoperative anesthesia method and drugs used, postoperative analgesia method, reason why the patient could not be weaned the day after the surgery, numerical rating scale (NRS) score, operative time, and the American Society of Anesthesiologists Physical Status (ASA-PS) score. The following data were collected from the results of the blood tests pre- and postoperatively: white blood cell (WBC) count, red blood cell (RBC) count, hemoglobin (Hb) content, hematocrit (Ht), and platelet (Plt) count. Data regarding the following parameters were collected from electronic medical records: total protein (TP), albumin (Alb), blood urea nitrogen (BUN), creatinine (Cre), estimated glomerular filtration rate (eGFR), aspartate aminotransferase (AST), alanine transaminase (ALT), γ-glutamyltransferase (γ-GT), C-reactive protein (CRP), prothrombin time activity (PT%), the international normalized ratio of prothrombin time (PT-INR), and activated partial thromboplastin time (APTT).
Analysis method
Data regarding the date patient first ambulated was collected from the electronic medical record, and the patients were divided into two groups for statistical comparison and examination. Patients who were ambulated within 1 day after the surgery were assigned to the successful group, and those who were ambulated on or after the second day after the surgery were assigned to the delayed group. Continuous variables are presented as mean or median, and Student’s t-test or Mann-Whitney U test was performed for comparison. Nominal and ordinal variables are presented as frequencies or proportions; they were compared using Fisher’s exact probability test. EZR was used for statistical analysis. Statistical significance was set at less than 5%. More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Ethical considerations
This study was conducted in compliance with the Declaration of Helsinki and the ethical guidelines for medical research involving human subjects.
When handling samples and information related to the implementation of the research, we assigned a number that was unrelated to the personal information of the research participants and gave sufficient consideration to the protection of the confidentiality of the research participants. This number was used for sending samples and information to the research secretariat and other related organizations, and sufficient care was taken to ensure that the personal information of the research participants was not dispersed outside the hospital. Information that could identify the research participants was not included when publishing the results of the research. The samples and information obtained in the research will not be used for any purpose other than that was stated in the purpose of the research. This research was conducted with the approval of the International University of Health and Welfare Research Ethics Review Committee (approval number: 20-Ig-35 September 28, 2020).
| Results | ▴Top |
Patient selection process
A total of 146 patients underwent laparotomy at the Department of Gastroenterology during the study period. Among the patients who met the inclusion criteria, one patient died during hospitalization, five patients were not allowed to wean by the physician, and 23 patients had missing data; thus, 29 patients were excluded. Ultimately, 117 patients were included in the analysis. Among these, 36 patients were assigned to the delayed group and 81 were assigned to the successful group for analysis. The patients were divided based on the early and late ambulation. The patients were assigned to the delayed group if they were unable to leave the bed and maintain the standing position on the day after the surgery, whereas they were assigned to the successful group if they were able to maintain the standing position. Figure 1 presents the analysis chart.
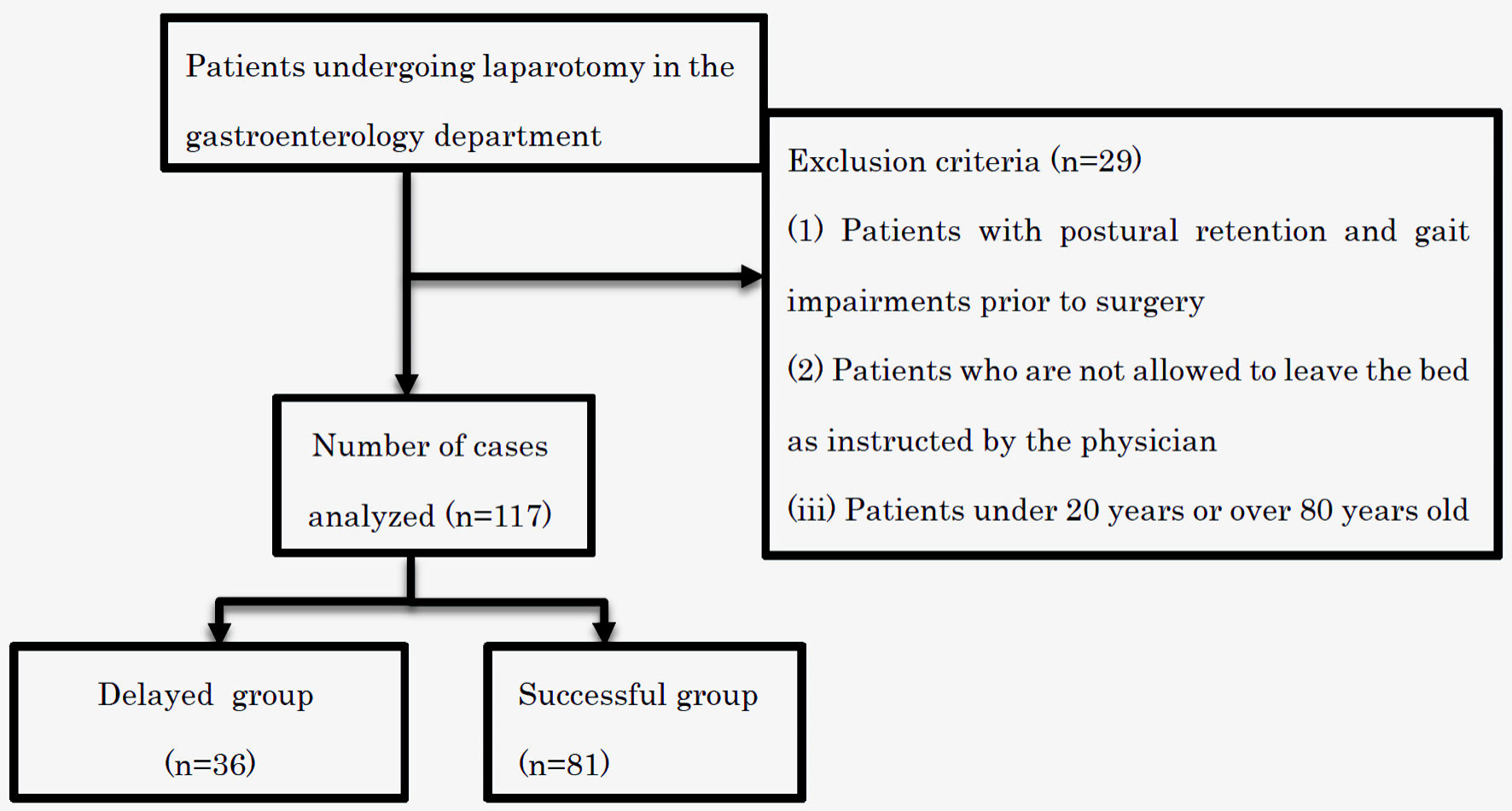 Click for large image | Figure 1. Flowchart of patient selection. |
Patient background
Table 1 presents the characteristics of patients. The mean age was 66.81 years in the delayed group and 65.62 years in the successful group (P = 0.624). No significant differences were found between the two groups. In the delayed group, 58.3% were male, and early ambulation group 59.3%.
 Click to view | Table 1. Patient Factors |
Comparison of the pre- and postoperative blood test data between the delayed and successful groups
Table 2 presents the data obtained from the blood test results. There was a significant increase in postoperative TP between the two groups (P = 0.03). WBC, RBC, Hb, Ht, Plt, Alb, BUN, Cre, eGFR, AST, ALT, γ-GT, CRP, PT, PT-INR, and APTT showed no significant increase.
 Click to view | Table 2. Blood Test Data |
Comparison of preoperative factors between the delayed and successful groups
A comparison of the preoperative factors is shown in Table 3. No significant increase was observed in the preoperative ASA-PS score (P = 0.61) or the preoperative patient gait status (P = 0.999).
 Click to view | Table 3. Preoperative Factors |
Comparison of intraoperative factors between the delayed and successful groups
A comparison of the intraoperative factors is presented in Table 4. We examined whether the type of intraoperative anesthesia is associated with early weaning. No significant increase was observed in the anesthesia method (P = 0.094) and operative time (P = 0.255).
 Click to view | Table 4. Intraoperative Factors |
Comparison of postoperative analgesia between the delayed and successful groups
A comparison of the postoperative analgesia methods is presented in Table 5. In the delayed group, PCEA was used in 32 patients, IV-PCA was used in two patients, continuous worked incisional infiltration anesthesia was used in one patient, and another method of postoperative analgesia was used in one patient. In the successful group, PCEA was used in 66 patients, IV-PCA was used in 11 patients, continuous worked incisional infiltration anesthesia was used in three patients, and acetaminophen administered intravenously on request was used in one patient (P = 0.534). No significant increase was observed.
 Click to view | Table 5. Postoperative Analgesia Methods |
Comparison of postoperative factors between the delayed and successful groups
A comparison of the postoperative factors is shown in Table 6. The mean number of days until the patients could walk independently was 6.64 days in the delayed group and 3.83 days in the successful group (P < 0.001), the mean duration of hospital stay was 39.36 days in the delayed group and 25.02 days in the successful group (P = 0.016), and the level of pain (NRS) was 4.25 in the delayed group and 2.48 in the successful group (P < 0.001). Significant differences were observed in all three parameters. The other parameters did not differ significantly between the groups.
 Click to view | Table 6. Postoperative Factors |
| Discussion | ▴Top |
Postoperative analgesia and ambulation
The American Society of Anesthesiologists has issued guidelines on postoperative analgesia, and the updated version recommends the following methods with recommendations and levels of evidence for each method: intravenous, intramuscular, subcutaneous, oral, or rectal administration of analgesics; timed or continuous intravenous or subcutaneous administration of analgesics; PCEA; IV-PCA with opioids; peripheral nerve block or infiltration anesthesia, and infiltration anesthesia. PCEA is effective for pain management during body movement unless there are contraindications, and IV-PCA are also recommended at level A. However, compared with IV-PCA, PCEA is less effective for the management of pain during body movement, and the side effects associated with opioids, such as somnolence, nausea, and vomiting, are more likely to occur. Administration of acetaminophen and NSAIDs is recommended at level A under certain conditions [9]. Among the 117 patients eligible for inclusion in this study, PCEA was the most commonly used method (98 patients), followed by IV-PCA (13 patients), continuous worked incisional infiltration anesthesia (four patients), and intravenous administration of anti-inflammatory analgesics, such as NSAIDs and acetaminophen, when requested by the patient (two patients). No significant differences were observed between the delayed and successful groups in this study, suggesting that the postoperative analgesic methods do not affect delayed or successful ambulation. Previous studies on the efficacy of postoperative analgesia have demonstrated the usefulness of PCEA and IV-PCA with regard to pain [9, 10]. In the present study, a possible association between postoperative analgesia and postoperative ambulation was also observed; however, no significant increase was observed in the delayed and successful groups based on the analgesia method. It cannot be stated that the postoperative analgesic method had no effect on the success or failure of initial postoperative ambulation in the present study. Postoperative pain is one of the most frequent complications of surgery [11], and it has a significant impact on the patient’s quality of life after surgery [12]. At the centers where the studies were conducted, pain was measured using NRS. The mean NRS was 4.25 in the delayed postoperative group and 2.48 in the successful group (P < 0.001). In a study by Carli et al on postoperative ambulation and its causes, postoperative pain was the most common cause of delayed ambulation [8]. In the present study, pain was the cause of delayed postoperative bed release in 14 patients, followed by hypotension (13 patients), nausea/vomiting (five patients), vertigo (two patients), and the patient’s refusal to leave the bed (one patient). The results of this study suggest that pain delays bed release and appropriate management of pain will greatly contribute to postoperative ambulation.
Limitations
In the current study, the patients were divided into two groups based on the success or failure of the ambulation process: the delayed and successful groups. However, it did not take into account information regarding the upper and lower gastrointestinal tracts, incision site and incision size, epidural catheter insertion position, and drug infusion rate. Therefore, in addition to the factors in the delayed group, further details regarding postoperative analgesia and the success or failure of postoperative ambulation by surgical site and incision site must be clarified.
Conclusions
This study analyzed each category and variable separately for the patients undergoing gastrointestinal laparotomy who were included in the successful and delayed groups and found no significant differences according to the postoperative analgesia method, suggesting that there may be no association between postoperative ambulation and postoperative analgesia method.
Acknowledgments
We would like to thank the International University of Health and Welfare, Mita Hospital.
Financial Disclosure
This work was supported by JSPS KAKENHI Grant (number: JP1919577).
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all patients.
Author Contributions
TI and YM designed and performed this study. TI drafted the manuscript and performed critical editing. TY and KN assisted and supported sample collection and subsequent statistical analysis. YY carefully supervised manuscript preparation and writing.
Data Availability
The authors declare that data supporting the findings of this study are available in the article.
Abbreviations
PCEA: patient-controlled epidural analgesia; IV-PCA: intravenous patient-controlled analgesia; PCA: patient-controlled analgesia; NSAIDs: non-steroidal anti-inflammatory drugs; ADL: activities of daily living; NRS: numerical rating scale; ASA-PS: American Society of Anesthesiologists Physical Status; WBC: white blood cell; RBC: red blood cells; Hb: hemoglobin; Ht: hematocrit; Pt: platelet; TP: total protein; Alb: albumin; BUN: blood urea nitrogen; Cre: creatinine; eGFR: estimated glomerular filtration rate; AST: aspartate aminotransferase; ALT: alanine transaminase; γ-GT: γ-glutamyltransferase; CRP: C-reactive protein; PT%: prothrombin time activity; PT-INR: international normalized ratio of prothrombin time; APTT: activated partial thromboplastin; ROC: receiver-operating characteristic
| References | ▴Top |
- Liu S, Carpenter RL, Neal JM. Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology. 1995;82(6):1474-1506.
doi pubmed - Wu CL, Fleisher LA. Outcomes research in regional anesthesia and analgesia. Anesth Analg. 2000;91(5):1232-1242.
doi pubmed - Silverstein JH, Timberger M, Reich DL, Uysal S. Central nervous system dysfunction after noncardiac surgery and anesthesia in the elderly. Anesthesiology. 2007;106(3):622-628.
doi pubmed - Ben-Eliyahu S, Page GG, Schleifer SJ. Stress, NK cells, and cancer: Still a promissory note. Brain Behav Immun. 2007;21(7):881-887.
doi pubmed - Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, Shimada M, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014;259(4):773-780.
doi pubmed - Zhang X, Yang J, Chen X, Du L, Li K, Zhou Y. Enhanced recovery after surgery on multiple clinical outcomes: Umbrella review of systematic reviews and meta-analyses. Medicine (Baltimore). 2020;99(29):e20983.
doi pubmed pmc - Chen Z, Xue H, Yuan H, Wang J, Wang Q, Zhang X. Complication rates in different gastrectomy techniques of enhanced recovery after surgery for gastric cancer: a meta-analysis. J Coll Physicians Surg Pak. 2022;32(10):1318-1325.
doi pubmed - Carli F, Mayo N, Klubien K, Schricker T, Trudel J, Belliveau P. Epidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery: results of a randomized trial. Anesthesiology. 2002;97(3):540-549.
doi pubmed - American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management. Anesthesiology. 2012;116(2):248-273.
doi pubmed - Mitra S, Carlyle D, Kodumudi G, Kodumudi V, Vadivelu N. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22(5):35.
doi pubmed - Fukawa Y, Kakuda W, Yoshida S, Zenta M, Itano O, Kiko R, Tani H, et al. Clinical impact of the introduction of an early rehabilitation protocol on infectious complications in patients after gastrointestinal cancer surgery. Prog Rehabil Med. 2019;4:20190005.
doi pubmed pmc - Ballantyne JC, Carr DB, deFerranti S, Suarez T, Lau J, Chalmers TC, Angelillo IF, et al. The comparative effects of postoperative analgesic therapies on pulmonary outcome: cumulative meta-analyses of randomized, controlled trials. Anesth Analg. 1998;86(3):598-612.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


