| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 15, Number 4, April 2023, pages 208-215
Predictors of Catheter-Related Bladder Discomfort After Surgery: A Literature Review
Yuta Mitobea, Tomomi Yoshiokab, h, Yasuko Babac, Yuri Yamaguchid, Kenji Nakagawae, Takeshi Itouf, Kiyoyasu Kurahashig
aGraduate School of Health and Welfare Science, International University of Health and Welfare, Tokyo, Japan
bDepartment of Nursing, Faculty of Health Science, Tokoha University, Shizuoka, Japan
cDepartment of Anesthesiology, International University of Health and Welfare, Mita Hospital, Tokyo, Japan
dDepartment of Anesthesiology, Yokohama City University Hospital, Kanagawa, Japan
eDepartment of Nursing, International University of Health and Welfare, Mita Hospital, Tokyo, Japan
fDepartment of Nursing, Capital Metropolitan Bokutoh Hospital, Tokyo, Japan
gDepartment of Anesthesiology and Intensive Care Medicine, International University of Health and Welfare Narita Hospital, Chiba, Japan
hCorresponding Author: Tomomi Yoshioka, Department of Nursing, Faculty of Health Science, Tokoha University, Shizuoka, Japan
Manuscript submitted January 27, 2023, accepted March 28, 2023, published online April 28, 2023
Short title: Review of Predictors of CRBD
doi: https://doi.org/10.14740/jocmr4873
| Abstract | ▴Top |
Background: Indwelling bladder catheters are routinely used in clinical practice. Patients may experience postoperative indwelling catheter-related bladder discomfort (CRBD). This study aimed to perform a literature review to identify predictors of postoperative CRBD.
Methods: We searched PubMed for relevant articles published between 2000 and 2020 using the search items “CRBD”, “catheter-related bladder discomfort”, and “prediction”. Additionally, we searched for articles that matched the research objectives from the references of the extracted articles. We included only prospective observational studies involving human participants and excluded interventional studies, observational studies that did not report sample sizes, or observational studies that did not research on predictors of CRBD. We narrowed our search to the keyword “prediction” and found five references. We selected five studies that met the objectives of the study as the target literature.
Results: Using the keywords “CRBD” and “catheter-related bladder discomfort”, we identified 69 published articles. The results were narrowed down by the keyword “prediction”, and five studies that recruited 1,147 patients remained. The predictors of CRBD can be divided into four factors: 1) patient factors; 2) surgical factors; 3) anesthesia factors; and 4) device and insertion technique factors.
Conclusion: Our study suggests that patients with predictors of CRBD should be closely monitored to reduce postoperative patient suffering, and their quality of life should be improved after anesthesia.
Keywords: Catheter-related bladder discomfort; Indwelling bladder catheters; Predictors; Perioperative; Postoperative
| Introduction | ▴Top |
Indwelling bladder catheters are routinely used in clinical practice. In the perioperative period, it is used to assess circulatory dynamics, maintain bed rest, and ensure urine drainage. Patients with perioperative indwelling bladder catheters may experience postoperative indwelling catheter-related bladder discomfort (CRBD), including pain and urinary urgency. These symptoms are often experienced after awakening from anesthesia and cause postoperative distress in patients. Patients may experience various types of discomfort other than pain immediately following surgery and anesthesia. A study reported that 43% of discomfort was related to an indwelling bladder catheter that had been inserted intraoperatively [1]. CRBD is unpleasant for patients after surgery, and it decreases patient satisfaction, causes postoperative complications, and significantly affects the patient’s recovery process. Indwelling bladder catheters are an important cause of postoperative agitation. Therefore, it is recommended that indwelling bladder catheters be removed as soon as possible [2]. Severe CRBD with behavioral responses, such as pulling out an indwelling bladder catheter, can also lead to urethral injury. Compared to a placebo drug, muscarinic antagonists, anesthetics, antiepileptics, and analgesics were reported to have greatly improved clinical symptoms and significantly reduced the incidence of CRBD [3]. Although CRBD has been studied extensively, because it is not a serious life-threatening complication, patients’ complaints of distress may not be properly addressed. A literature review has been published on interventions that may reduce the incidence and severity of CRBD; however, none has been published on predictors of CRBD. Therefore, the purpose of this study was to conduct a literature review of the predictors of CRBD and identify the predictors of CRBD. By preoperatively assessing the predictors of CRBD, appropriate interventions can be provided for patients at risk of CRBD.
| Research Methods | ▴Top |
Literature review methods
We searched PubMed for relevant articles published between 2000 and 2020 using search items.
Various algorithms, including the following terms: catheter-related bladder discomfort, risk factor, risk, and predictors were used. The results of the database search are summarized in ENDNOTE. Data from all selected studies were extracted and tabulated by one author and corroborated by another. Discrepancies were resolved by consensus by all authors. Information retrieved included the following: 1) author name and year of publication; 2) details of the study design (number of patients randomized, method of randomization, and duration of observation); 3) characteristics of the recruited patients; 4) details of interventions used (dosage and schedule); and 5) data on primary and secondary outcomes and P-values.
Definition of terms
CRBD is defined as urinary urgency and suprapubic discomfort [4, 5].
Rating scale for CRBD
CRBD was assessed using the four-point scale used by Agarwal et al [5] (Table 1).
 Click to view | Table 1. Rating Scale for Catether-Related Bladder Discomfort |
| Results | ▴Top |
Literature to be analyzed
Using the keywords “CRBD” and “catheter-related bladder discomfort”, we identified 69 published articles. The results were narrowed down by the keyword “prediction”, and five studies that recruited 1,147 patients remained (Fig. 1) (Table 2).
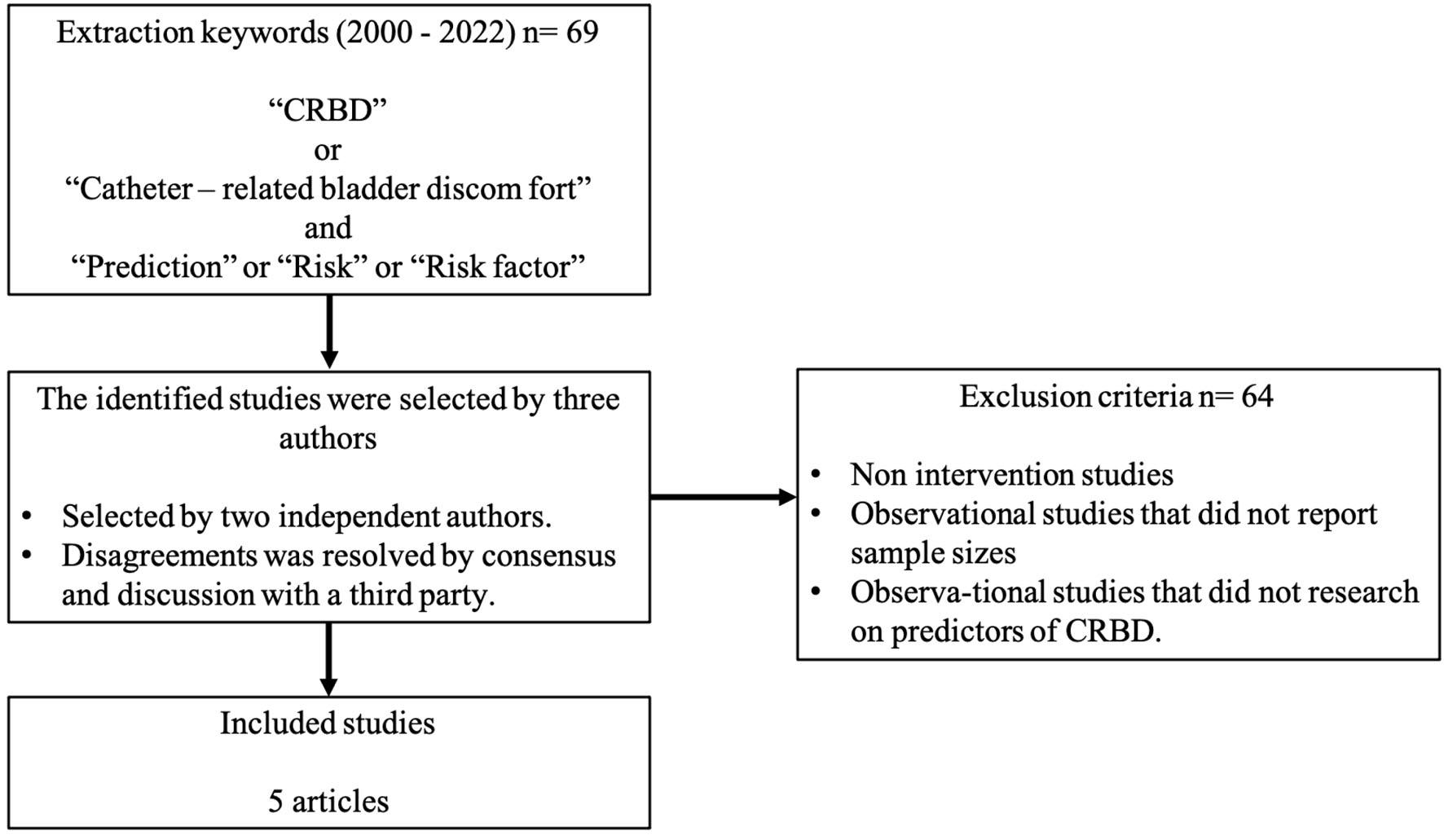 Click for large image | Figure 1. Flowchart of literature review. |
 Click to view | Table 2. Studies on Predictors of CRBD |
Incidence of CRBD
The incidence of CRBD in the five extracted studies ranged from 44.3% to 84.5% [4, 6-9]. The incidence of CRBD was the highest (84.5%) in a study that recruited patients who had undergone abdominal laparotomy in urological diseases [7] and the lowest (44.3%) in a study that recruited patients who had undergone obstetrical and gynecological surgery [4].
Predictors of CRBD
The predictors of CRBD that were extracted from the five studies are presented in Table 3.
 Click to view | Table 3. Predictors of Catether-Related Bladder Discomfort |
Patient factors
The following patient factors were extracted: male sex, age ≥ 50 years, age < 50 years, history of indwelling bladder catheters, and history of cesarean section.
Binhas et al classified postoperative patients into two groups: with and without CRBD. Male sex (odds ratio (OR) = 3.2; 95% confidence interval (95% CI), 1.0 - 10.5; P < 0.06) was a predictor of CRBD [6].
Lim et al classified postoperative patients into two groups: with a CRBD grade of 1 or less and those with a CRBD grade of 2 or more [4]. Male sex (OR = 7.07; 95% CI, 1.47 - 34.17; P = 0.015) and age < 50 years (OR = 4.79; 95% CI, 1.62 - 14.09; P = 0.005) were predictors of CRBD.
Li et al classified postoperative urological surgery patients into two groups: with and without CRBD [7]. History of indwelling bladder catheters (OR = 2.458; 95% CI, 1.1 - 5.9; P < 0.05) was a predictor of CRBD [7].
Li et al classified postoperative gynecological surgery patients into two groups: with a CRBD grade of ≥ 1 point (mild, moderate and severe) and those with a CRBD grade of ≥ 2 points (moderate and severe) [8]. Age ≥ 50 years (OR = 2.106; 95% CI, 1.2 - 3.8; P = 0.013) was a predictor of CRBD [8].
Moataz et al classified postoperative patients into two groups: with a first group (none and mild) and those with a second group (moderate and severe) [9]. Age < 50 years (OR = 0.4; 95% CI, 0.08 - 9.00; P = 0.006), history of indwelling bladder catheters (OR = 0.2; 95% CI, 0.04 - 1.30; P = 0.032), and history of cesarean section (OR = 0.3; 95% CI, 0.06 - 2.10; P = 0.005) were predictors of CRBD.
Surgical factors
The following surgical factors were extracted: abdominal laparotomy in urological diseases, uterus-related laparoscopic surgery, and obstetric and gynecological surgery.
Abdominal laparotomy in urological diseases was a predictor of CRBD in the studies by Li et al (OR = 3.074; 95% CI, 1.3 - 7.4; P < 0.05) [7] and Moataz et al [9] (OR = 0.5; 95% CI, 0.1 - 1.9; P = 0.02).
Uterus-related laparoscopic surgery (OR = 1.863; 95% CI, 1.1 - 3.1; P = 0.019) was reported to be a predictor of CRBD [8], and obstetrical and gynecological surgery (OR = 11.07; 95% CI, 1.06 - 115.70; P = 0.045) was a predictor of CRBD [4].
Anesthetic factors
Lack of postoperative analgesics (OR = 0.408; 95% CI, 0.2 - 0.9; P = 0.032) was a predictor of CRBD [8].
Device and insertion technique factors
The following device and insertion technique factors were extracted: a urinary catheter size of 18 ≥ Fr and lack of lubrication of a catheter.
The studies by Binhas et al [6] and Moataz et al [9] reported that a urinary catheter size of 18 ≥ Fr was a predictor of CRBD (OR = 2.2; 95% CI, 1.0 - 5.1; P = 0.06 and OR = 0.9; 95% CI, 0.08 - 1.1; P = 0.012, respectively). Moataz et al [9] further reported that lack of lubrication of a catheter (OR = 0.1; 95% CI, 0.05 - 1.1; P = 0.008) was a predictor of CRBD.
Overlap between each of the studies on CRBD
Four patient factors associated with CRBD had one or two items of overlap among the five studies. Three surgical factors associated with CRBD had one or two items of overlap among the five studies. One anesthetic factor associated with CRBD had one item of overlap among the five studies. Lack of lubrication of a catheter associated with CRBD had one or two items of overlap among the five studies (Table 4).
 Click to view | Table 4. Overlap Between Each of the Studies on CRBD |
| Discussion | ▴Top |
We conducted a literature review of five articles on the predictors of CRBD. The predictors of CRBD can be divided into four factors including patient factors, surgical factors, anesthetic factors, and device and insertion technique factors. By identifying the predictors of CRBD, unpleasant patient experiences and decreased patient satisfaction associated with CRBD can be reduced.
Incidence of CRBD
According to Bai et al [3], CRBD is frequent and occurs immediately after urological surgeries, especially after transurethral resection of the bladder tumor (TURBT). To date, TURBT is the most refractory surgical procedure among all urological surgical procedures because most patients who undergo TURBT are men and many have large indwelling bladder catheters (≥ 18 Fr) after the procedure. TURBT may increase the incidence of CRBD due to resection of the bladder wall and continued irritation of the bladder wall by reflux fluid.
Predictors of CRBD
Patient factors
The male sex was reported as a predictor of CRBD [4, 6] because anatomically, the male urethra is longer than the female urethra and is bent in an S-shape. This is because the indwelling bladder catheter stimulates a larger area of the urethra in men than in women, and the urethra is more strongly stimulated due to its S-shaped bend. In addition, men are more likely than women to complain of pain and use painkillers [10], indicating a lower pain tolerance. Male patients were more dissatisfied than their female counterparts with transurethral catheterization (satisfaction score: 4.18/10 vs. 2.75/10; P = 0.05) [11].
The controversies surround age factor of CRBD. Age ≥ 50 years and < 50 years were reported as predictors of CRBD [4, 8, 9]. Gynecological surgery studies have reported that an age of ≥ 50 years is a predictor of CRBD [8]. In gynecological surgery, the older the patient, the higher the possibility of that patient undergoing hysterectomy due to malignancy, and since hysterectomy, which irritates the bladder, is performed for patients ≥ 50 years, an age of ≥ 50 years is a predictor of CRBD. As we age, our pain threshold increases [12], we become more insensitive to pain stimuli, and we are less likely to complain of CRBD. In a study of female patients, higher pain scores with indwelling bladder catheters were recorded for younger women, which could be explain by better urethral sphincter muscle tone compared to that of older women [13]. Different studies have reported different results [4, 8, 9], and further research is needed.
History of indwelling bladder catheters was reported as a predictor of CRBD [7, 9]. Emotional distress and anxiety have been shown to be associated with severe acute pain [14]. Patients’ past experience with placement of a retained catheter might psychologically mitigate the fear of urinary catheters, thereby lowering the incidence of CRBD [7]. Preoperative education can effectively reduce anxiety regarding catheterization [15], and preoperative education on CRBD using illustrations, which is simple and inexpensive, is effective in reducing both the incidence and severity of CRBD [16].
History of cesarean section was a predictor of CRBD [9]. Compared with patients with a history of vaginal delivery, patients with a history of cesarean section were significantly more likely to develop CRBD. To date, no study has established an association between CRBD and the method of delivery.
Surgical factors
Obstetrical and gynecological surgery and, specifically, uterus-related laparoscopic surgery were reported as predictors of CRBD [4, 8]. This is because uterine contraction or irritation during laparoscopic surgery may irritate the bladder. Furthermore, postoperative neuropathy can induce bladder paralysis.
Anesthetic factors
Lack of postoperative analgesics was reported as a predictor of CRBD [8]. Inadequate postoperative analgesia increases incidence of CRBD. CRBD is similar to overactive bladder and is caused by involuntary contraction of the bladder smooth muscle due to muscarinic receptor stimulation. There are five subtypes of muscarinic receptors, M1 to M5. Bladder smooth muscle assembles M2 (70-80%) and M3 (20-30%) receptors, and M3 receptors are responsible for the contraction of bladder smooth muscle [17]. Therefore, muscarinic receptor antagonists such as tolterodine, oxybutynin, and butyl scopolamine are effective in preventing CRBD [4]. Tramadol and ketamine are centrally acting opioid analgesics with antimuscarinic effects that effectively prevent CRBD when administered intravenously [3]. Intravenous paracetamol has been shown to be effective in the prevention of CRBD [18]. The mechanism of CRBD is related to prostaglandin E2 (PGE2) in urine. PGE2 is produced in the bladder and acts on bladder smooth muscle contraction. Stimulation of bladder smooth muscles by indwelling bladder catheters promotes PGE2 synthesis and induces contraction of the bladder smooth muscles, resulting in CRBD. Paracetamol, an inhibitor of PG synthesis and cyclooxygenase-2, reduces the incidence and symptoms of CRBD [3].
In a study that compared the effects of sevoflurane and desflurane inhalant anesthetics on CRBD, sevoflurane, when compared with desflurane, reduced the incidence of CRBD in patients who underwent TURBT. CRBD in the first 24 h postoperatively occurred in 34/45 (76%) patients receiving sevoflurane compared to 41/44 (93%) patients receiving desflurane [19]. In another study that compared the effects of sevoflurane and propofol on CRBD, CRBD in the first 1 h postoperatively was lower in the sevoflurane group than in the propofol group (59% vs. 85%; P = 0.007) [20]. This is thought to be due to the ability of sevoflurane to block M3 receptors, which cause CRBD [21].
A study examining the effects of magnesium’s smooth muscle relaxant effects on CRBD reported that magnesium reduced the incidence of CRBD grade of ≥ 2 points (above a moderate grade) and increased patient satisfaction after TURBT [22].
To prevent CRBD, intraoperative and postoperative pain management are important. Each drug has complications, such as anticholinergic effects, sedation, nausea and vomiting, and respiratory depression; however, multimodal pain management can reduce the incidence of these complications.
Device and insertion technique factors
A urinary catheter size of 18 ≥ Fr was reported as a predictor of CRBD [6, 9]. The incidence of CRBD is less in nonurological postoperative patients with indwelling bladder catheters of 12 - 14 Fr [23]. Reducing the size of the indwelling bladder catheter reduces mechanical irritation to the urethra, leading to a reduction in the CRBD.
Lack of lubrication of a catheter was reported as a predictor of CRBD [9]. If an indwelling bladder catheter is inserted without lubrication, the urethral mucosa is damaged by friction during insertion [13]. When lubricants containing local anesthetics are used, they can reduce trauma to the urethra and minimize pain and discomfort. Local anesthetics, such as lidocaine or prilocaine cream injected into the urethra or applied to the catheter as a lubricant, have been shown to reduce the incidence and severity of CRBD [24]. In addition, indwelling bladder catheters coated with analgesics are effective in preventing CRBD [25], and some indwelling bladder catheters for men are made such that they can be used to inject a local anesthetic into the urethra, which provides surface anesthesia for the urethral mucosa [26].
The balloon volume of an indwelling bladder catheter affects the occurrence of CRBD. In a study of patients who underwent urological surgery, a 50% reduction in the balloon volume of the indwelling bladder catheter reduced CRBD incidence [27]. The pain was mostly reported when the balloon of the urinary catheter contacts the bladder triangle or when the balloon volume of the indwelling bladder catheter is too large. Balloon catheters of 5 - 10 mL should be selected [28]. Reducing the balloon volume reduces the stimulation of the bladder induced by the balloon, thereby reducing the symptoms of CRBD. A comparison of the effects of indwelling bladder catheter insertion and suprapubic bladder drainage on CRBD after robot-assisted laparoscopic radical prostatectomy showed a decrease in postoperative CRBD in patients who underwent suprapubic bladder drainage [29]. The use of appropriate devices and insertion methods can help to reduce the incidence of CRBD.
Limitations
In this study, a literature review was conducted to identify patient factors associated with the occurrence of CRBDs: surgical factors, anesthetic factors, device and insertion technique factors and patient-related factors. However, these factors were not independent of each other, but combined to cause CRBD. However, it was not clear how many of these factors combined to cause CRBD and whether the combination of factors affected the severity and duration of CRBD. In addition, it was not clear if patient factors were responsible for causing POST or if they affected severity and duration. The current review found no reports related to CRBD or patient factors. Therefore, further research on CRBD and patient factors is warranted. There were few studies on CRBD, and thus only 1 - 2 studies overlapped items for each factor. Therefore, a meta-analysis could not be performed.
| Conclusion | ▴Top |
Predictors of CRBD included: 1) patient factors (male sex, age ≥ 50 years, age < 50 years, history of indwelling bladder catheters, and history of cesarean section); 2) surgical factors (abdominal laparotomy in urological diseases, uterus-related laparoscopic surgery, and obstetrical and gynecological surgery); 3) anesthetic factors (lack of postoperative analgesics); and 4) device and insertion technique factors (a urinary catheter size of ≥ 18 Fr, lack of lubrication of a catheter, and urinary catheter-related pain (UCRP) ≥ 4).
Our study suggests that patients with predictors of CRBD should be closely monitored to reduce postoperative patient suffering, and their quality of life should be improved after anesthesia.
Acknowledgments
None to declare.
Financial Disclosure
This work was supported by JSPS KAKENHI grant (number: 21K21204).
Conflict of Interest
The authors declare no conflict of interest.
Author Contributions
TY designed the study. KN, TI, and YY participated in data acquisition, extraction, and analysis, and drafted the final work. KK, YM and YB supervised this manuscript’s preparation and writing. The authors reviewed the final version of the manuscript and approved it for publication.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
CRBD: catheter-related bladder discomfort; UCRP: urinary catheter-related pain; TURBT: transurethral resection of the bladder tumor; PG: prostaglandin
| References | ▴Top |
- Zegerman A, Ezri T, Weinbroum AA. Postoperative discomfort (other than pain) - a neglected feature of postanesthesia patient care. J Clin Monit Comput. 2008;22(4):279-284.
doi pubmed - Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010;57(9):843-848.
doi pubmed - Bai Y, Wang X, Li X, Pu C, Yuan H, Tang Y, Li J, et al. Management of catheter-related bladder discomfort in patients who underwent elective surgery. J Endourol. 2015;29(6):640-649.
doi pubmed pmc - Lim N, Yoon H. Factors predicting catheter-related bladder discomfort in surgical patients. J Perianesth Nurs. 2017;32(5):400-408.
doi pubmed - Agarwal A, Raza M, Singhal V, Dhiraaj S, Kapoor R, Srivastava A, Gupta D, et al. The efficacy of tolterodine for prevention of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Anesth Analg. 2005;101(4):1065-1067.
doi pubmed - Binhas M, Motamed C, Hawajri N, Yiou R, Marty J. Predictors of catheter-related bladder discomfort in the post-anaesthesia care unit. Ann Fr Anesth Reanim. 2011;30(2):122-125.
doi pubmed - Li C, Liu Z, Yang F. Predictors of catheter-related bladder discomfort after urological surgery. J Huazhong Univ Sci Technolog Med Sci. 2014;34(4):559-562.
doi pubmed - Li SY, Song LP, Ma YS, Lin XM. Predictors of catheter-related bladder discomfort after gynaecological surgery. BMC Anesthesiol. 2020;20(1):97.
doi pubmed pmc - Moataz A, Chadli A, Wichou E, Gallouo M, Jandou I, Saber S, Serhier Z, et al. [Predictors of catheter-related bladder discomfort]. Prog Urol. 2020;30(16):1045-1050.
doi pubmed - Tsui SL, Tong WN, Irwin M, Ng KF, Lo JR, Chan WS, Yang J. The efficacy, applicability and side-effects of postoperative intravenous patient-controlled morphine analgesia: an audit of 1233 Chinese patients. Anaesth Intensive Care. 1996;24(6):658-664.
doi pubmed - Tan GW, Chan SP, Ho CK. Is transurethral catheterisation the ideal method of bladder drainage? A survey of patient satisfaction with indwelling transurethral urinary catheters. Asian J Surg. 2010;33(1):31-36.
doi pubmed - Riley JL, 3rd, Cruz-Almeida Y, Glover TL, King CD, Goodin BR, Sibille KT, Bartley EJ, et al. Age and race effects on pain sensitivity and modulation among middle-aged and older adults. J Pain. 2014;15(3):272-282.
doi pubmed pmc - Chan MF, Tan HY, Lian X, Ng LY, Ang LL, Lim LH, Ng WM, et al. A randomized controlled study to compare the 2% lignocaine and aqueous lubricating gels for female urethral catheterization. Pain Pract. 2014;14(2):140-145.
doi pubmed - Katz J, Poleshuck EL, Andrus CH, Hogan LA, Jung BF, Kulick DI, Dworkin RH. Risk factors for acute pain and its persistence following breast cancer surgery. Pain. 2005;119(1-3):16-25.
doi pubmed - Ramesh C, Nayak BS, Pai VB, Patil NT, George A, George LS, Devi ES. Effect of Preoperative Education on Postoperative Outcomes Among Patients Undergoing Cardiac Surgery: A Systematic Review and Meta-Analysis. J Perianesth Nurs. 2017;32(6):518-529.e512.
doi pubmed - Zhou L, Zhou L, Tian L, Zhu D, Chen Z, Zheng C, Zhou T, et al. Preoperative education with image illustrations enhances the effect of tetracaine mucilage in alleviating postoperative catheter-related bladder discomfort: a prospective, randomized, controlled study. BMC Anesthesiol. 2018;18(1):204.
doi pubmed pmc - Yamanishi T, Chapple CR, Chess-Williams R. Which muscarinic receptor is important in the bladder? World J Urol. 2001;19(5):299-306.
doi pubmed - Ergenoglu P, Akin S, Yalcin Cok O, Eker E, Kuzgunbay B, Turunc T, Aribogan A. Effect of intraoperative paracetamol on catheter-related bladder discomfort: a prospective, randomized, double-blind study. Curr Ther Res Clin Exp. 2012;73(6):186-194.
doi pubmed pmc - Kim HC, Hong WP, Lim YJ, Park HP. The effect of sevoflurane versus desflurane on postoperative catheter-related bladder discomfort in patients undergoing transurethral excision of a bladder tumour: a randomized controlled trial. Can J Anaesth. 2016;63(5):596-602.
doi pubmed - Kim HC, Park HP, Lee J, Jeong MH, Lee KH. Sevoflurane vs. propofol in post-operative catheter-related bladder discomfort: a prospective randomized study. Acta Anaesthesiol Scand. 2017;61(7):773-780.
doi pubmed - Nakayama T, Penheiter AR, Penheiter SG, Chini EN, Thompson M, Warner DO, Jones KA. Differential effects of volatile anesthetics on M3 muscarinic receptor coupling to the Galphaq heterotrimeric G protein. Anesthesiology. 2006;105(2):313-324.
doi pubmed - Park JY, Hong JH, Kim DH, Yu J, Hwang JH, Kim YK. Magnesium and bladder discomfort after transurethral resection of bladder tumor: a randomized, double-blind, placebo-controlled study. Anesthesiology. 2020;133(1):64-77.
doi pubmed - Bach H, Kaasby K, Sorensen A, Lofqvist S, Laursen BS. Incidence and severity of catheter-related bladder discomfort among nonurological adult patients in a postanesthesia care unit. J Perianesth Nurs. 2020;35(1):29-33
- Mu L, Geng LC, Xu H, Luo M, Geng JM, Li L. Lidocaine-prilocaine cream reduces catheter-related bladder discomfort in male patients during the general anesthesia recovery period: A prospective, randomized, case-control STROBE study. Medicine (Baltimore). 2017;96(14):e6494.
doi pubmed pmc - Sun JL, Lu YP, Huang B, Tu HL, Zhou XY, Chen QM, Guo SM, et al. [Effect of a novel analgesic disposable urinary catheter in prevention of restlessness caused by catheter-related bladder discomfort in general anesthesia patients in recovery period]. Zhonghua Yi Xue Za Zhi. 2008;88(25):1750-1752.
pubmed - Imai H, Seino Y, Baba H. Efficacy of a novel urinary catheter for men with a local anesthetic injection port for catheter-related bladder discomfort: a randomized controlled study. J Anesth. 2020;34(5):688-693.
doi pubmed - Zugail AS, Pinar U, Irani J. Evaluation of pain and catheter-related bladder discomfort relative to balloon volumes of indwelling urinary catheters: A prospective study. Investig Clin Urol. 2019;60(1):35-39.
doi pubmed pmc - Wilson M. Causes and management of indwelling urinary catheter-related pain. Br J Nurs. 2008;17(4):232-239.
doi pubmed - Krane LS, Bhandari M, Peabody JO, Menon M. Impact of percutaneous suprapubic tube drainage on patient discomfort after radical prostatectomy. Eur Urol. 2009;56(2):325-330.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


