| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 2, February 2023, pages 109-115
Positive Correlation Between Changes in Serum Albumin Levels and Breakfast Non-Protein Calorie/Nitrogen Ratio in Geriatric Patients
Yasuko Fukudaa, b, e, Mikako Ochic, Ryouko Kanazawaa, Hiromu Nakajimad, Keisuke Fukuoa, b, Masanobu Nakaic
aDepartment of Food Science and Nutrition, School of Human Environmental Science, Mukogawa Women’s University, Ikebiraki-cho, Nishinomiya, Hyogo 663-8558, Japan
bResearch Institute for Nutrition Science, Mukogawa Women’s University, Ikebiraki-cho, Nishinomiya, Hyogo 663-8558, Japan
cNakai Hospital, Nada-ku, Kobe, Hyogo 657-0833, Japan
dDepartment of Endocrinology and Metabolism/Clinical Laboratory, Osaka International Cancer Institute, Chuo-ku, Osaka, Osaka 541-8567, Japan
eCorresponding Author: Yasuko Fukuda, Department of Food Science and Nutrition, School of Human Environmental Science, Mukogawa Women’s University, Hyogo 663-8558, Japan
Manuscript submitted November 28, 2022, accepted January 27, 2023, published online February 28, 2023
Short title: Serum Albumin and NPC/N in Geriatric Patients
doi: https://doi.org/10.14740/jocmr4848
| Abstract | ▴Top |
Background: Differences in nutrition intake by meal intake time of geriatric patients may affect albumin (Alb) synthesis ability.
Methods: We included 36 geriatric patients (81.7 ± 7.7 years; 20 males and 16 females) as subjects. We calculated their dietary patterns (DPs) by computing intake by breakfast, lunch, and dinner, as well as by nutrient, for a weight of 1 kg/day for 4 weeks after hospitalization. We confirmed the relationship between “DP with a positive correlation with breakfast protein” and the change rate of albumin (Alb-RC). Then, we performed linear regression analysis to explore factors influencing Alb-RC and compared non-protein calorie/nitrogen ratio (NPC/N) between the upper and lower Alb-RC groups.
Results: It was observed that Alb-RC was negatively correlated with “DP with a positive correlation with breakfast protein” (B = -0.055, P = 0.038) and positively correlated with breakfast NPC/N (B = 0.043, P = 0.029). Breakfast NPC/N tended to be higher in the upper group than in the lower group (P = 0.058).
Conclusion: The study revealed that there was a positive correlation between Alb-RC levels and breakfast NPC/N in geriatric patients at the care mix institution.
Keywords: Albumin; Energy intake; Hospitalization; Nutrients; Regression analysis
| Introduction | ▴Top |
Serum albumin (Alb) level is widely used as an index to assess nutritional status [1-4]. To increase the intake of good protein or advantageously induce body protein synthesis, non-protein calorie/nitrogen ratio (NPC/N), which is the balance between energy and protein, is considered. NPC/N is an index demonstrating the amount of carbohydrate and lipid that should be consumed so that the consumed protein can be effectively utilized [5].
At small-scale, community-based hospitals providing care-mix medical care, geriatric patients who have completed acute treatment are continuously provided care. Hospital food is provided in controlled quantities and preparations, taking into account patients’ medical conditions as well as their masticatory and swallowing abilities. However, dietary intake may differ depending on patients’ appetites and preferences, and NPC/N may vary; therefore, it is necessary to clarify which type of meal should be consumed at which time of the day to provide nutritional support.
We have previously reported that the differences in intake by breakfast, lunch, and dinner, as well as by nutrient calculated from the nutrition of hospital food consumed by geriatric patients, may affect the Alb synthesis ability in the liver [6]. In addition, we have clarified that NPC/N in nutrition intake affects the selection of discharge destination [7].
In this study, we report the relationship between changes in Alb at discharge and admission, as well as NPC/N in nutrition intake that we examined.
| Materials and Methods | ▴Top |
Subjects
The target hospital was a small-scale (48-bed) hospital providing care-mix medical care in Nada Ward, Kobe, Hyogo.
The subjects were 36 geriatric patients (81.7 ± 7.7 years; 20 males and 16 females) admitted to the target hospital between January 1, 2017 and December 31, 2020, suffering from chronic diseases, receiving only oral nutritional support, and whose meal intake information 1 month after hospitalization as well as blood test findings at admission and discharge were available. All of the subjects had chronic diseases such as diabetes and hypertension, but they were treated in an acute hospital and their medical conditions were stable at the time of this study.
No double-counting transpired. However, we excluded those who had severe restrictions on protein intake (≤ 45 g/ day).
Methods
We conducted a retrospective medical-record review study. The survey items were as follows: basic attributes at admission, comorbidities, Barthel index, the length of hospitalization, the type of hospital food, blood biochemical data at admission and discharge, and the amount of leftovers from staple food and side dish of breakfast, lunch, and dinner for 4 weeks after admission.
We calculated the body mass index using height and weight and assigned a score to the comorbidities according to the Carlson comorbidity index [8].
Duration of hospitalization was the number of days from admission to discharge.
Alb level at discharge was divided by Alb level at admission to obtain the Alb rate of change (Alb-RC). Next, multivariate analysis was performed.
Dietary patterns (DPs) were extracted using principal component analysis. Energy intake (kcal/body weight (BW) kg/day), protein intake (g/BW kg/day), and non-protein energy intake (kcal/BW kg/day) obtained from breakfast, lunch, and dinner were calculated from dietary intake, and these nine variables were used.
When calculating the nine variables, we calculated each nutrition intake for 4 weeks after hospitalization and the mean intake by nutrient per day based on the survey results of the amount of leftover food by staple food and side dish of each individual subject as well as the nutrient described in the menu table. There were several types of hospital food available, including the normal diet, whole porridge diet, diabetic diet, dyslipidemia diet, liver diet, heart/hypertensive diet, and kidney disease diet.
In addition, NPC/N was calculated by (energy(kcal) - protein(g) × 4(kcal))/(protein/6.25), standardized, and used.
Furthermore, Alb-RC was arranged in ascending order, and NPC/N by breakfast, lunch, and dinner were compared between the lower 12 subjects (lower group) and upper 12 subjects (upper group).
Ethical considerations
This study was approved by the Research Ethics Committee of Mukogawa Women’s University and Junior College on March 15, 2019 (approval No. 18-85), and was conducted according to the principles of the Declaration of Helsinki. We obtained the subjects’ informed consent, with the assurance that they would remain anonymous and could withdraw from the study anytime.
Statistical analysis
Factor loading for the food groups representing the principal components was set at ≥ 0.50, and three principal components were extracted.
Next, two multiple regression analyses were performed. In model 1, with Alb-RC as the objective variable, gender and the three principal components were input as the explanatory variables. In model 2 (stepwise method), with Alb-RC as the objective variable, gender, breakfast energy intake, protein intake, and NPC/N were input as the explanatory variables.
Statistical Analysis System (SAS) version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for analysis, and the criterion for statistical significance was less than 5%.
| Results | ▴Top |
Subjects’ demographics
As shown in Table 1, the most common reasons for admission were chronic heart failure, bronchial pneumonia, chronic obstructive pulmonary disease, and type 2 diabetes; however, these conditions had been treated in the acute care hospital, and thus, there were no clinical issues requiring active intervention (Table 1).
 Click to view | Table 1. Demographics (n = 36) |
There was no difference between Alb at admission and discharge, and mean Alb-RC was 0.98 ± 0.13 (Table 1, Fig. 1).
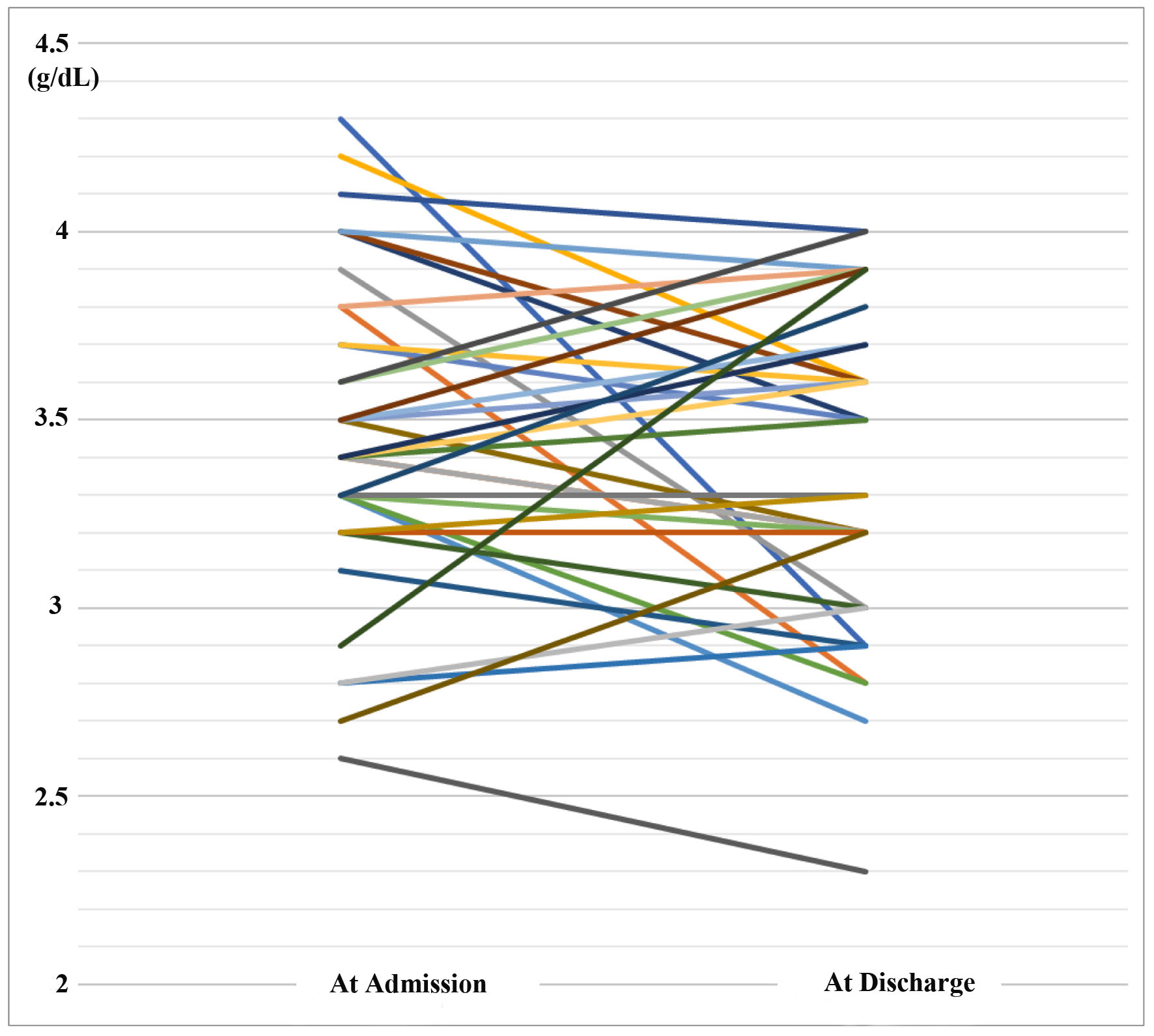 Click for large image | Figure 1. Changes in serum albumin levels at admission and discharge. |
Mean energy intake was 29.8 ± 6.5 kcal/BW kg/day, mean protein intake was 1.17 ± 0.28 kg/BW kg/day, and there was no excessive or insufficient nutrition intake, as instructed by attending physicians (Table 1).
Daily mean NPC/N was 136 ± 22, breakfast NPC/N was 167 ± 37, lunch NPC/N was 140 ± 30, and dinner NPC/N was 130 ± 30 (Table 1).
Multivariate analysis results
Principal component analysis
The first principal component was “DP without characterized factors”, and its contribution rate was 79.0%. The second principal component was “DP characterized by a positive correlation with breakfast energy (0.551) and non-protein energy intake (0.607)”, and its contribution rate was 9.8%. The third principal component was “DP characterized by a positive correlation with breakfast protein (0.760)”, and its contribution rate was 7.3%. The cumulative contribution rate of the three principal components was 96.1% (Table 2).
 Click to view | Table 2. Dietary Pattern (n = 36) |
Multiple regression analysis
1) Model 1
The third principal component was a significant negative determinant factor for Alb-RC (B = -0.055, P = 0.038, Table 3).
 Click to view | Table 3. Examination of Factors for Change Rate of Albumin (n = 36) |
2) Model 2
Breakfast NPC/N was a significant positive determinant factor for Alb-RC (B = 0.043, P = 0.029, Table 3).
Comparison of Alb-RC between the two groups: upper group vs. lower group
Alb-RC was 1.11 ± 0.09 for the upper group and 0.85 ± 0.08 for the lower group, and there was a significant difference (P < 0.001). Breakfast NPC/N was 0.54 ± 1.23 for the upper group and -0.35 ± 0.91 for the lower group, and it was higher in the upper group than in the lower group (P = 0.058), but no difference was observed in lunch and dinner NPC/N. A choice of bread or porridge was given for breakfast, and individuals choosing porridge tended to be more in the upper group than in the lower group (P = 0.069, Table 4).
 Click to view | Table 4. Comparison Between the Upper Group and the Lower Group of Change Rate of Albumin (n = 24) |
| Discussion | ▴Top |
This study aimed to explore nutritional factors affecting changes in Alb at discharge and admission in geriatric patients admitted to a local small-scale hospital providing care-mix medical care.
Regarding the methods, the nine variables of energy intake (kcal/BW kg/day), protein intake (g/BW kg/day), and non-protein energy intake (kcal/BW kg/day) collected from the hospital food intake status survey of each individual patient were calculated by breakfast, lunch, and dinner, as well as by nutrient, and three DPs were calculated using principal component analysis method. Next, linear regression analysis was performed with Alb-RC as the objective variable and gender and three principal components as the explanatory variables. The result showed that the third principal component was negatively correlated. The third principal component had “a positive correlation with breakfast protein intake”. By focusing on NPC/N, linear regression analysis (stepwise method) was performed with Alb-RC as the objective variable and gender, breakfast energy intake (kcal/BW kg/day), protein intake (g/BW kg/day), and NPC/N as the explanatory variables. Breakfast NPC/N was positively correlated with Alb-RC. Furthermore, to verify the validity of breakfast NPC/N, the upper and lower Alb-RC groups were compared. Breakfast NPC/N tended to be higher in the upper group than in the lower group. NPC/N indicates the ratio of non-protein energy intake (energy from carbohydrates and lipids) per gram of nitrogen contained in protein [6]. Therefore, higher amounts of energy were derived from carbohydrates and lipids in the upper Alb-RC group.
NPC/N is an index that determines whether administered amino acids are effectively synthesized into proteins [6]. It is also an index applicable to hospital food ingested orally. In this study, NPC/N might be dispersed due to the bias in the intake of staple food and side dishes of each individual patient or the difference in staple food selection. Initially, hospital food is managed by nutrition and NPC/N contributing to improvement based on medical conditions. However, when dietary intake differs depending on patients’ appetites and preferences, NPC/N may vary. Among them, at the target hospital, the side dish for breakfast is fixed, such as vegetable dishes, fruits, and milk, but the staple food is either bread or porridge. As protein and carbohydrate levels differ in bread and porridge, breakfast NPC/N varies depending on which of them is chosen. NPC/N is higher with porridge than with bread. Breakfast contents were confirmed between the upper and lower groups, and it was found that individuals choosing porridge tended to be more in the upper Alb-RC group (six out of 12 subjects) than in the lower group (one out of 12 subjects) (P = 0.069). Based on these observations, it was thought that an enough amount of non-protein energy may be necessary at breakfast. In other words, to improve Alb metabolism, it might be useful to increase the ratio of carbohydrates as much as possible and to increase non-protein energy intake at breakfast after taking required nutrition into account. In addition, there was no difference in lunch and dinner NPC/N. This is because, in principle, there was no choice for the staple food of lunch and dinner, which was unified as rice or porridge.
Chrononutrition has shown that the regulation of the body clock, which forms a rhythm of approximately 24 h a day, is important for maintaining health [9, 10]. Light is the most crucial factor in resetting (synchronizing) the subtle deviation in the biological clock among cells, but eating is a stronger factor than light [11]. Breakfast normalizes the liver clock, but late-night supper disrupts the liver clock. When the same high-carbohydrate food is consumed at breakfast and dinner, differences have been shown in pathways related to glycolysis and the tricarboxylic acid (TCA) cycle, which are close to glucose metabolism [12-14].
Furthermore, it has been elucidated by animal experiments that the metabolism of nutrients changes as per time zone [15-17]. In addition, the metabolic dynamics in the blood during breakfast and dinner were comprehensively compared using human metabolome. The results showed that the metabolic activities of the energy generation system and biocomponent synthesis system are enhanced during breakfast than dinner by focusing on glycolysis, TCA cycle, and amino acid metabolism [18]. From the perspective of chrononutrition, it is important to prioritize and consume food ingredients that move the body clock in the morning, and carbohydrates are useful for promoting the metabolism of sugar that is easily expended in the morning.
Alb is a protein produced only in the liver. It is used as one of the indices to assess disease severity and the quality of nutritional status [19-24]. The liver has a large reserve capacity and is resistant to aging. However, it is a well-known fact that, with aging, liver weight and volume decrease, hepatocytes count and blood flow decrease, and its metabolic function declines. Therefore, glucose tolerance deteriorates with age, and protein and lipid metabolism are also impacted considerably [25-27].
On the other hand, liver glycogen is essential for the liver to maintain its metabolic function. As liver glycogen is expended even during sleep, it is necessary to rapidly increase it through breakfast. In geriatric patients, in addition to the physiological aging of the liver, pathological aging may also reduce its function. Therefore, rapid glycogen synthesis is necessary at breakfast following fasting after dinner. Thus, it is believed that the active intake of carbohydrates that is easily expended at breakfast may promote sugar metabolism and contribute to the recovery of liver function.
In this study, we investigated the relationship between Alb-RC and breakfast NPC/N in geriatric patients. Current findings and discussions support, the usefulness of increasing the ratio of carbohydrate intake, non-protein energy intake, and NPC/N at breakfast. Therefore, it is recommended for older adults to support their dietary needs by increasing non-protein energy intake at breakfast within the appropriate range to improve their Alb.
Limitations of the study
The limitations of this study are that it is a retrospective study rather than an intervention study, the subjects are limited, and the number of cases is small as geriatric patients admitted to a local small-scale hospital were targeted. Therefore, it is undeniable that there are limitations in the interpretation of results. We used a stepwise method in this study because of the small sample size; however, it would be preferable to increase the number of subjects and analyze using a non-stepwise method to compare outcomes with other studies with similar objectives. The authors understand that the results should not be generalized because of the insufficient sample size. Nevertheless, we believe that it is worth reporting that the current result provides a good opportunity to begin verifying this issue through a future larger study.
Conclusions
It was shown that differences in breakfast NPC/N in nutrition intake observed in geriatric patients may affect the improvement of Alb at discharge. It may be useful to increase breakfast NPC/N within the acceptable range.
Acknowledgments
We would like to express our deep gratitude to the patients admitted to Nakai Hospital who provided their consent to participate in this study.
Financial Disclosure
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
This study was a retrospective study. We asked on the message board if we could use their data anonymously in our hospital. We have obtained informed consents for publication from all participants.
Author Contributions
Yasuko Fukuda: all processes including data collection, analysis, paper writing and so on. Mikako Ochi and Ryoko Kanazawa were responsible for medical chart survey. Hiromu Nakajima, Keisuke Fukuo and Masanobu Nakai: final proofreading of the manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
Alb: albumin; DP: dietary pattern; Alb-RC: change rate of albumin; NPC/N: non-protein calorie/nitrogen ratio; BW: body weight
| References | ▴Top |
- Richard JA, Dolores Durr E. Invited review: albumin: use in nutrition and support. Nutr Clin Pract. 1988;3:226-229.
doi pubmed - Jabbour J, Abou Ali AN, Rabeh W, Al-Shaar L, Avgerinos ED, Habib RH. Role of nutritional indices in predicting outcomes of vascular surgery. J Vasc Surg. 2019;70(2):569-579.e564.
doi pubmed - Butterworth CE. The skeleton in the hospital closet. Nutr Today. 1974;9:4-8.
doi - Bistrian BR, Blackburn GL, Hallowell E, Heddle R. Protein status of general surgical patients. JAMA. 1974;230(6):858-860.
doi pubmed - Li Z, Xu D, Jiang X, Li T, Su Y, Mu R. Anemia Is an Indicator for Worse Organ Damage Trajectories in Patients with Systemic Sclerosis: A Retrospective Study. J Clin Med. 2022;11(17):5013-5015.
doi pubmed - Fukuda Y, Kanazawa R, Yao N, Ishida T, Nakaoka A, Tazuhara M, Yao S, et al. Nutritional intake by meal time zone in geriatric patients is related to nutritional assessment index. J Clin Med Res. 2021;13(6):334-342.
doi pubmed - Fukuda Y, Kohara M, Hatakeyama A, Ochi M, Nakai M. Influence of geriatric patients' food preferences on the selection of discharge destination. J Clin Med Res. 2020;12(11):705-710.
doi pubmed - Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383.
doi pubmed - Tahara Y, Shibata S. Chronobiology and nutrition. Neuroscience. 2013;253:78-88.
doi pubmed - Kagawa Y, Shibata S, Oda H. Chrononutrition. Tokyo, Japan: Kagawa Nutrition Publishing Division; 2009 (in Japanese).
- Tahara Y, Otsuka M, Fuse Y, Hirao A, Shibata S. Refeeding after fasting elicits insulin-dependent regulation of Per2 and Rev-erbalpha with shifts in the liver clock. J Biol Rhythms. 2011;26(3):230-240.
doi pubmed - Nakamura Y, Youngju Choi, Akazawa N, Insung P, Kawana F, Satoh M, Tokuyama K, et al. Effect of bright-light exposure before sleep on human urine metabolome. J Phys Fitness Sports Med. 2019;8:89-96.
doi - Davies SK, Ang JE, Revell VL, Holmes B, Mann A, Robertson FP, Cui N, et al. Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci U S A. 2014;111(29):10761-10766.
doi pubmed - Dallmann R, Viola AU, Tarokh L, Cajochen C, Brown SA. The human circadian metabolome. Proc Natl Acad Sci U S A. 2012;109(7):2625-2629.
doi pubmed - Paschos GK, Ibrahim S, Song WL, Kunieda T, Grant G, Reyes TM, Bradfield CA, et al. Obesity in mice with adipocyte-specific deletion of clock component Arntl. Nat Med. 2012;18(12):1768-1777.
doi pubmed - Dyar KA, Ciciliot S, Wright LE, Bienso RS, Tagliazucchi GM, Patel VR, Forcato M, et al. Muscle insulin sensitivity and glucose metabolism are controlled by the intrinsic muscle clock. Mol Metab. 2014;3(1):29-41.
doi pubmed - Lamia KA, Storch KF, Weitz CJ. Physiological significance of a peripheral tissue circadian clock. Proc Natl Acad Sci U S A. 2008;105(39):15172-15177.
doi pubmed - Takahashi M, Ozaki M, Kang MI, Sasaki H, Fukazawa M, Iwakami T, Lim PJ, et al. Effects of meal timing on postprandial glucose metabolism and blood metabolites in healthy adults. Nutrients. 2018;10(11):1763.
doi pubmed - Anderson CF, Wochos DN. The utility of serum albumin values in the nutritional assessment of hospitalized patients. Mayo Clin Proc. 1982;57(3):181-184.
doi - Sayarath VG. Nutrition screening for malnutrition: potential economic impact at a community hospital. J Am Diet Assoc. 1993;93(12):1440-1442.
doi pubmed - McClave SA, Mitoraj TE, Thielmeier KA, Greenburg RA. Differentiating subtypes (hypoalbuminemic vs marasmic) of protein-calorie malnutrition: incidence and clinical significance in a university hospital setting. JPEN J Parenter Enteral Nutr. 1992;16(4):337-342.
doi pubmed - Fuhrman MP. The albumin-nutrition connection: separating myth from fact. Nutrition. 2002;18(2):199-200.
doi pubmed - Hector GP, Luis MAG, Julio S, Carlos MS, Xochitl AOL, Marco APC, Rafael B. Probnostic implications of serum albumin levels in patients with acute coronary syndromes. Am J Cardiol. 2017;119:951-958.
doi pubmed - Uemura K, Doi T, Lee S, Shimada H. Sarcopenia and low serum albumin level synergistically increase the risk of incident disability in older adults. J Am Med Dir Assoc. 2019;20(1):90-93.
doi pubmed - Basu R, Breda E, Oberg AL, Powell CC, Dalla Man C, Basu A, Vittone JL, et al. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes. 2003;52(7):1738-1748.
doi pubmed - Gordon DJ, Rifkind BM. Treating high blood cholesterol in the older patient. Am J Cardiol. 1989;63(16):48H-52H.
doi pubmed - Soejima K, Sato H, Hisaka A. Age-related change in hepatic clearance inferred from multiple population pharmacokinetic studies: comparison with renal clearance and their associations with organ weight and blood flow. Clin Pharmacokinet. 2022;61(2):295-305.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


