| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 15, Number 2, February 2023, pages 84-89
Quadratus Lumborum Blockade for Postoperative Analgesia in Infants and Children Following Colorectal Surgery
Katherine Manupipatponga, b, Anuranjan Ghimirea, Nguyen K. Trama, Richard Woodc, Joseph D. Tobiasa, b, Giorgio Venezianoa, b, d
aDepartment of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA
bDepartment of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
cDepartment of Pediatric Colorectal & Pelvic Reconstructive Surgery, Nationwide Children’s Hospital, Columbus, OH, USA
dCorresponding Author: Giorgio Veneziano, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH 43205, USA
Manuscript submitted December 7, 2022, accepted February 23, 2023, published online February 28, 2023
Short title: QLB in Pediatric Surgery
doi: https://doi.org/10.14740/jocmr4833
| Abstract | ▴Top |
Background: Adult studies have indicated that the quadratus lumborum block (QLB) may provide superior analgesia compared to single-shot neuraxial and other truncal peripheral nerve blocks. The technique is being increasingly used for postoperative analgesia in children undergoing lower abdominal surgery. To date, these pediatric reports have been limited by small sample sizes, which may hinder the interpretation of results and assessment of safety. In this study, we retrospectively examined QLBs performed at a large tertiary care hospital for evidence of effectiveness and safety in the pediatric colorectal surgery population.
Methods: Patients less than 21 years of age who underwent abdominal surgery and received a unilateral or bilateral QLB over a 4-year period were identified in the electronic medical record. Patient demographics, surgery type, and QLB characteristics were retrospectively examined. Pain scores and opioid consumption were tabulated over the first 72-h postoperative period. QLB procedural complications or adverse events attributable to the regional anesthetic were obtained.
Results: The study cohort included 204 QLBs in 163 pediatric-aged patients (2 days to 19 years of age, median age of 2.4 years). The most common indication was unilateral blockade for ostomy creation or reversal. The majority of QLBs were performed using ropivacaine 0.2% with a median volume of 0.6 mL/kg. The median opioid requirement in oral morphine milligram equivalents (MMEs) was 0.7, 0.5, and 0.3 MME/kg on the first, second, and third postoperative days, respectively. Median pain scores were less than 2 over each time period. Aside from block failure (incidence 1.2%), there were no complications or postoperative adverse events related to the QLBs.
Conclusion: This retrospective review in a large cohort of pediatric patients demonstrates that the QLB can be performed safely and efficiently in children undergoing colorectal surgery. The QLB provides adequate postoperative analgesia, has a high success rate, may limit postoperative opioid consumption, and is associated with a limited adverse effect profile.
Keywords: Quadratus lumborum block; Pediatric; Children; Postoperative analgesia; Local anesthetic
| Introduction | ▴Top |
Effective pain control after abdominal surgery enhances postoperative recovery, improves patient and parental satisfaction, facilitates hospital discharge, and reduces costs [1]. Regional anesthesia has become an important component of pain management after surgical procedures in the pediatric-aged patient, owing to its opioid-sparing effect and improved perioperative outcomes [2]. Ultrasonography has allowed for the evolution of peripheral nerve blockade as an analgesic adjunct, replacing neuraxial analgesia such as caudal epidural blockade in many clinical scenarios. Given their favorable adverse effect profile and prolonged duration of analgesia, peripheral nerve blocks have become more popular in infants and children [3].
In recent years, peripheral nerve blockade of the trunk has gained popularity as an alternative to neuraxial techniques in abdominal surgery [4]. The quadratus lumborum block (QLB) is an evolution of the transversus abdominis plane (TAP) block, providing extension of the cephalad sensory blockade to the T7 level [2]. Multiple studies have suggested the superiority of the QLB to neuraxial anesthesia and other truncal nerve blocks in providing analgesia for gynecological and urological procedures [5-7]. There are a paucity of clinical reports describing the use of QLBs in pediatric-aged patients following open colorectal procedures, such as bowel resection, exploratory laparotomy, or colostomy creation and revision. In this retrospective study, we described our experience with the QLB performed in children undergoing open lower abdominal and colorectal procedures at a tertiary care institution.
| Materials and Methods | ▴Top |
Approval for this study was acquired from the Institutional Review Board of Nationwide Children’s Hospital (00001681) and conducted in accordance with the regulations of the Declaration of Helsinki for research involving human subjects. As a retrospective cohort study, patients were deemed as exposed to no more than minimal risk and the need for individual written informed consent was waived. To maintain patient confidentiality, only deidentified data were used for the purpose of this study. Data collected during this study were stored in a secure location and only the collaborators directly involved in this study had access. All electronic files were stored on a secure, password protected network.
Patients less than 21 years of age who received a QLB for abdominal surgery over a 4-year period from January 2016 to December 2020 were identified. The institutional electronic medical record was reviewed for patient demographics, surgical procedure, and nerve block specifications. Additionally, adverse effects and complications related to the block were noted. The postoperative course was reviewed including pain scores and opioid consumption. Demographic information obtained included age, weight, gender, and co-existing medical conditions, such as the presence of spinal cord or vertebral abnormalities (spinal dysraphism), coagulation disturbances, or presurgical diagnosis of chronic pain. The type and length of the surgical procedure was obtained. QLB characteristics recorded included the approach used and whether the QLB was performed unilaterally or bilaterally. Data were collected on the local anesthetic type, concentration, volume, as well as any adjuncts utilized. The time required to perform the block and any complications attributable to performance of the QLB were noted. The following postoperative outcomes were analyzed for the first 72 h after surgery: pain scores, use of adjunctive analgesic agents, opioid consumption, and QLB-related complications. Pain was evaluated in our study population by either a visual analog scale (VAS), Wong-Baker pain (FACES) scale, or Faces, Legs, Agitation, Cry, and Consolability (FLACC) scale, depending on patient age and cognitive state. All three scales are validated assessment tools for pain which use a 10-point grading system [8], with zero being most comfortable or no pain. Pain scores were collected at 6-h intervals for all patients. Mean individual pain scores for the first 24, 48, and 72 h were tabulated and the median and interquartile scores over each 24-h time period were calculated. Opioid consumption was determined over the first postoperative 72 h with conversion of all administered intravenous and oral opioids to oral morphine milligram equivalents (MMEs) in mg/kg/day [9]. Patient records were investigated for adverse events that could be attributable to QLB blocks (site infection, bleeding, hypotension, or bradycardia).
Parametric continuous data were presented as means and standard deviations (SDs). Non-parametric data were presented as medians and interquartile ranges (IQRs). Categorical variables were presented as frequencies and percentages. All statistical analysis was performed using the Statistical Functions package (scipy.stats) in Python (Python Software Foundation, Wilmington, DE).
| Results | ▴Top |
The study cohort included 204 QLBs in 163 pediatric patients, 2 days to 19 years of age (median 2.4 years), who underwent abdominal surgery and received a QLB for postoperative analgesia from January 2016 to December 2020. Patient demographics and surgical procedures are summarized in Table 1. There were 137 who had surgery related to a bowel stoma (ileostomy/colostomy) creation or revision. The mean duration (SD) of surgery was 2.4 h (1.8). All QLBs were performed under general anesthesia using the anterior/transmuscular approach with ultrasound-guidance in lateral position. The QLBs were unilateral in 122 patients and bilateral in 41 patients. The median time (IQR) to complete the block was 5 min (4 - 9 min). The block success rate was 99%. The most common analgesic regimen for the QLB was 0.2% ropivacaine with 1:200,000 epinephrine and 0.2 mg/mL of preservative-free dexamethasone. QLB characteristics including local anesthetic type, volume, and dosage are displayed in Table 2. There were no documented complications during QLB placement.
 Click to view | Table 1. Demographic Data of the Study Cohort (n = 163) |
 Click to view | Table 2. QLB Characteristics |
The average pain score (0 - 10) was 2 ± 1, 1 ± 1, and 1 ± 1 during the first 24, 48, and 72 postoperative hours, respectively. The median pain scores were 1, 1, and 0 for the first 3 postoperative days, respectively. A total of 139 of 163 (85.3%) patients received postoperative opioids during the time period studied. Opioid requirements in median (IQR) oral MMEs were 0.7 (0.3 - 1.4), 0.5 (0.3 - 0.9), and 0.3 (0.2 - 0.7) MME/kg on the first, second, and third postoperative days, respectively (Fig. 1). The median number of intravenous and oral opioid administrations (IQR) was 4 (2 - 9), 3 (1 - 7), and 2 (1 - 5) during the first, second, and third postoperative days, respectively. The median time from anesthetic completion to the first opioid dose (IQR) was 1.2 h (0.2 - 3.8).
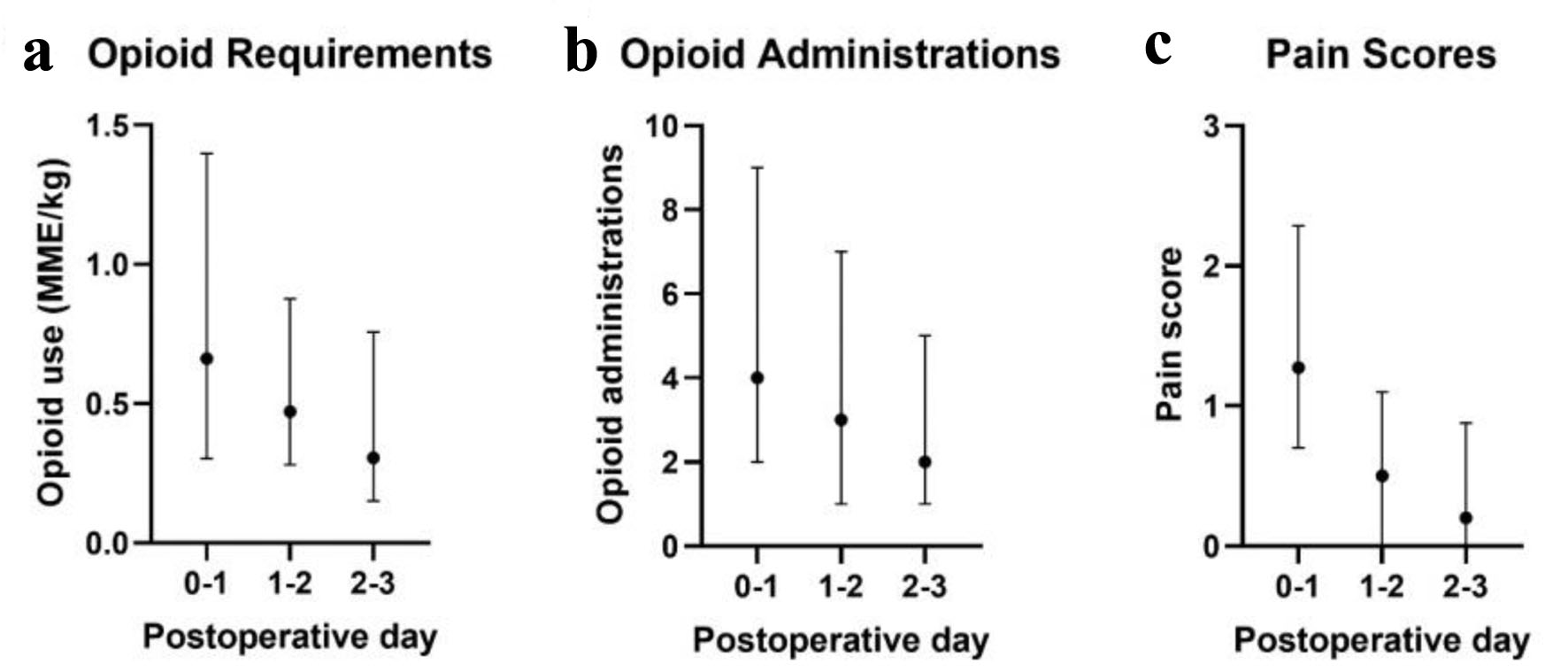 Click for large image | Figure 1. Postoperative opioid requirement (a), opioid administrations (b), and pain scores (c). Data show the median values and interquartile range. MME: morphine milligram equivalent. |
There were no QLB-related adverse events recorded during the perioperative course for any patient including hypotension, arrhythmias, local anesthetic systemic toxicity (LAST), convulsions, lower-extremity motor block, neurologic deficit, local hematoma or infection.
| Discussion | ▴Top |
Regional anesthesia is an essential component of multimodal pain control after pediatric surgery [2]. The QLB has gained popularity as a non-opioid adjunct in lower abdominal surgery, owing to superior analgesia and avoidance of neuraxial access [10-12]. While several studies have demonstrated the utility of the QLB in urological surgery and gynecological procedures [13-17], limited reports exist to describe its application in pediatric colorectal patients. This retrospective study summarizes the characteristics and safety profile of the QLB for pediatric patients following open lower abdominal and colorectal surgical procedures at a large tertiary care center. Our retrospective review suggests that the QLB can be performed safely and efficiently in anesthetized patients with a high success rate, and may serve as a useful analgesic adjunct for children undergoing open colorectal surgery.
The QLB is an “interfascial plane block”, first described by Blanco as a variant of the TAP block in 2007 [18]. The nomenclature describing the various approaches to the QLB has gone through multiple permutations in the literature over the years. Recently, the American Society of Regional Anesthesia and European Society of Regional Anesthesia issued a consensus paper on the terminology surrounding regional anesthetic techniques, including the QLB [19]. The three types of QLB are described based on the location of the deposition of local anesthetic in relation to the quadratus lumborum muscle (QLM) [20, 21]. Regardless of the approach used, the mechanisms responsible for analgesia are generally considered to be local anesthetic spread along the thoracolumbar plane and endothoracic fascia to the paravertebral space [22, 23]. In the lateral block, the local anesthetic is deposited on the lateral side of the QLM, at the level where the transversus abdominis muscle tapers off its aponeurosis. In the posterior block, the medication is deposited between the QLM and the medial lamina of the thoracolumbar fascia. In the anterior/transmuscular block, the local anesthetic is deposited in front of the QLM, at the level of its attachment to the transverse process of the L4 vertebra. The “Shamrock sign” is defined in this approach, where the transverse process of L4 vertebra represents the stem, with the erector spinae muscle as the posterior leaf, psoas major muscle as the anterior leaf, and QLM as the lateral leaf. It has been proposed that the anterior QLB may provide a broader dermatomal coverage than its counterparts, as the local anesthetic can spread more easily beyond the TAP to the paravertebral space. All of the QLBs performed in the current study were performed using the anterior approach based on previous practitioner clinical experiences with difficulty in expanding the inter-fascial space using the lateral QLB approach or the transversus abdominal plane block in patients with an ostomy in place. We postulate that regional inflammation from previous surgical procedures may cause the inter-fascial layers to become more adherent nearer to the ostomy.
The median volume of local anesthetic used for the QLB in pediatric colorectal surgery in this review (0.6 mL/kg) is comparable to prior reports [6, 7, 24, 25]. Contrast dye and magnetic resonance imaging data in adult cadavers have suggested that up to 20 mL of solution is required to achieve the desired T7-L1 sensory blockade, making it frequently the volume of choice in adult patients. The volume and concentration of local anesthetic used in reports describing QLBs in pediatric patients has varied according to the weight, surgical procedure and hence dermatomal coverage required, and provider preference. Samerchua et al reported effective postoperative analgesia with 0.2 mL/kg of 0.25% bupivacaine in the QLB for pediatric inguinal hernia repair [24]. Alternatively, QLBs performed by Oksuz et al and Sato for pediatric urological surgery utilized 0.5 mL/kg of 0.2% bupivacaine or ropivacaine [5-7]. In comparing the aforementioned studies, there appears to be limited correlation between postoperative pain scores and the local anesthetic volumes used. It is reassuring to note that there have not been any reports of LAST during performance of QLBs in children likely related to the avascular nature of the inter-fascial space, the routine use of ultrasound for QLBs, and the relative lack of proximity to major vessels.
To our knowledge, this is the first large, single-center retrospective study describing the use of the QLB in children undergoing colorectal surgery. Unfortunately, a comparable control group was not available at our institution during the study period because the QLB has become established as routine care for patients following surgery for ostomy creation/revision/reversal. As such, a true evaluation of analgesic efficacy is limited. Therefore, we have compared our data to those from a published cohort of similar patients that did not receive a QLB. The mean pain score during the first 24-h postoperative hours for our study cohort was 2 ± 1. George et al reported a mean 24-h postoperative pain score of 4.5 in 148 children who underwent laparoscopic and open colorectal surgery, none of whom received regional anesthesia [26]. The lower mean pain score in our study cohort provides support for our use of this technique as standard of care at our institution as it speaks to the analgesic efficacy of the QLB further supporting the evidence from the literature demonstrating improved analgesia with regional anesthesia versus systemic opioids. Furthermore, the median 24-h postoperative pain score (IQR) in our study cohort was 1 (1 - 2), lower than the 5 (4 - 6) reported by Sato et al in 22 children who received the QLB for ureteral implantation [5]. Differences in our study cohort included the predominant use of a unilateral QLB given the type of surgery and placement via the anterior versus posterior approach used by Sato and colleagues.
The first postoperative day opioid consumption (in morphine milligram equivalents) in our cohort (0.7 mg/kg/day) compares favorably to a report by Rizk et al of adult patients who underwent open and laparoscopic colorectal surgery without regional anesthesia receiving 44 and 21 mg/kg/day, respectively [27]. A smaller retrospective study reported a mean opioid consumption of 0.2 mg/kg/day in pediatric patients who received the QLB for colorectal surgery, though it is unclear whether this measurement was limited to the first postoperative day or averaged for the entire hospital course [28]. In the previously mentioned study by George et al, 98.7% of patients required opioid medications postoperatively if they did not receive an epidural or truncal block [26]. In comparison, 85.3% of children who received regional anesthesia in our investigation required postoperative opioids within the studied time period.
Enhanced pain control in our cohort is likely attributable to analgesic coverage of somatic abdominal pain by the QLB. However, persistent opioid requirement may be secondary to the visceral pain component not completely alleviated by the regional block. As a retrospective study, strict adherence to guidelines controlling opioid administration was not in place. Additionally, it is not feasible to regulate opioid administration in older patients who were given patient-controlled analgesia pumps (such as in cases of prophylactic self-administration). As the median pain score does not directly correlate with the maximum pain score, it is possible that narcotic medication was administered for a higher pain score as opposed to the low reported median.
Potential adverse effects of the QLB include lower limb weakness (due to spread of local anesthetic to the lumbar plexus), delayed mobilization, and hypotension (due to spread of local anesthetic to the paravertebral and epidural space). Reassuringly, records of these adverse events were not found in any of the study cohort. This is remarkable given the large number of patients, young median age, and larger local anesthetic volumes described in this study compared to previous reports and lends further evidence to the safety of the QLB in children. While statistical calculation of the approximate complication rate is not achievable with this study’s sample size, previous randomized controlled trials have supported the safety of the QLB in adults [21].
The QLB may provide additional advantages when compared to neuraxial techniques such as a caudal epidural block, including the ability to provide unilateral blockade, avoidance of motor blockade, and lack of urinary retention. Furthermore, the technique can be used in patients with contraindications to neuraxial analgesia including spinal dysraphism and coagulation disturbances (Table 1). A large portion of our study cohort contained patients with a diagnosis of anorectal malformation. These patients are more likely to have known, or yet undetected, sacral abnormalities and/or tethered spinal cord that makes caudal epidural block unadvisable.
As the QLB is central to the multimodal analgesic regimen for colorectal surgery at our institution, this study is limited by lack of formal control group. Inherent to the retrospective nature of the study, standardization of the intraoperative anesthetic technique, the postoperative analgesic regimen, and the concentration and volume of the local anesthetic agent as well as adjunctive agents for the QLB were not feasible. Additionally, although the majority of patients had procedures involving ostomy placement or creation, there were a variety of other diverse surgical procedures. As such, block characteristics and postoperative recovery (i.e., opioid consumption, pain scores) could potentially fluctuate based on the degree of surgical invasiveness, laterality of the QLB (unilateral vs. bilateral), and patient co-morbid features. Although the postoperative analgesic regimen was not controlled, given our routine clinical practice, there is standardization for assessment of postoperative pain including routine use of pain scores.
While the QLB has been described to provide comparable or superior analgesia to TAP and neuraxial blocks for inguinal hernia repairs and other urological/gynecological procedures [5-7], its use in children is still not as widespread as in adults. This may be due to institution-specific protocols and the experience and comfort of the provider. For example, the subspecialty trained regional anesthesia team performs the majority of QLBs at our institution. Despite these limitations, the technique appears to be rising in popularity in children as more pediatric-specific data are published.
Conclusion
At our institution, the QLB has become the regional anesthetic technique of choice for children undergoing ostomy-related surgery. This retrospective review demonstrates that the QLB can be performed safely and swiftly, with a high success rate and a negligible adverse effect profile. The QLB appears to enhance pain control after pediatric colorectal surgery, as suggested by lower postoperative pain scores and reduced opioid consumption when compared to prior published reports. Future investigation should include randomized controlled prospective analyses of optimal local anesthetic dosing (concentration and volume), use of adjunctive agents such as dexamethasone, and efficacy across different types of invasive lower abdominal procedures.
Acknowledgments
The authors would like to acknowledge the hard work and expertise of the Nationwide Children’s Hospital Anesthesiology research team. We would also like to show our gratitude to Dr. Joseph Tobias for his support and mentorship.
Financial Disclosure
The authors have no funding sources to disclose.
Conflict of Interest
The authors have no conflict of interest to disclose.
Informed Consent
As a retrospective observational study, patients were deemed as exposed to no more than minimal risk and the need for individual written informed consent was waived.
Author Contributions
Giorgio Veneziano and Joseph Tobias conceived the study concept and design. Katherine Manupipatpong and Anuranjan Ghimire assisted in data collection and wrote the manuscript draft. Nguyen Tram performed the data analysis. Giorgio Veneziano and Joseph Tobias revised the final manuscript for submission.
Data Availability
Data collected during this study was stored in a secure location and only the collaborators directly involved in this study have access.
Abbreviations
QLB: quadratus lumborum block; QLM: quadratus lumborum muscle; TAP: transversus abdominis plane; VAS: visual analog scale; FLACC: Faces, Legs, Agitation, Cry, Consolability; MME: morphine milligram equivalent; LAST: local anesthetic systemic toxicity; IQR: interquartile range; SD: standard deviation
| References | ▴Top |
- Wang Y, Wu T, Terry MJ, Eldrige JS, Tong Q, Erwin PJ, Wang Z, et al. Improved perioperative analgesia with ultrasound-guided ilioinguinal/iliohypogastric nerve or transversus abdominis plane block for open inguinal surgery: a systematic review and meta-analysis of randomized controlled trials. J Phys Ther Sci. 2016;28(3):1055-1060.
doi pubmed - Heydinger G, Tobias J, Veneziano G. Fundamentals and innovations in regional anaesthesia for infants and children. Anaesthesia. 2021;76(Suppl 1):74-88.
doi pubmed - Polaner DM, Taenzer AH, Walker BJ, Bosenberg A, Krane EJ, Suresh S, Wolf C, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012;115(6):1353-1364.
doi pubmed - Carline L, McLeod GA, Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117(3):387-394.
doi pubmed - Sato M. Ultrasound-guided quadratus lumborum block compared to caudal ropivacaine/morphine in children undergoing surgery for vesicoureteric reflex. Paediatr Anaesth. 2019;29(7):738-743.
doi pubmed - Oksuz G, Arslan M, Urfalioglu A, Guler AG, Teksen S, Bilal B, Oksuz H. Comparison of quadratus lumborum block and caudal block for postoperative analgesia in pediatric patients undergoing inguinal hernia repair and orchiopexy surgeries: a randomized controlled trial. Reg Anesth Pain Med. 2020;45(3):187-191.
doi pubmed - Oksuz G, Bilal B, Gurkan Y, Urfalioglu A, Arslan M, Gisi G, Oksuz H. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. 2017;42(5):674-679.
doi pubmed - von Baeyer CL. Children's self-reports of pain intensity: scale selection, limitations and interpretation. Pain Res Manag. 2006;11(3):157-162.
doi pubmed - Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S. Clinical application of opioid equianalgesic data. Clin J Pain. 2003;19(5):286-297.
doi pubmed - Aksu C, Sen MC, Akay MA, Baydemir C, Gurkan Y. Erector Spinae Plane Block vs Quadratus Lumborum Block for pediatric lower abdominal surgery: A double blinded, prospective, and randomized trial. J Clin Anesth. 2019;57:24-28.
doi pubmed - Naaz S, Kumar R, Ozair E, Sahay N, Asghar A, Jha S, Akhil VP. Ultrasound Guided Quadratus Lumborum Block Versus Transversus Abdominis Plane Block for Post-operative Analgesia in Patients Undergoing Total Abdominal Hysterectomy. Turk J Anaesthesiol Reanim. 2021;49(5):357-364.
doi pubmed - Ipek CB, Kara D, Yilmaz S, Yesiltas S, Esen A, Dooply S, Karaaslan K, et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. 2019;49(5):1395-1402.
doi pubmed - Saleh AH, Abdallah MW, Mahrous AM, Ali NA. Quadratus lumborum block (transmuscular approach) versus transversus abdominis plane block (unilateral subcostal approach) for perioperative analgesia in patients undergoing open nephrectomy: a randomized, double-blinded, controlled trial. Braz J Anesthesiol. 2021;71(4):367-375.
doi pubmed - Elsharkawy H, Ahuja S, Sessler DI, Maheshwari K, Mao G, Sakr Esa WA, Soliman LM, et al. Subcostal anterior quadratus lumborum block versus epidural block for analgesia in open nephrectomy: a randomized clinical trial. Anesth Analg. 2021;132(4):1138-1145.
doi pubmed - Kang R, Lee S, Kim GS, Jeong JS, Gwak MS, Kim JM, Choi GS, et al. Comparison of analgesic efficacy of erector spinae plane block and posterior quadratus lumborum block in laparoscopic liver resection: a randomized controlled trial. J Pain Res. 2021;14:3791-3800.
doi pubmed - Meouchy MG, Awaida CJ, Jabbour HJ, Rayess YA, Jabbour SF, Nasr MW. Ultrasound-guided quadratus lumborum block for postoperative pain in abdominoplasty: a randomized controlled study. Plast Reconstr Surg. 2021;147(4):851-859.
doi pubmed - Visoiu M, Yakovleva N. Continuous postoperative analgesia via quadratus lumborum block - an alternative to transversus abdominis plane block. Paediatr Anaesth. 2013;23(10):959-961.
doi pubmed - Blanco R. TAP block under ultrasound guidance: the description of a "no pops technique". Reg Anesth Pain Med. 2007;32:130.
doi - El-Boghdadly K, Wolmarans M, Stengel AD, Albrecht E, Chin KJ, Elsharkawy H, Kopp S, et al. Standardizing nomenclature in regional anesthesia: an ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med. 2021;46(7):571-580.
doi pubmed - Akerman M, Pejcic N, Velickovic I. A Review of the Quadratus Lumborum Block and ERAS. Front Med (Lausanne). 2018;5:44.
doi pubmed - Lin C, Wang X, Qin C, Liu J. Ultrasound-Guided Posterior Quadratus Lumborum Block for Acute Postoperative Analgesia in Adult Patients: A Meta-Analysis of Randomized Controlled Trials. Ther Clin Risk Manag. 2022;18:299-313.
doi pubmed - Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66(11):1023-1030.
doi pubmed - Hussein MM. Ultrasound-guided quadratus lumborum block in pediatrics: trans-muscular versus intra-muscular approach. J Anesth. 2018;32(6):850-855.
doi pubmed - Samerchua A, Leurcharusmee P, Panichpichate K, Bunchungmongkol N, Wanvoharn M, Tepmalai K, Khorana J, et al. A Prospective, randomized comparative study between ultrasound-guided posterior quadratus lumborum block and ultrasound-guided ilioinguinal/iliohypogastric nerve block for pediatric inguinal herniotomy. Paediatr Anaesth. 2020;30(4):498-505.
doi pubmed - Genc Moralar D, Tok Cekmecelioglu B, Aslan M, Hergunsel GO. Effect of quadratus lumborum block on postoperative analgesic requirements in pediatric patients: a randomized controlled double-blinded study. Minerva Anestesiol. 2020;86(2):150-156.
doi pubmed - George JA, Salazar AJG, Irfan A, Prichett L, Nasr IW, Garcia AV, Boss EF, et al. Effect of implementing an enhanced recovery protocol for pediatric colorectal surgery on complication rate, length of stay, and opioid use in children. J Pediatr Surg. 2022;57(7):1349-1353.
doi pubmed - Rizk E, Haas EM, Swan JT. Opioid-sparing effect of liposomal bupivacaine and intravenous acetaminophen in colorectal surgery. J Surg Res. 2021;259:230-241.
doi pubmed - Short HL, Heiss KF, Burch K, Travers C, Edney J, Venable C, Raval MV. Implementation of an enhanced recovery protocol in pediatric colorectal surgery. J Pediatr Surg. 2018;53(4):688-692.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


