| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 11, November 2022, pages 474-486
Trends and Disparities in Outcomes of Clostridioides difficile Infection Hospitalizations in the United States: A Ten-Year Joinpoint Trend Analysis
Pius Ehiremen Ojemolona, f , Hafeez Shakab, Robert Kwei-Nsoroa, Hisham Laswia, Ebehiwele Ebhohonc, Abdultawab Shakad, Abdul-Rahman Abusalima, Benjamin Mbaa, e
aDepartment of Internal Medicine, John H. Stroger Jr. Hospital of Cook County, Chicago, IL, USA
bDepartment of Medicine, John H. Stroger Jr. Hospital of Cook County, Chicago, IL, USA
cDepartment of Internal Medicine, Lincoln Medical Center, Bronx, NY, USA
dWindsor University School of Medicine, St. Kitts
eProfessor of Medicine, Rush Medical College, Chicago, IL, USA
fCorresponding Author: Pius Ehiremen Ojemolon, Department of Internal Medicine, John H. Stroger, Jr. Hospital of Cook County, Chicago, IL 60612, USA
Manuscript submitted October 9, 2022, accepted November 23, 2022, published online November 29, 2022
Short title: Clostridioides difficile Infection Trends
doi: https://doi.org/10.14740/jocmr4828
| Abstract | ▴Top |
Background: Clostridioides difficile infection (CDI) is the most frequently reported nosocomial infection. This study aimed to describe epidemiological trends, sex, race, and economic disparities in clinical and mortality outcomes among CDI hospitalizations over a decade.
Methods: We queried Nationwide Inpatient Sample databases from 2010 to 2019, identified hospitalizations with CDI, and obtained the incidence and admission rate of CDI per 100,000 adult hospitalizations each year. We analyzed trends in mortality rate, mean length of hospital stay (LOS), and mean total hospital charge (THC). We highlighted disparities in outcomes stratified by sex, race, and mean household income quartile.
Results: Of the 305 million hospitalizations included in our study, over 3.3 million were complicated by CDI, with 1.01 million principal admissions for CDI. Among primary admissions for CDI, the mortality rate decreased from 3.2% in 2010 to 1.4% in 2019. Mean LOS reduced from 6.6 to 5.3 days while mean THC increased from US$40,593 to US$42,934 between 2010 and 2019. Females had a 21% decrease in adjusted odds of mortality compared to males (all P-trends < 0.001). Middle-aged and elderly patients had aOR of 4.96 and 14.74 respectively for mortality when compared to young adults (P < 0.001). Mortality rates showed a steady decline among Whites over the study period. Mean LOS trends were similar across racial subgroups.
Conclusions: Outcomes of CDI hospitalizations improved over the studied decade. Older age, male sex, and being from a minority racial group were associated with worse clinical and mortality outcomes. Further studies are needed to elucidate the reasons for these findings.
Keywords: Clostridioides difficile infection; Hospitalization; Disparities; Trends; Mortality
| Introduction | ▴Top |
Clostridioides difficile infection (CDI) is the most frequently reported pathogen in nosocomial infections and accounts for 12.1% of healthcare-associated infections in the United States [1]. The clinical severity of CDI is a spectrum ranging from a mild, self-limited diarrheal illness to fulminant, life-threatening colitis [2]. Data from active population- and laboratory-based surveillance show that approximately half a million cases of CDI occur each year in the United States, with almost 30,000 deaths reported in 2011 [3]. The total annual CDI-attributable health care cost in the United States is estimated at US$6.3 billion with nearly 2.4 million days of inpatient stay attributable to CDI [4].
The Centers for Disease Control and Prevention’s Emerging Infections Program demonstrated a decrease in the estimated national burden of CDI and associated hospitalizations from 2011 through 2017 [5]. However, the proportion of community-acquired CDI has been increasing over time. Cases of CDI have been increasingly reported outside of acute care facilities over the last few years with progressively more cases being diagnosed and treated without hospitalization [3, 6].
While the above-stated changes in the epidemiology of CDI have been extensively documented in the literature, there is a relative paucity of research on the impact of sociodemographic indices on CDI hospitalizations and outcomes. This study aimed to describe the epidemiological trends, sex, race, and economic disparities in clinical and mortality outcomes among hospitalizations with CDI over a decade.
| Materials and Methods | ▴Top |
Design and data source
This was a retrospective longitudinal trends study involving hospitalizations with CDI in the US from 2010 to 2019. We sourced data from the Nationwide Inpatient Sample (NIS) databases from 2010 through 2019. The NIS is developed by the Healthcare Cost and Utilization Project (HCUP), a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS is a database of hospital inpatient stays derived from billing data submitted by hospitals to statewide data organizations across the US, covering more than 97% of the US population [7]. The provided dataset for a given calendar year approximates a 20% stratified sample of discharges from US hospitals, excluding rehabilitation and long-term acute care hospitals. This dataset is weighted to obtain US national estimates [8]. Databases before 2016 were coded using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS). Databases from 2016 were coded using the ICD-10-CM/PCS. The 2015 NIS has both ICD-9 and 10 codes, hence requiring a combination of both codes to obtain the studied cohort in keeping with the HCUP regulations [9]. In this study, we weighted the 9 months of ICD-9 data in 2015 for the entire year. In the NIS, diagnoses are divided into two separate categories: principal diagnosis and secondary diagnoses. A principal diagnosis was the ICD code attributed as the reason for hospitalization. Secondary diagnoses were any ICD code discharge diagnosis other than the principal diagnosis. We obtained total yearly adult hospitalizations from the NIS databases. This manuscript conforms with the STROBE statement for reporting observational studies.
Study population and variables
We queried NIS databases from 2010 to 2019 for this study. The study involved two cohorts of hospitalizations: any hospitalization with CDI and hospitalizations with a principal admitting diagnosis of CDI. We searched the databases for hospitalizations using ICD codes (008.45 and A04.7x). We excluded hospitalizations involving patients less than 18 years. The NIS includes variables on patient demographics, including age, sex, race, median household income (MHOI) for patient’s zip code (income quartiles referred to patients as 1 - low income, 2 - middle income, 3 - upper middle income, 4 - high income), and primary payer. It also contains hospital-specific variables including bed size, teaching status, and location. We assessed the comorbidity burden using Sundararajan’s adaptation of the modified Deyo’s Charlson comorbidity index (CCI). This modification groups CCI into four groups in increasing risk for mortality. It has been adapted to population-based research. A score of > 3 has about a 25% 10-year mortality, while a score of 2 or 1 has a 10% and 4% 10-year mortality, respectively. This cutoff point was chosen as a means of assessment of the increased risk of mortality [10]. Total hospital charge (THC) was adjusted for inflation using the Medical Expenditure Panel Survey index for hospital care, with 2019 as the reference point [11].
Outcome measures
We highlighted the biodemographic trends over time of CDI hospitalizations. Specifically, we obtained the CDI admission rate and the incidence of CDI among all hospitalizations. We calculated the crude CDI admission rate per 100,000 adult hospitalizations and the incidence of CDI per 100,000 adult hospitalizations during each calendar year. We analyzed trends in inpatient mortality rate, mean length of hospital stay (LOS), and mean THC of both cohorts. We also highlighted disparities in outcomes of CDI hospitalizations stratified by sex (male and female), race (Whites, Blacks, and Hispanics), and MHOI quartile (low-income quartile - LIQ and high-income quartile - HIQ).
Statistical analysis
Stata® Version 16 software (StataCorp, TX, USA) and Joinpoint Regression Program, Version 4.9.1.0 were used for data analysis. We analyzed and reported the weighted sample following HCUP regulations for using the NIS database. Age was grouped as 18 - 44 years representing young adults, 45 - 64 years representing middle-aged adults, and 65 years and above representing elderly. The incidence of CDI among hospitalizations was calculated following the HCUP methodology for disease incidence and prevalence [12]. The crude admission rate was calculated by dividing total CDI hospitalizations as the principal diagnosis by the total adult hospitalization for each calendar year studied and expressed per 100,000 hospitalizations. The incidence of CDI per 100,000 adult hospitalizations was obtained by dividing the total hospitalizations with CDI by the total number of adult hospitalizations. This was also expressed as per 100,000 adult hospitalizations. We used multivariable regression analysis to calculate the incidence and admission rates adjusted for age categories, sex, and race using predictive margins. We subsequently used Joinpoint regression analysis to obtain the trends in rates over the study duration, using the adjusted rates and standard errors. Joinpoint regression analysis has been widely used and validated by the National Institutes of Health (NIH) National Cancer Institute to model non-linear trends in cancer rates over a given period [13]. This has been adopted in prior HCUP database research [14, 15]. We used multivariable regression trend analysis to obtain trends in mortality, LOS, and THC adjusted for age categories, sex, and race. All P values were two-sided, with 0.05 set as the threshold for statistical significance.
Ethical compliance with human/animal study
The NIS database lacks patient and hospital level identifiers. This study, therefore, did not require Cook County Health Institutional Review Board approval.
Data availability statement
The NIS is a large publicly available all-payer inpatient care database in the United States, containing data on more than seven million hospital stays per year. Its large sample size is ideal for developing national and regional estimates and enables analyses of rare conditions, uncommon treatments, and special populations. Datasets are available through the HCUP central distributor on request.
| Results | ▴Top |
Hospitalizations with CDI
Over 300 million hospitalizations were included in our study over the period from 2010 to 2019. Of these hospitalizations, 1.1% (more than 3.3 million) were complicated by CDI with the CDI incidence rate amongst hospitalizations down-trending from 1,001 per 100,000 hospitalizations in 2010 to 871 per 100,000 hospitalizations in 2019. When adjusted for age and sex, there was an average annual percentage change (AAPC) of -2% reduction in the incidence of CDI among hospitalizations over the study period. In 2010, CDI was the principal reason for hospitalization in 33.1% of these hospitalizations with CDI, with a reduction in that proportion to 29% in 2019. Other top reasons for hospitalizations included unspecified sepsis, pneumonia from unspecified organism, and acute kidney injury. Joinpoint regression analysis showed an increase in the adjusted CDI incidence rate from 2010 to 2015 (annual percent change (APC) = 2.88%). There subsequently was a decreased incidence from 2015 to 2019 (APC = -8.11%), as shown in Figure 1.
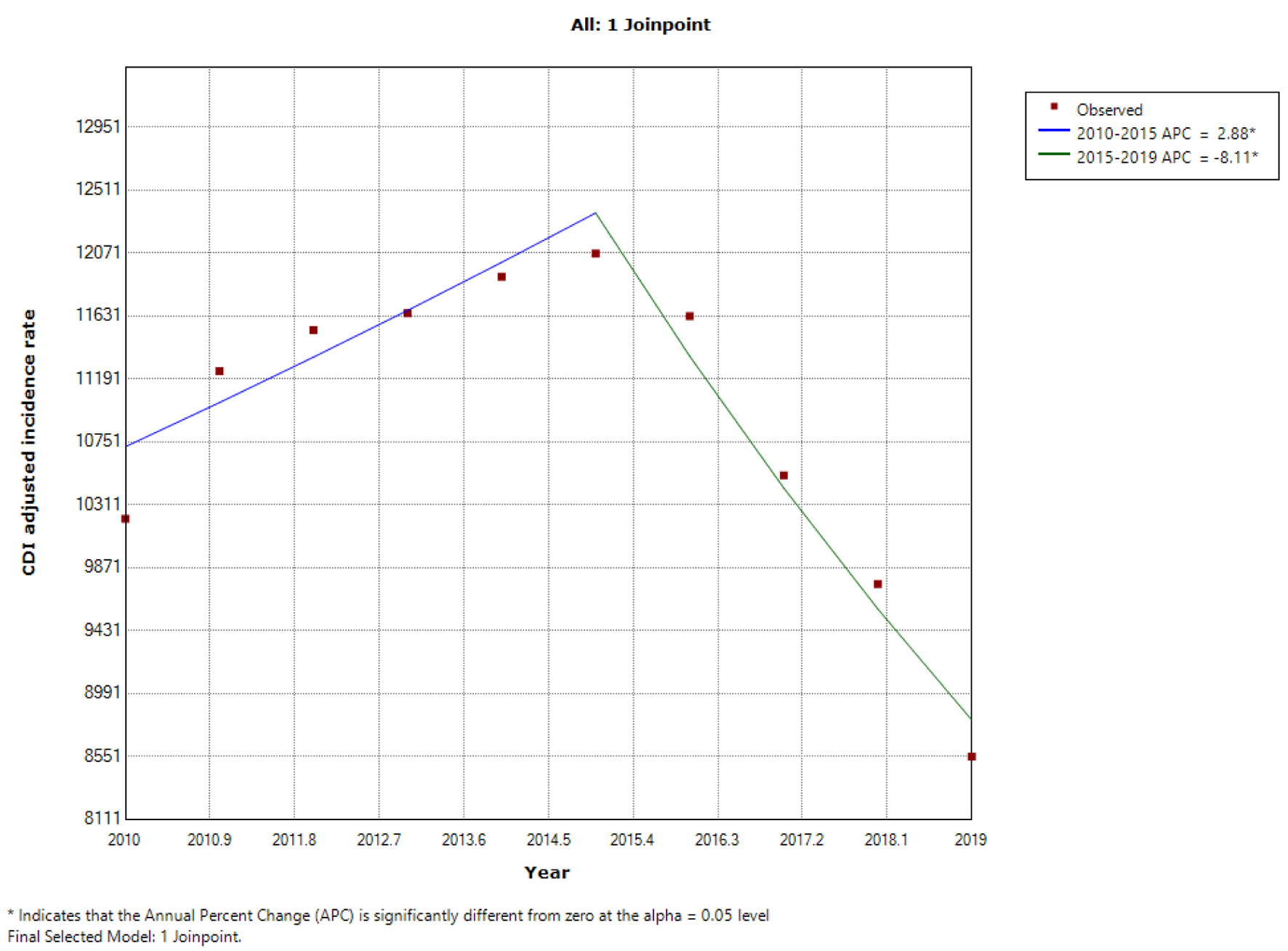 Click for large image | Figure 1. Trend in the adjusted incidence of CDI among all hospitalizations from 2010 to 2019. *Statistically significant. APC: annual percentage change; CDI: Clostridioides difficile infection. |
Table 1 shows the biodemographic distribution of hospitalizations with CDI. Older age groups were consistently at higher odds of hospitalization with CDI compared to young adults with elderly hospitalizations having higher odds than middle-aged hospitalizations. Middle-aged and elderly patients had adjusted odds ratios (aORs) of 2.54 and 3.86 respectively for hospitalization with CDI when compared to young adults (P < 0.001). Females had a 12% increase in adjusted odds of hospitalization with CDI compared to males over the study period (P < 0.001).
 Click to view | Table 1. Biodemographic Data of Hospitalizations With CDI |
The mortality rate in the cohort of hospitalizations with CDI was 6.9% over the study period and decreased from 8.4% in 2010 to 5.8% in 2019. The mean LOS decreased from 11.6 to 9.8 days and the mean THC increased from US$93,521 to US$108,357 (all P-trends < 0.001). When adjusted for age and sex, there was a -4% APC in mortality among hospitalizations with CDI over the study period. On sex subgroup analysis, females had a significantly lower mortality rate (Fig. 2). On racial subgroup analysis, mortality rates were lowest among Whites over the study period, most improved in Hispanics over the study period with the least improvement in Blacks (Fig. 3). Mean LOS trends were also similar to mortality trends across the three racial subgroups. Mortality rates, mean LOS, and mean THC followed similar trends over the study period in hospitalizations with mean household income (MHOI) quartile 1 when compared to those with MHOI quartile 4 (Table 2).
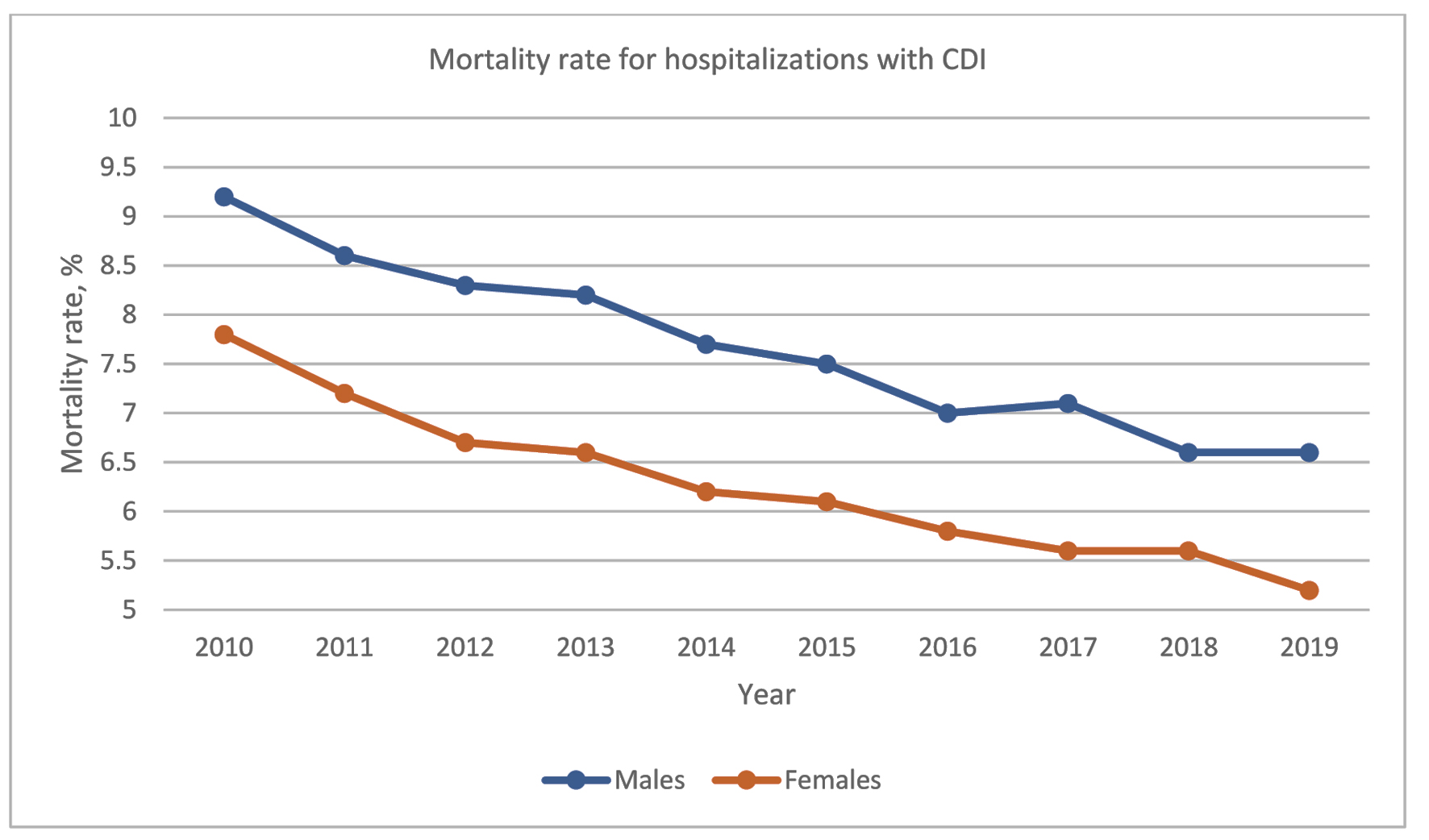 Click for large image | Figure 2. Trend in the mortality rate for hospitalizations with CDI (sex subgroup analysis). CDI: Clostridioides difficile infection. |
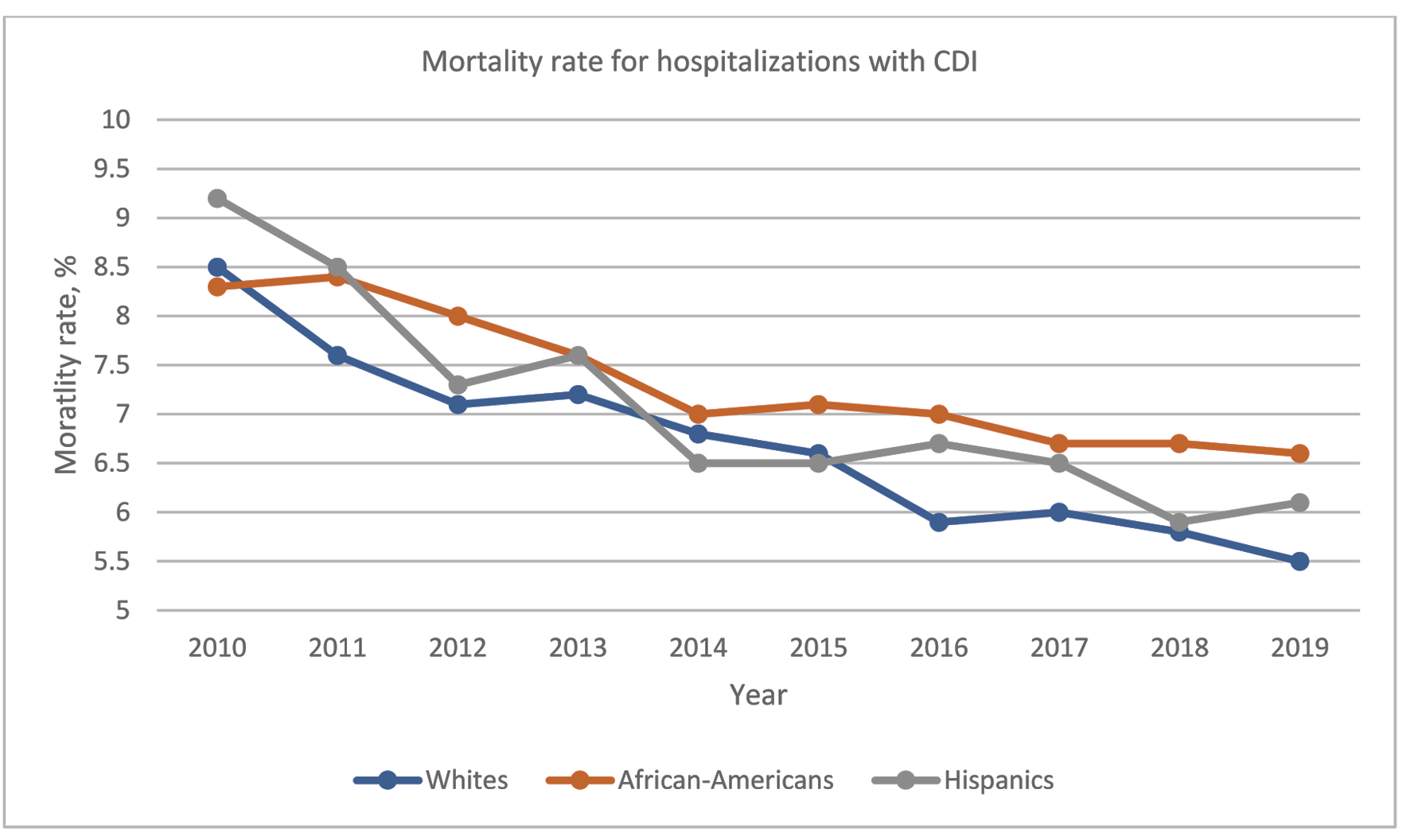 Click for large image | Figure 3. Trend in the mortality rate for hospitalizations with CDI (racial subgroup analysis). CDI: Clostridioides difficile infection. |
 Click to view | Table 2. Outcomes of Hospitalizations With CDI |
Middle-aged and elderly patients had aOR of 2.15 and 3.58 respectively for mortality when compared to young patients (P < 0.001). Females had a 22% decrease in adjusted odds of mortality compared to males over the study period (P < 0.001).
When adjusted for age and sex, there was an annual 0.19 decrease in LOS over the study period (P < 0.001), with this finding similar across the different racial subgroups.
Patients hospitalized for CDI
There were over 1 million hospitalizations with CDI as the reason for inpatient stay, representing 30.6% of all hospitalizations with CDI over the study period. The AAPC for CDI admissions was -3.2% over the study period. Joinpoint regression analysis showed a non-statistically significant increase in adjusted CDI admission rate from 2010 to 2012 (APC = 4.15%), with a subsequent reduction in adjusted CDI admission rate from 2012 to 2016 (APC = -2.17%) which was also not statistically significant. From 2016 to 2019, there was a statistically significant trend towards reduction in adjusted CDI admission rate (APC = -9.87%) (Fig. 4).
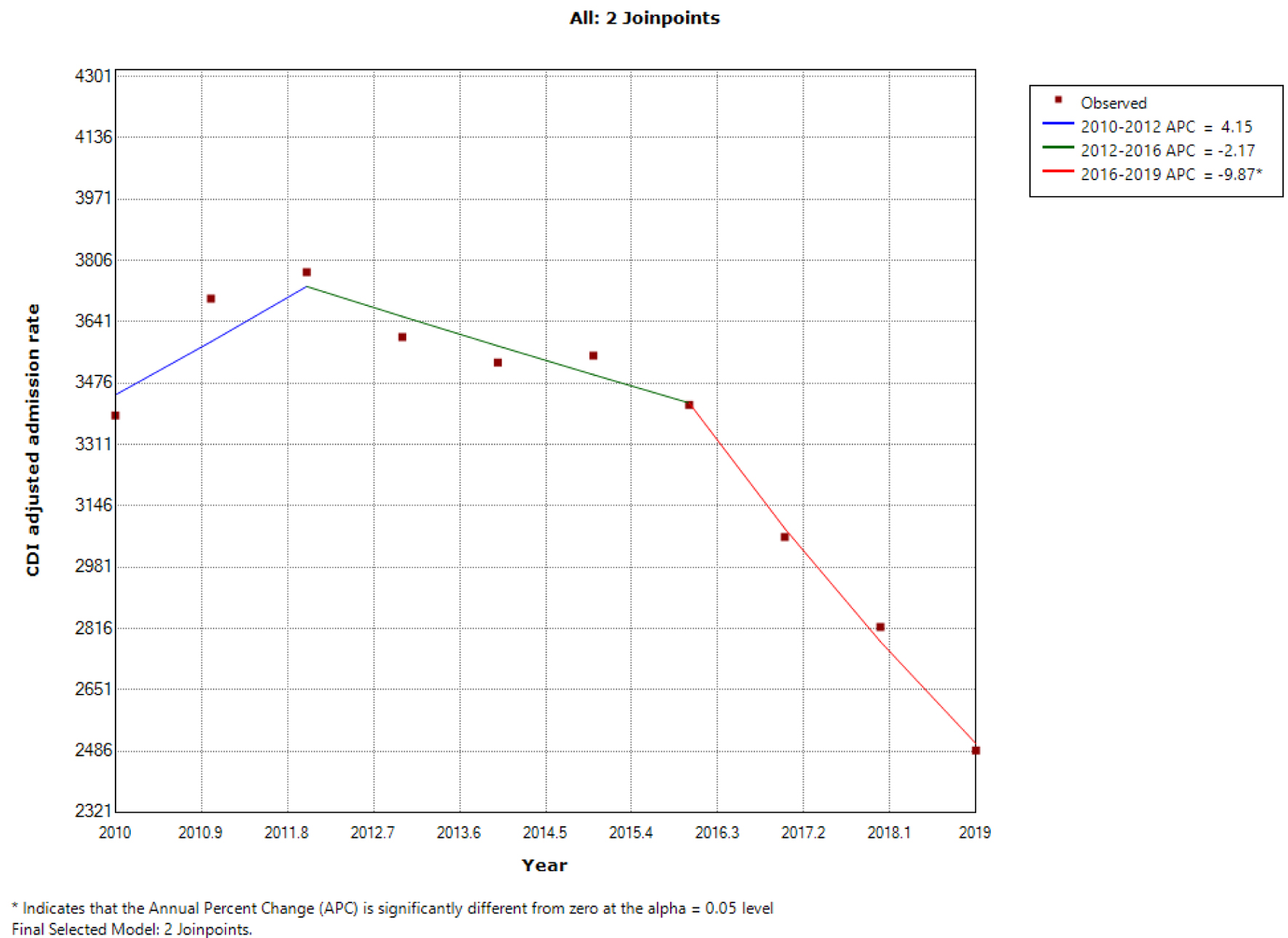 Click for large image | Figure 4. Trends in adjusted CDI admission rate from 2010 to 2019. *Statistically significant. APC: annual percentage change; CDI: Clostridioides difficile infection. |
The mean age of CDI admissions decreased from 69.4 years in 2010 to 66.6 years in 2019 with the proportion of elderly patients similarly down-trending from 66.3% in 2010 to 60.3% in 2019 (both P-trends < 0.001). The proportion of CDI admissions with CCI scores ≥ 3 increased from 28.4% in 2010 to 39.3% in 2019 (P-trend < 0.001). The highest proportion of the primary payer across each year was Medicare, and most patients were managed at large hospitals (both P < 0.001) (Table 3).
 Click to view | Table 3. Biodemographic Data of Hospitalizations With Principal Admitting Diagnosis of CDI |
The mortality rate in patients admitted for CDI was 1.9% over the study period, down-trending from 3.2% in 2010 to 1.4% in 2019. When adjusted for age and sex, the AAPC for mortality was -10.2%. The mean LOS reduced from 6.6 days in 2010 to 5.3 days in 2019 and the mean THC increased from US$40,593 to US$42,934 (all P-trends < 0.001). On sex subgroup analysis, mortality rates showed a downtrend in males and females over the study period (Fig. 5). A similar trend was observed in mean LOS in males and females while mean THC increased in both groups over the study period (Table 4). On racial subgroup analysis, mortality rates showed a steady decline among Whites and Blacks over the study period (Fig. 6). Mean LOS trends were also similar across the three racial subgroups. Mortality rates, mean LOS, and mean THC followed similar trends over the study period in hospitalizations among LIQ and HIQ patients.
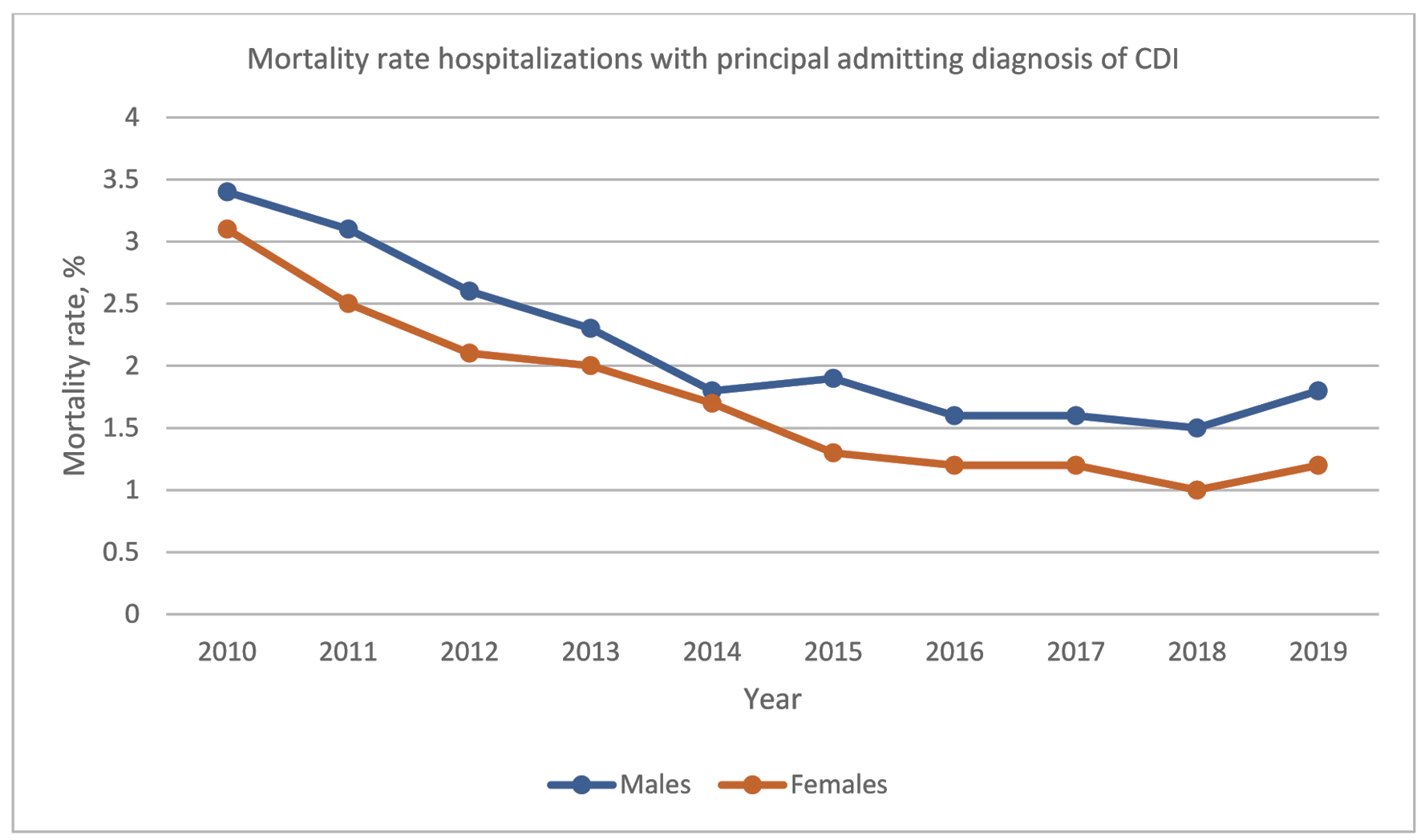 Click for large image | Figure 5. Trend in mortality rate hospitalizations with a principal admitting diagnosis of CDI (sex subgroup analysis). CDI: Clostridioides difficile infection. |
 Click to view | Table 4. Outcomes of Hospitalizations With Principal Admitting Diagnosis of CDI |
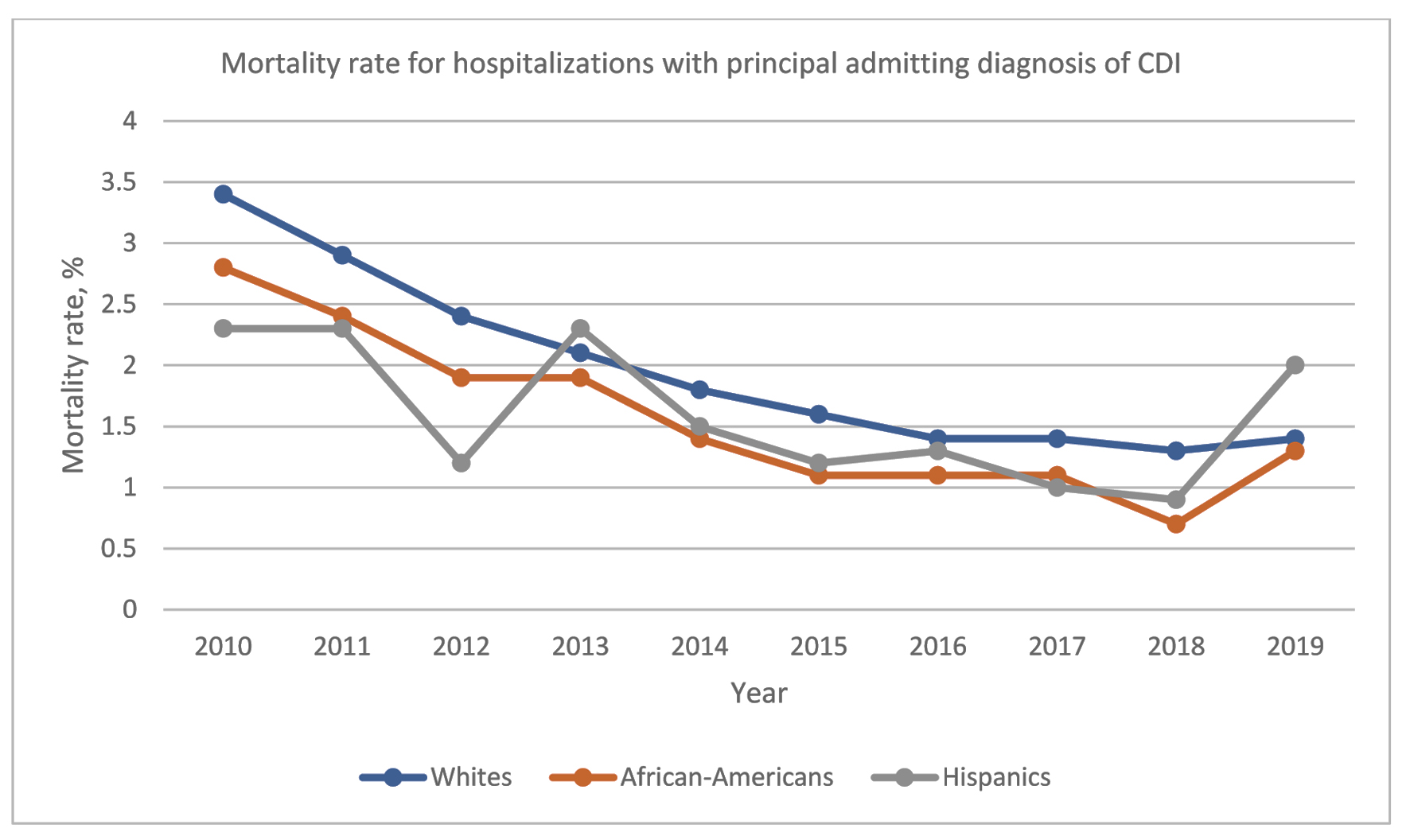 Click for large image | Figure 6. Trend in mortality rate hospitalizations with a principal admitting diagnosis of CDI (racial subgroup analysis). CDI: Clostridioides difficile infection. |
Middle-aged and elderly patients had aOR of 4.96 and 14.74 respectively for mortality when compared to young adults (P < 0.001). Females had a 21% decrease in adjusted odds of mortality compared to males over the study period (P < 0.001).
When adjusted for age and sex, there was a 0.14 annual decrease in the mean LOS in days over the study period (P < 0.001), with this finding similar across the different racial subgroups and MHOC quartiles. However, there was no significant change in the adjusted mean THC over the study period (P = 0.249).
| Discussion | ▴Top |
We analyzed the trends in CDI hospitalizations during the decade under review and found that the incidence and admission rates of CDI initially trended up, likely representing a continuation of the increasing trend in CDI incidence in the first decade of the 21st century [16-18]. After 2015, there was a marked decline in incidence and admission rates among hospitalizations with CDI. Given the transition from ICD-9 to ICD-10 codes in 2015, we ensured that the change in administrative code for the disease was accounted for. The sensitivity and specificity of these administrative codes at identifying CDI has been established at 88% and 100% respectively [19].
When the cohort of admissions with a primary diagnosis of CDI was analyzed, we found that this downward trend in incidence predated 2015 and began in 2012. This is likely explained by increased caution with antimicrobial drug use following the widespread initiation of antibiotic stewardship programs. A report by the Blue Cross Blue Shield Association in 2017 showed that the fill rate of outpatient antibiotic prescriptions declined 9% among commercially insured Americans from 2010 to 2016 with broad-spectrum antibiotic fill rates dropping the most at 13% [20]. Several studies have shown that antimicrobial stewardship programs and formulary restrictions have resulted in significant reductions in the rates of occurrence of CDI [2]. An interrupted time-series analysis conducted by Valiquette et al [21] in a secondary/tertiary-care hospital in Quebec showed that there was no significant change in nosocomial CDI incidence after strengthening of infection control procedures (P = 0.63), but the implementation of an antimicrobial stewardship program was followed by a 60% reduction in CDI incidence (P = 0.007). Similar findings were observed in two other interrupted time-series studies conducted by Fowler et al [22] and Talpaert et al [23] among acute medical admissions which showed that CDI rates fell by 65% (P = 0.009) and 66% (P < 0.0001) respectively compared to controls when “narrow-spectrum” antibiotic policies were applied.
Most of the hospitalizations for CDI in our study were among elderly patients, although the mean age of both cohorts progressively reduced while the proportion of patients with CCI scores of 3 or more increased over the study period. When adjusted for race and sex, elderly patients were found to have increased odds of hospitalizations for CDI. An older age group and multiple medical comorbidities are established risk factors for CDI [24]. Other risk factors include immunocompromised states (as seen in patients with human immunodeficiency virus infection or patients with cancer who are receiving chemotherapy), broad-spectrum antibiotic therapy (especially clindamycin, cephalosporins, amoxicillin, and fluoroquinolones), gastric acid suppression therapy, intensive care unit admission, recent non-surgical gastrointestinal procedures, and tube feeding [4, 22, 24].
We noted improvements in adjusted mortality rates and LOS amongst hospitalizations with CDI and admissions with a principal admitting diagnosis of CDI over the study period. This is likely due to new treatment strategies which were implemented over the decade under review. Between 2010 and 2019, therapeutic options including oral vancomycin, fidaxomicin, fecal microbiota transplantation, and bezlotoxumab were approved for the treatment of index episodes or recurrences of CDI and have been incorporated into clinical guidelines [25]. Another possible explanation for the improvement in mortality and LOS is the increased use of Clostridium difficile toxin polymerase chain reaction (PCR) testing assays over the study period. The rapid stool PCR test was approved by the FDA in 2011 [26] after the test was shown to have higher sensitivity and comparable specificity to the previously prevalent enzyme immunoassay [27, 28].
Elderly patients were found to have worse outcomes compared to young and middle-aged individuals. Older patients have previously been shown to be at higher risk of severe and fulminant CDI [29] which invariably have worse outcomes. This increased risk among the elderly is likely related to increased odds of comorbidities and underlying conditions that are also well-recognized risk factors for CDI [28]. Institutionalization, longer hospital stays, and infections that necessitate frequent treatment with antibiotics are more common in the elderly [2].
Females were at increased odds of CDI hospitalization but had better adjusted outcomes. Sex disparities in CDI incidence and prevalence vary across studies, but male sex has previously been associated with severe/complicated CDI [30, 31]. While the reasons behind this are unclear, it may be related to male patients being at higher odds of comorbid conditions that predispose them to CDI [32].
We also found that most hospitalizations were among White patients, but adjusted outcomes were significantly worse in ethnic minorities. Blacks and Hispanics showed significantly worse mortality outcomes, longer hospital stays, and higher total hospitalization costs compared to Whites. These are similar to findings of a retrospective analysis of the US National Hospital Discharge Surveys from 2001 to 2010 which showed that while CDI incidence was higher among White patients (7.7/1,000 discharges vs. 4.9/1,000 discharges in Blacks, P < 0.0001), the Black race was independently associated with mortality (odds ratio 1.12, 95% CI 1.09 - 1.15) and severe CDI (odds ratio 1.09, 95 % CI 1.07 - 1.11), despite being a negative predictor for hospital LOS (OR 0.93, 95 % CI 0.93 - 0.94) [33]. The reasons behind these findings are still uncertain and require further studies to elucidate. However, they may suggest socioeconomic and structural inequities disparately affecting minoritized communities including an inequitable distribution of quality healthcare, differential access to public and private insurance, and insufficient research evaluating and addressing these inequities [34].
This study has some important limitations. Firstly, the NIS uses “claims data”, and ICD-9 and ICD-10 codes were used to confirm diagnoses that may not completely match clinical/laboratory parameters. Hence our findings were dependent on appropriate data collection and correct representation of these administrative codes. Secondly, the NIS lacks laboratory or radiological data and does not appropriately grade clinical disease severity, hence we could not stratify outcomes specific to severe/fulminant CDI. Thirdly, the NIS reports data on hospitalizations rather than individual patients, hence patients with recurrent CDI infections may count as multiple admissions. Also, the sampling data from NIS do not include rehabilitation and long-term acute care hospitals which is a subset of the population that is at risk for CDI, hence that subset is not accounted for. Lastly, we were unable to determine treatment modalities and the effect of medication adherence on outcomes. Lastly, we were unable to determine treatment modalities and the effect of medication adherence on outcomes.
Conclusions
Outcomes of CDI hospitalizations improved over the studied decade, but CDI still places significant mortality and economic burden on the US health care system. Older age, male sex, and belonging to a minority racial group were associated with worse outcomes. Further studies are needed to elucidate the reasons for these findings. Continued efforts to address other established risk factors are needed for primary and secondary prevention of CDI.
Acknowledgments
None to declare.
Financial Disclosure
No external funding was received for this research.
Conflict of Interest
The authors have no current or potential conflict to declare.
Informed Consent
Not required as the study involves publicly available data from the Nationwide Inpatient Sample database.
Author Contributions
Pius Ehiremen Ojemolon drafted the manuscript, created the tables and figures, and participated in the review and final approval of the manuscript. Hafeez Shaka conceptualized the manuscript, carried out the data analysis, and participated in the review and final approval of the manuscript. Robert Kwei-Nsoro and Hisham Laswi participated in drafting the introduction and in the review and final approval of the manuscript. Ebehiwele Ebhohon, Abdultawab Shaka and Abdul-Rahman Abusalim participated in drafting the discussion and in the review and final approval of the manuscript. Benjamin Mba revised the manuscript for intellectual content and participated in the review and final approval of the manuscript.
Data Availability
Datasets are available through the HCUP central distributor on request.
| References | ▴Top |
- Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, Lynfield R, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370(13):1198-1208.
doi pubmed - Riddle DJD, Dubberke ERD. Trends in Clostridium difficile disease: epidemiology and intervention. Infect Med. 2009;26(7):211-220.
- Lessa FC, Mu Y, Bamberg WM, Beldavs ZG, Dumyati GK, Dunn JR, Farley MM, et al. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372(9):825-834.
doi pubmed - Zhang S, Palazuelos-Munoz S, Balsells EM, Nair H, Chit A, Kyaw MH. Cost of hospital management of Clostridium difficile infection in United States-a meta-analysis and modelling study. BMC Infect Dis. 2016;16(1):447.
doi pubmed - Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, Wilson LE, et al. Trends in U.S. Burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382(14):1320-1330.
doi pubmed - Turner NA, Grambow SC, Woods CW, Fowler VG, Jr., Moehring RW, Anderson DJ, Lewis SS. Epidemiologic trends in clostridioides difficile infections in a regional community hospital network. JAMA Netw Open. 2019;2(10):e1914149.
doi pubmed - Healthcare cost and utilization project. Introduction to the HCUP National Inpatient Sample (NIS). The National (Nationwide) Inpatient Sample database documentation. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2018.jsp. Accessed May 2, 2022.
- Houchens R, Ross D, Elixhauser A, Jiang J. 2014 Nationwide Inpatient Sample (NIS) Redesign Final Report. 2014. HCUP Methods Series Report # 2014-04 ONLINE. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. Accessed May 2, 2022.
- Elixhauser A, Heslin KC, Owens PL. Healthcare Cost and Utilization Project (HCUP) recommendations for reporting trends using ICD-9-CM and ICD-10-CM/PCS Data. Online. Revised July 5, 2017. U.S. Agency for Healthcare Research and Quality. Available: https://www.hcupus.ahrq.gov/datainnovations/icd10_resources.jsp. Accessed May 2, 2022.
- Sundararajan V, Quan H, Halfon P, Fushimi K, Luthi JC, Burnand B, Ghali WA, et al. Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45(12):1210-1215.
doi pubmed - Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175-196.
doi pubmed - Barrett M, Coffey R, Levit K. Population denominator data sources and data for use with the HCUP databases (Updated with 2019 Population Data). 2020 HCUP Methods Series Report # 2020-02 Online. U.S. Agency for Healthcare Research and Quality. Available: www.hcup-us.ahrq.gov/reports/methods.jsp. Accessed May 2, 2022.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335-351.
doi - Zoorob RJ, Salemi JL, Mejia de Grubb MC, Modak S, Levine RS. A nationwide study of breast cancer, depression, and multimorbidity among hospitalized women and men in the United States. Breast Cancer Res Treat. 2019;174(1):237-248.
doi pubmed - Ikedionwu CA, Dongarwar D, Williams C, Odeh E, Peh MPN, Hooker H, Wiseman S, et al. Trends and risk factors for leishmaniasis among reproductive aged women in the United States. Int J MCH AIDS. 2021;10(2):166-173.
doi pubmed - Depestel DD, Aronoff DM. Epidemiology of Clostridium difficile infection. J Pharm Pract. 2013;26(5):464-475.
doi pubmed - Zilberberg MD, Shorr AF, Kollef MH. Increase in adult Clostridium difficile-related hospitalizations and case-fatality rate, United States, 2000-2005. Emerg Infect Dis. 2008;14(6):929-931.
doi pubmed - Bossuyt P, Verhaegen J, Van Assche G, Rutgeerts P, Vermeire S. Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohns Colitis. 2009;3(1):4-7.
doi pubmed - Negron M, Barkema H, Rioux K, De Buck J, Checkley S, Beck P, Dieleman L, et al. Accuracy of ICD9 and ICD 10 codes for clostridium difficile among ulcerative colitis patients: 1264. Official Journal of the American College of Gastroenterology | ACG. 2011;106:S481.
doi - Antibiotic prescription fill rates declining in the U.S. (n.d.). Retrieved September 30, 2022. https://www.bcbs.com/the-health-of-america/reports/antibiotic-prescription-rates-declining-in-the-US.
- Valiquette L, Cossette B, Garant MP, Diab H, Pepin J. Impact of a reduction in the use of high-risk antibiotics on the course of an epidemic of Clostridium difficile-associated disease caused by the hypervirulent NAP1/027 strain. Clin Infect Dis. 2007;45(Suppl 2):S112-121.
doi pubmed - Fowler S, Webber A, Cooper BS, Phimister A, Price K, Carter Y, Kibbler CC, et al. Successful use of feedback to improve antibiotic prescribing and reduce Clostridium difficile infection: a controlled interrupted time series. J Antimicrob Chemother. 2007;59(5):990-995.
doi pubmed - Talpaert MJ, Gopal Rao G, Cooper BS, Wade P. Impact of guidelines and enhanced antibiotic stewardship on reducing broad-spectrum antibiotic usage and its effect on incidence of Clostridium difficile infection. J Antimicrob Chemother. 2011;66(9):2168-2174.
doi pubmed - Evans CT, Safdar N. Current trends in the epidemiology and outcomes of clostridium difficile infection. Clin Infect Dis. 2015;60(Suppl 2):S66-71.
doi pubmed - Johnson S, Lavergne V, Skinner AM, Gonzales-Luna AJ, Garey KW, Kelly CP, Wilcox MH. Clinical practice guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of clostridioides difficile infection in adults. Clin Infect Dis. 2021;73(5):e1029-e1044.
doi pubmed - FDA Approves Rapid C. Diff Test. 2011. https://www.medpagetoday.com/infectiousdisease/generalinfectiousdisease/25838.
- Peterson LR, Manson RU, Paule SM, Hacek DM, Robicsek A, Thomson RB, Jr., Kaul KL. Detection of toxigenic Clostridium difficile in stool samples by real-time polymerase chain reaction for the diagnosis of C. difficile-associated diarrhea. Clin Infect Dis. 2007;45(9):1152-1160.
doi pubmed - Luna RA, Boyanton BL, Jr., Mehta S, Courtney EM, Webb CR, Revell PA, Versalovic J. Rapid stool-based diagnosis of Clostridium difficile infection by real-time PCR in a children's hospital. J Clin Microbiol. 2011;49(3):851-857.
doi pubmed - Eze P, Balsells E, Kyaw MH, Nair H. Risk factors for Clostridium difficile infections - an overview of the evidence base and challenges in data synthesis. J Glob Health. 2017;7(1):010417.
doi pubmed - Tay HL, Chow A, Ng TM, Lye DC. Risk factors and treatment outcomes of severe Clostridioides difficile infection in Singapore. Sci Rep. 2019;9(1):13440.
doi pubmed - Khanafer N, Barbut F, Eckert C, Perraud M, Demont C, Luxemburger C, Vanhems P. Factors predictive of severe Clostridium difficile infection depend on the definition used. Anaerobe. 2016;37:43-48.
doi pubmed - Hopper I, Kotecha D, Chin KL, Mentz RJ, von Lueder TG. Comorbidities in heart failure: are there gender differences? Curr Heart Fail Rep. 2016;13(1):1-12.
doi pubmed - Argamany JR, Delgado A, Reveles KR. Clostridium difficile infection health disparities by race among hospitalized adults in the United States, 2001 to 2010. BMC Infect Dis. 2016;16(1):454.
doi pubmed - Chen J, Khazanchi R, Bearman G, Marcelin JR. Racial/Ethnic Inequities in Healthcare-associated Infections Under the Shadow of Structural Racism: Narrative Review and Call to Action. Curr Infect Dis Rep. 2021;23(10):17.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


