| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Short Communication
Volume 14, Number 9, September 2022, pages 388-393
Prescribing Patterns for Long-Acting Inhaled Bronchodilators Among Rural Adults With Chronic Obstructive Pulmonary Disease
Wendy M. Brunnera, c , Nadir Siddiquib, Melissa B. Scribania, Nicole L. Krupaa, Erik Riesenfeldb
aResearch Institute, Bassett Medical Center, Cooperstown, NY, USA
bBassett Medical Center, Cooperstown, NY, USA
cCorresponding Author: Wendy Brunner, Research Institute, Bassett Medical Center, Cooperstown, NY 13326, USA
Manuscript submitted July 6, 2022, accepted August 5, 2022, published online September 29, 2022
Short title: Long-Acting Inhaled Bronchodilators for COPD
doi: https://doi.org/10.14740/jocmr4786
| Abstract | ▴Top |
Background: Chronic obstructive pulmonary disease (COPD) is prevalent in rural areas of the USA. Long-acting inhaled bronchodilators (LABDs) are a key tool in COPD management and are underutilized. The purpose of this study was to determine whether rates of prescriptions for LABD differed by payer among patients with COPD in a rural healthcare network.
Methods: In analysis 1, a random sample of patients with spirometry- and symptom-confirmed COPD over April 1, 2017 to December 31, 2019 was identified. Patient characteristics, including payer status, extracted from medical records were compared for those who did and did not have any prescriptions for LABD during the study window. In analysis 2, patients with one or more COPD-related hospitalizations during the same time period were identified and similar comparisons were made by LABD prescription status.
Results: Among a random sample of patients with spirometry-confirmed COPD, 93.0% had been prescribed LABD during the study window with no difference in proportion by payer. Among the 461 patients with a COPD-related hospitalization, 388 (84.2%) had been prescribed LABD, again with no difference in prescriptions by payer. Those with a COPD-related hospitalization who had been prescribed LABD were younger, had lower body mass index, were more likely to be current smokers and had higher rates of hospitalizations for COPD during the study period than those not prescribed LABD.
Conclusion: While disparities in LABD utilization may occur due to cost or other barriers to filling prescriptions, in our study, prescriptions for LABD were common and did not differ by payer status.
Keywords: Long-acting antimuscarinics; Long-acting beta2-agonists; Prescriptions; Rural; Payer
| Introduction | ▴Top |
Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of death in United States [1]. The prevalence of COPD is higher among adults living in rural compared with nonrural areas in the USA [2-4]. According to the National Health Interview Survey, 8.4% of US adults have COPD. Among rural adults, the prevalence of COPD is 12.7% and among rural residents experiencing poverty, the prevalence rises to 15.7% [5]. In addition to higher prevalence, rural adults experience a higher frequency of COPD exacerbations and mortality [6, 7]. Challenges to COPD management in rural areas include the lack of pulmonary disease specialists and longer distances to care [3]. Long-acting antimuscarinics (LAMAs) and long-acting beta2-agonists (LABAs) are long-acting inhaled bronchodilators (LABDs) that can be used alone or in combination with each other or with inhaled steroids [8]. LABDs are important in the treatment of COPD as they have been demonstrated to decrease exacerbations which can be common and costly and impact quality of life for people with COPD [9]. Guidance provided by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) initiates patients on LABD after assessing stage and severity of COPD using the ABCD assessment scheme and starts LABD if there has been more than one COPD exacerbation leading to hospitalization irrespective of symptom burden, as measured by the modified Medical Research Council Dyspnea Scale (mMRC) [8, 10]. The purpose of this study was to determine whether the proportion of COPD patients in a rural healthcare network prescribed LABD differed by payer. This question arose in part out of an observation by the authors that participants in a pilot COPD self-management education program for Medicaid enrollees were less likely to have heard about LABD, in contrast with participants in COPD support groups who were largely Medicare enrollees.
| Materials and Methods | ▴Top |
Design
This study was designed as a retrospective chart review of patients with COPD in a rural healthcare network. The network covers an eight-county region in central upstate New York in which seven of the eight counties served meet the US Federal Office of Rural Health Policy’s definition of rural. The study period ran from April 1, 2017 (the date at which billing through the network’s electronic medical record (EMR) system began that made it easier to accurately identify payer information) through December 31, 2019 (to exclude changes in health care utilization patterns related to the coronavirus disease 2019 (COVID-19) pandemic). We conducted two analyses using different definitions of COPD: spirometry-confirmed and hospitalization-based. Figure 1 shows flow diagrams depicting the two analyses that comprised our study. The outcome of interest was having ever versus never been prescribed a long-acting inhaled bronchodilator (LAMA or LABA) during the study period. Patients with exceptions for use of LABD were excluded from this study.
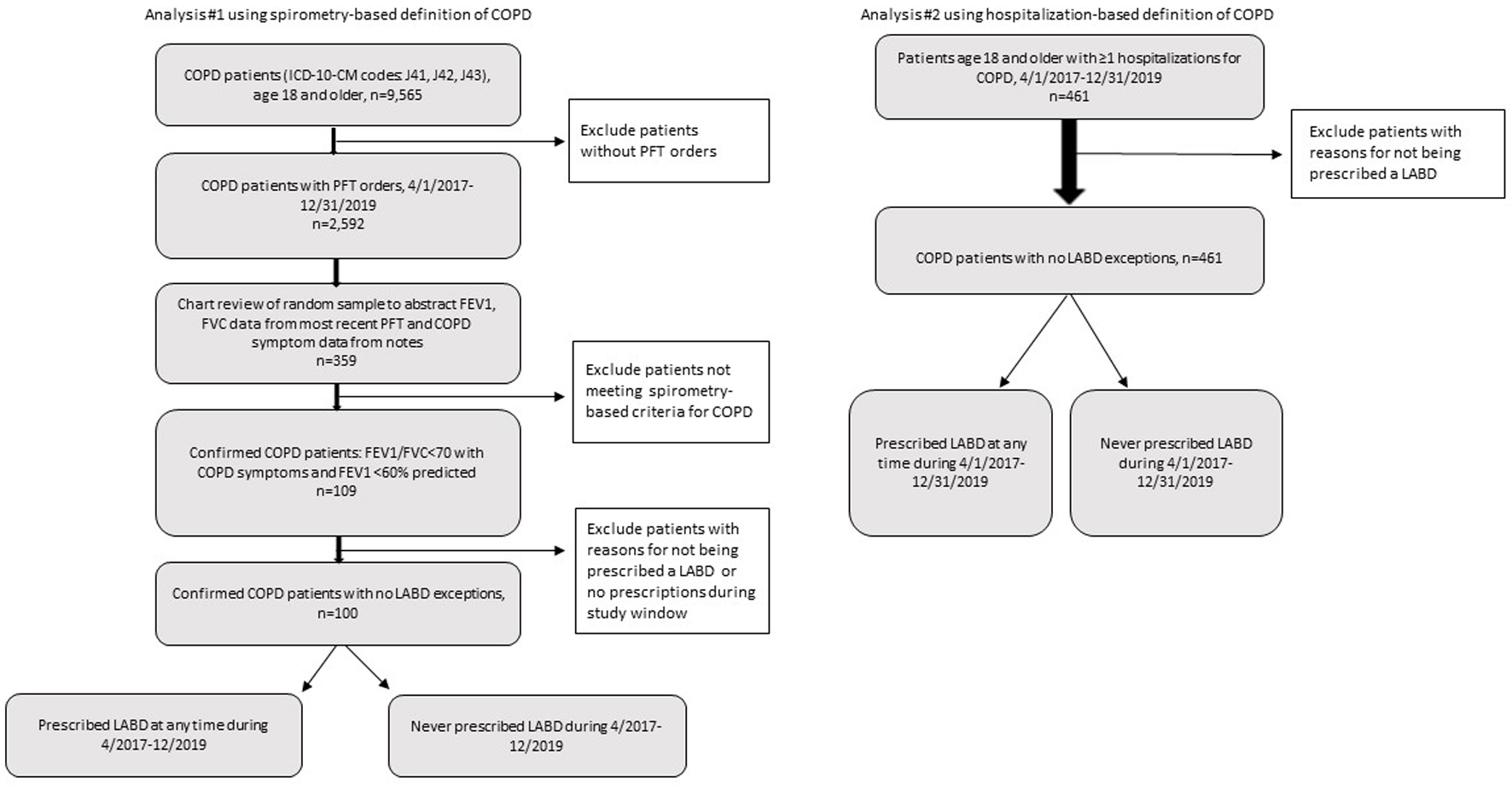 Click for large image | Figure 1. Study flow diagrams. The arrows depict the study flow for the two separate analyses. |
Participants and procedure
In the first analysis, we examined prescriptions for LABD among patients with spirometry-confirmed COPD. This definition was based on the National Quality Forum measure #0102: Chronic Obstructive Pulmonary Disease (COPD): Long-Acting Inhaled Bronchodilator Therapy [11]. First, we identified patients aged 18 or older with possible COPD using International Classification of Disease Clinical Modification version 10 (ICD-10-CM) codes: J41.x, J42.x, J43.x, and J44.x. Within this group, we identified patients with spirometry-confirmed COPD using the following definition: forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) < 70 with documented COPD symptoms (dyspnea, cough, and wheezing) and FEV1 < 60% predicted and no contraindications for LABD use. Because spirometry data were not accessible through a query in the EMR system, we conducted a manual chart review on a random sample of patients who had had spirometry done during the study period. To do this, we generated a random number list to select patients based on medical record number. In addition to excluding patients not meeting the spirometry-confirmed COPD definition, we excluded patients who had no prescriptions during the study period. When a patient was not eligible, the reviewer (NS) moved on to the next record on the random number list. We continued reviews until reaching 100 eligible patients. The chart review involved abstracting spirometry values, COPD symptoms and exceptions for LABD use and source of COPD care (primary care, pulmonology, emergency department (ED), other, and unknown). In the second analysis, we examined prescriptions for LABD among patients who had one or more COPD-related hospitalizations between April 1, 2017 and December 31, 2019 (putting them in GOLD’s C and D categories) [8, 10]. COPD-related hospitalizations were identified as those for which COPD was the primary diagnosis (ICD-10-CM codes: J41.x, J42.x, J43.x, and J44.x). We also conducted a chart review of records for the hospitalized patients who had no prescriptions for LABD to identify contraindications for use of LABD. For both analyses, we collected the following information from the medical records (as recorded at the time of the order for pulmonary function testing for analysis #1 or at the time of hospitalization for analysis #2): demographics (age, sex, and race/ethnicity), body mass index (BMI), payer (Medicare, Medicaid, dual eligible, private, and uninsured), smoking history (never, current, and former), and ED visits or hospitalizations where COPD was the primary diagnosis (predictor of future exacerbations).
Statistical analysis
Comparisons of patient characteristics between those prescribed LABD and those not prescribed LABD were carried out using Chi-square analysis (or Fisher’s exact test as appropriate) for categorical variables and using the Student’s t-test for continuous variables. For analysis 2 only, the incidence density for COPD hospitalizations (the number of COPD-related hospitalizations divided by the total patient time at risk, in days) was calculated for patients who had been prescribed LABD and for those who had not. The rate ratio was calculated by dividing the incidence density for those prescribed LABD by the incidence density for those not prescribed LABD. Incidence densities were compared by LABD status (yes/no) using the two-sample test for incidence rates [12]. Statistical analysis was conducted using SAS 9.4 (Cary, NC). Statistical significance was defined as P < 0.05. Prior to the researchers obtaining patient medical records, the Mary Imogene Bassett Institutional Review Board (IRB) reviewed the study protocol and determined that this study was exempt from IRB review under 45 CFR 46.104 (d)(4)(ii), “secondary research for which consent is not required” in which data are recorded in a way that human subjects cannot readily be identified, the subjects are not contacted by the project team, and the subjects will not be re-identified. Thus, patient consent for review of medical records was not required.
| Results | ▴Top |
Analysis 1
Among the sample of 100 patients with spirometry-confirmed COPD, there was no difference in the likelihood of being prescribed LABD by insurance payer. Ninety-three (93.0%) had been prescribed LABD during the study period and seven had not (7.0%). More than 90% of subjects obtained COPD care within the primary care system of the network. There were no differences in likelihood of being prescribed LABD with respect to patient age, sex, or smoking history (Table 1). Those with no prescription for LABD had higher BMI than those that were prescribed LABD, but this difference did not reach statistical significance in this limited sample.
 Click to view | Table 1. Characteristics of Patients With Confirmed COPD by LABD Prescription Status (N = 100) |
Analysis 2
Among the 461 subjects hospitalized for COPD during the study period, insurance payer was not associated with LABD prescription. Three hundred eighty-eight (388, 84.2%) had been prescribed LABD and 73 (15.8%) had not (Table 2). Those who were prescribed LABD during the study period were significantly younger on average and had lower BMI than those not prescribed LABD. A greater proportion of those prescribed LABD were current smokers versus those not prescribed LABD. Patient sex was not associated with LABD prescription. Those prescribed LABD had a significantly higher rate of COPD-related hospitalizations during the study period than those without a prescription for LABD. Upon further chart review for analysis 2, it was determined that 41 (56%) of the 73 COPD patients who had been hospitalized and had no prescriptions for LABD during the study window had evidence of use of LABD in their medical records (listed as historical medications). Two (3.4%) were prescribed in 2020 and one (1.4%) did not have COPD. Twenty-nine (39.7%) of the 73, or 6.3% (29/461) of all of the COPD patients who had been hospitalized neither had a prescription for an LABD nor evidence of taking an LABD.
 Click to view | Table 2. Characteristics of Patients Hospitalized for COPD During the Study Period by LABD Prescription Status (N = 461) |
| Discussion | ▴Top |
Undertreatment of COPD is common among both commercial and Medicare enrollees [13] with only 30-35% of COPD patients being prescribed maintenance medications [9]. In a survey of COPD patients, 66% of those on commercial insurance and 71% on Medicare Advantage had not been prescribed any long-acting medication [9]. Among patients with advanced COPD, those figures dropped to 59% and 69%, respectively [9]. A recent Canadian study of prescription patterns for COPD found overprescribing of inhaled corticosteroids and underprescribing of LABD [14]. In contrast, our analyses showed a very high proportion of COPD patients having ever received a prescription for LABD during the study period for both spirometry-based and hospitalization-based definitions of COPD. These results precluded a more in-depth examination of our original question, i.e., whether prescription patterns for LABD differed by payer. We suspect that the results from our first analysis might have been biased as the inclusion criteria were based in part on spirometry. That is, patients with pulmonary function testing data in their medical records may be more likely to have been prescribed LABD. The second analysis was intended to address that bias by including all patients with a COPD-related hospitalization whether or not there were spirometry data to confirm the diagnosis. Because our study was limited to examining medical records, not claims data, we were only able to look at patterns of prescriptions, not prescription fills. However, studying the proportion of those prescriptions that were filled may indeed provide a different picture as the financial costs of medications for COPD are high. Among adults with Medicare Part D coverage, the projected annual out-of-pocket monthly cost for a single inhaler is at least $900 [15]. Among the 60% of COPD patients with 2 - 3 exacerbations per year, the costs of treatment for COPD nearly doubled [16]. Nearly one-third of adults with COPD enrolled in Medicare reported that they did not fill prescriptions for COPD inhalers due to cost [17]. Adults with COPD are more likely than those with other chronic conditions to experience housing and food insecurity and those factors are in turn tied to an increased likelihood of experiencing economic barriers to accessing health care [18]. Thus, while the percentage of COPD patients in our rural network who received prescriptions for LABD was high, that is not necessarily an indication of LABD use, although, receiving a prescription for LABD is a necessary step. For this reason, this study was intended to be a first step in understanding barriers to the management of COPD and prevention of COPD exacerbations in a rural healthcare network.
Previous studies using prescription claims data have reported low rates of LABD use. In a study of adults hospitalized for COPD, including those with commercial insurance (aged 40 and older) or Medicare (aged 65 and older), Baker et al found that prescription fills for LABD were 41% in the 90 days prior and 57% in the 180-day post-hospitalization period [19]. In a study of Medicare Advantage plan members (aged 65 and older) with COPD, Xu et al also found a low rate of prescription fills for LABD (12%); however, they found that LABD prescription fills did increase following hospitalization [20]. The authors point to the need for future research to better understand why such a high proportion of COPD patients are not filling prescriptions for LABD [20].
Limitations
As with lack of access to data on prescription fills, we were not able to assess the prescription data in terms of cumulative doses to determine if they were consistent with ongoing guidelines-based pharmaceutical treatment. That is, we could not assess whether the number of prescriptions for a particular patient was sufficient over a certain time period to indicate daily use. Additionally, because the spirometry data were only accessible through manual chart review, we were limited to studying a random sample of 100 patients in the first analysis, which limited our statistical power. We were also limited in not being able to include non-hospitalized patients with COPD who did not have pulmonary function testing data that would allow us to validate their diagnosis.
Conclusion
Prescriptions for LABD among COPD patients in a rural healthcare network were common and did not appear to differ by payer status. Further work is needed to assess other potential barriers to utilization of LABDs among patients with COPD.
Acknowledgments
An abstract based on this manuscript was accepted for presentation as a poster at the American Thoracic Society annual meeting in May 2022.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
Wendy Brunner: conceptualization, writing - original draft, writing - review and editing. Nadir Siddiqui: conceptualization, data curation, writing - reviewing and editing. Melissa Scribani: formal analysis, writing - review and editing. Nicole Krupa: data curation, formal analysis, writing - review and editing. Erik Riesenfeld: conceptualization, writing - review and editing.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Zarrabian B, Mirsaeidi M. A trend analysis of chronic obstructive pulmonary disease mortality in the United States by race and sex. Ann Am Thorac Soc. 2021;18(7):1138-1146.
doi pubmed - Gaffney AW, Hawks L, White AC, Woolhandler S, Himmelstein D, Christiani DC, McCormick D. Health care disparities across the urban-rural divide: a national study of individuals with COPD. J Rural Health. 2022;38(1):207-216.
doi pubmed - Moore P, Atkins GT, Cramb S, Croft JB, Davis L, Dolor RJ, Doyle D, et al. COPD and rural health: a dialogue on the national action plan. J Rural Health. 2019;35(4):424-428.
doi pubmed - Mushtaq A. COPD and rural health in the USA. Lancet Respir Med. 2018;6(5):330-331.
doi - Raju S, Keet CA, Paulin LM, Matsui EC, Peng RD, Hansel NN, McCormack MC. Rural residence and poverty are independent risk factors for chronic obstructive pulmonary disease in the United States. Am J Respir Crit Care Med. 2019;199(8):961-969.
doi pubmed - Burkes RM, Gassett AJ, Ceppe AS, Anderson W, O'Neal WK, Woodruff PG, Krishnan JA, et al. Rural residence and chronic obstructive pulmonary disease exacerbations. analysis of the SPIROMICS cohort. Ann Am Thorac Soc. 2018;15(7):808-816.
doi pubmed - Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, Cunningham TJ, et al. Urban-rural county and state differences in chronic obstructive pulmonary disease - United States, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(7):205-211.
doi pubmed - GOLD. Global strategy for the diagnosis, management and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2022 Report. 2022. https://goldcopd.org.
- Blanchette CM, Gross NJ, Altman P. Rising costs of COPD and the potential for maintenance therapy to slow the trend. Am Health Drug Benefits. 2014;7(2):98-106.
- Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD guidelines: a review of the 2018 GOLD report. Mayo Clin Proc. 2018;93(10):1488-1502.
doi pubmed - US Quality Payment Program. Chronic obstructive pulmonary disease (COPD): long-acting inhaled bronchodilator therapy. Quality ID #52,. Accessed June 8, 2021, https://qpp.cms.gov/docs/QPP_quality_measure_specifications/CQM-Measures/2020_Measure_052_MIPSCQM.pdf.
- Rosner M. Fundamentals of Biostatistics. 7th ed. Brooks/Cole; 2010.
- Make B, Dutro MP, Paulose-Ram R, Marton JP, Mapel DW. Undertreatment of COPD: a retrospective analysis of US managed care and Medicare patients. Int J Chron Obstruct Pulmon Dis. 2012;7:1-9.
doi pubmed - Bahremand T, Etminan M, Roshan-Moniri N, De Vera MA, Tavakoli H, Sadatsafavi M. Are COPD prescription patterns aligned with guidelines? Evidence from a canadian population-based study. Int J Chron Obstruct Pulmon Dis. 2021;16:751-759.
doi pubmed - Tseng CW, Yazdany J, Dudley RA, DeJong C, Kazi DS, Chen R, Lin GA. Medicare part D plans' coverage and cost-sharing for acute rescue and preventive inhalers for chronic obstructive pulmonary disease. JAMA Intern Med. 2017;177(4):585-588.
doi pubmed - Milewska A, Rysiak E, Zareba I, Holownia A, Mroz RM. Costs of Treatment of Chronic Obstructive Pulmonary Disease. Adv Exp Med Biol. 2016;885:67-75.
doi pubmed - Castaldi PJ, Rogers WH, Safran DG, Wilson IB. Inhaler costs and medication nonadherence among seniors with chronic pulmonary disease. Chest. 2010;138(3):614-620.
doi pubmed - Charkhchi P, Fazeli Dehkordy S, Carlos RC. Housing and food insecurity, care access, and health status among the chronically ill: an analysis of the behavioral risk factor surveillance system. J Gen Intern Med. 2018;33(5):644-650.
doi pubmed - Baker CL, Zou KH, Su J. Long-acting bronchodilator use after hospitalization for COPD: an observational study of health insurance claims data. Int J Chron Obstruct Pulmon Dis. 2014;9:431-439.
doi pubmed - Xu Q, Laxa SS, Serna O, Sansgiry SS. Medication use before and after hospitalization for chronic obstructive pulmonary disease in a cohort of elderly patients with a medicare advantage plan. Am Health Drug Benefits. 2020;13(1):32-42.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


