| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 8, August 2022, pages 293-299
Prevalence and Impact of Acute Pancreatitis on Hospitalization Outcomes in a Cohort of Patients With Crohn’s Disease
Ahmed Abomhyaa, g , Elizabeth Clemetsonb, Farrah Khana, Omar Tageldinc, Zainab Abdulsadad, Hossam Hamade, Vijay Gayamf, Denzil Etiennef
aDepartment of Internal Medicine, The Brooklyn Hospital Center, NY, USA
bSt. Georges University School of Medicine, West Indies, Grenada
cGastroenterology Department, Albany Medical Center, NY, USA
dMeharry Medical College School of Medicine, Nashville, TN, USA
eFaculty of Medicine, Al-Azhar University, Cairo, Egypt
fGastroenterology Department, The Brooklyn Hospital Center, NY, USA
gCorresponding Author: Ahmed Abomhya, Department of Internal Medicine, The Brooklyn Hospital Center, NY, USA
Manuscript submitted June 8, 2022, accepted August 8, 2022, published online August 27, 2022
Short title: Acute Pancreatitis in CD Patients
doi: https://doi.org/10.14740/jocmr4761
| Abstract | ▴Top |
Background: Few studies evaluated the risk of acute pancreatitis (AP) in patients with Crohn’s disease (CD). It’s controversial if AP can be considered as an extraintestinal manifestation of CD. We studied this potential association in a retrospective cohort of patients with CD.
Methods: We draw our cohort from the Nationwide Readmission Databases 2016 - 2018. We used the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes to identify all adult patients admitted with a diagnosis of CD. Patient with a comorbid AP were identified. We analyzed the significant impact of AP on hospitalization outcomes. A multivariate regression analysis was used to identify factors associated with AP.
Results: We included 214,622 patients discharged from an index hospitalization for CD, 1.1% had AP. AP was independently associated with higher odds of inpatient mortality (odds ratio (OR): 1.831; 95% confidence interval (CI): 1.345 - 2.492, P < 0.001), gallstone disease (OR: 4.047; 95% CI: 3.343 - 4.9, P < 0.001), nonalcoholic fatty liver disease (NAFLD) (OR: 3.568; 95% CI: 3.08 - 4.133, P < 0.001), and hypercalcemia (OR: 1.964; 95% CI: 1.302 - 2.965, P = 0.001). Thirty-day readmission analysis showed that CD patients with AP were more commonly to be readmitted for AP than for any other reason.
Conclusions: In our nationwide cohort of CD patients, there was a significant association between AP and worse hospitalization outcomes. Additionally, we found independent associations for having AP that may help identify patients at high risk.
Keywords: Acute pancreatitis; Crohn’s disease; Gallstones; Hypercalcemia; Chronic pancreatitis
| Introduction | ▴Top |
Acute pancreatitis is an inflammation of the pancreas that varies in severity but is usually associated with significant morbidity [1]. It is the most common gastrointestinal cause of hospital admissions in the USA, with over 270,000 hospital admission and up to $2.6 billion per year in cost [2, 3]. Crohn’s disease (CD) is a chronic transmural inflammation that can affect the entire gastrointestinal tract with relapsing and remitting symptoms and has been associated with multiple extraintestinal manifestations (EIMs). CD is more prevalent in developed countries with the USA having one of the highest prevalence worldwide at 214 per 100,000 [4].
While the intestine is the most commonly involved organ in patients with CD, inflammation can occur outside the intestine [5]. Specific EIMs that are known to occur with CD include arthritis, spondylitis, sacroiliitis, primary sclerosing cholangitis, uveitis, erythema nodosum, and pyoderma gangrenosum [6].
Whether acute pancreatitis can be considered an extraintestinal manifestation of CD or not, remains a controversial topic [7-9]. Mucin-1 (MUC-1) is expressed in an abnormal, hyperglycosylated form on the colonic epithelium of humans with inflammatory bowel disease (IBD) and contributes to inflammation. Animal studies have shown the migration of MUC-1 specific T cells to the colon and pancreas of IBD patients, suggesting potential susceptibility to a T cell-mediated injury of the pancreas [10]. One-third of patients with CD have antibodies against pancreatic juice, which may contribute to the development of acute pancreatitis. Some studies showed that patients with CD have a four-fold increase in the risk of developing acute pancreatitis compared to patients without CD [7].
Previous studies have shown that CD patients tend to have an increased risk of gallstones compared to patients without CD, with a reported prevalence of gallstones in CD ranging from 13% to 34% based on data from recent studies [11-13]. Weersma et al showed that the occurrence of acute pancreatitis in CD patients who are taking azathioprine (AZA) is significantly increased compared to patients taking AZA for other autoimmune conditions like systemic lupus erythematosus [14].
Recent studies showed that IBD patients have a three-fold higher health care cost than patients without IBD. Some of the biggest cost drivers include anemia, mental health disorders, chronic steroid or opioid use, emergency department (ED) visits, and nonelective readmissions [15].
This is the first study to evaluate the burden and associated outcomes of acute pancreatitis in a large nationwide cohort of CD patients. We, therefore, aimed to estimate the prevalence of acute pancreatitis among patients with CD, and demographic and clinical factors associated with acute pancreatitis in this patient population. We also evaluated hospitalization outcomes including inpatient mortality, costs of hospitalizations, hospital length of stay (LOS), and readmission rates.
| Materials and Methods | ▴Top |
Data source and study design
We utilized the Healthcare Cost and Utilization Project (HCUP) Nationwide Readmissions Database (NRD) which is drawn from HCUP State Inpatient Databases (SID) and contains verified patient linkage numbers that can be used to track a person’s hospitalizations within a state while adhering to strict privacy guidelines [16]. This is a retrospective cohort study of patients discharged with a diagnosis of CD between 2016 and 2018. The study was performed in accordance with the 1963 Helsinki Declaration and is exempt from an Institutional Review Board due to the lack of any identifying patient information [17, 18].
Study population and groups
Inclusion criteria: NRD records between 2016 and 2018 with discharge diagnosis of CD. We excluded patients younger than 18 years old and records with missing information. We used the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes to identify diagnoses of interest.
CD patients with a comorbid diagnosis of acute pancreatitis were identified. We compared CD patients with and without acute pancreatitis. Before comparing CD patients with and without acute pancreatitis, we first excluded those with chronic pancreatitis (Fig. 1).
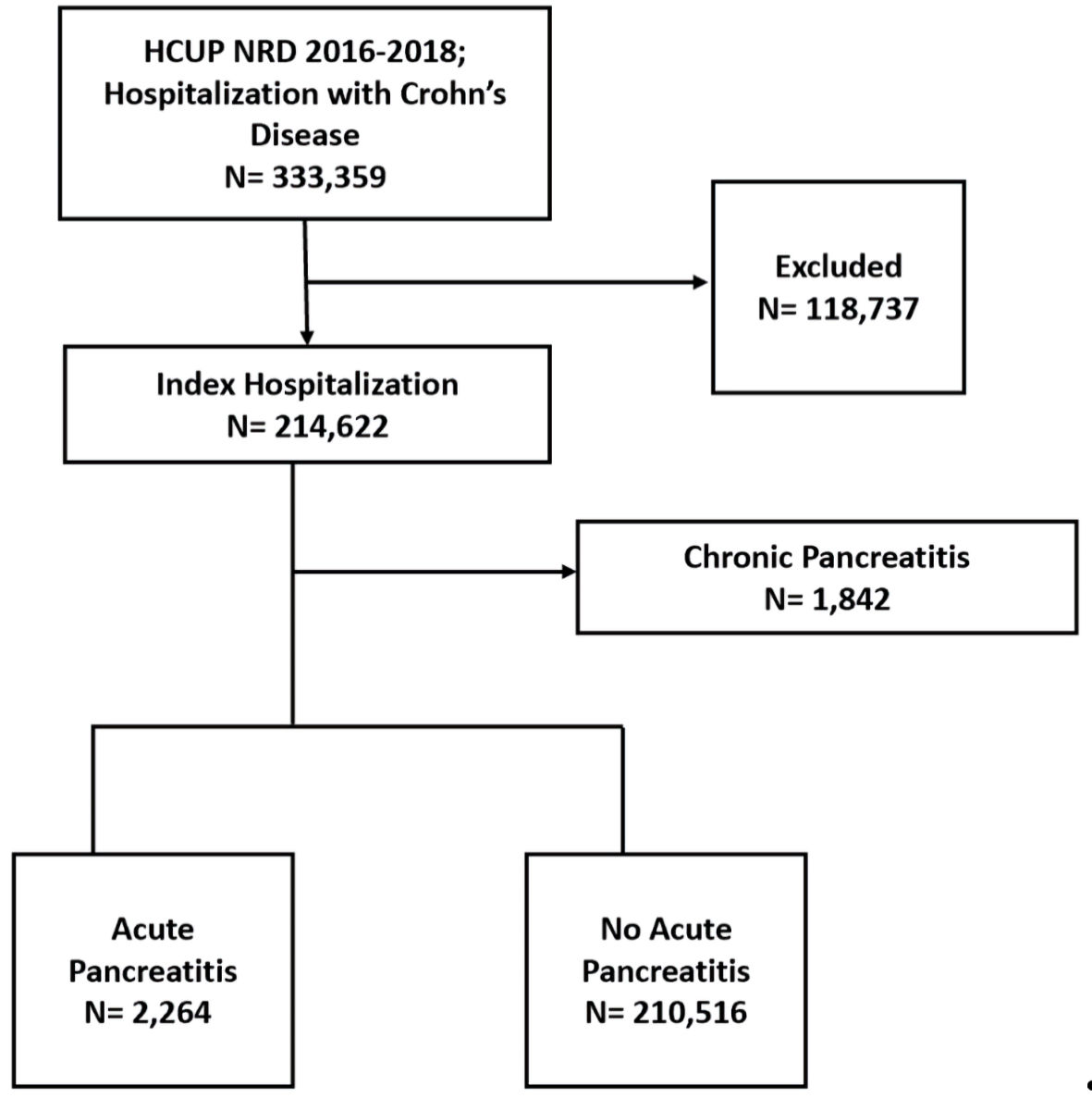 Click for large image | Figure 1. Case selection flowchart. HCUP: the Healthcare Cost and Utilization Project; NRD: Nationwide Readmissions Database. |
Study variables
We collected data on age, gender, income status, hospitals’ bed size, and insurance. NRD categorizes income status into four groups according to the average household income of the zip code where the patient lives. Comorbid conditions of interest were identified using ICD-10-CM codes (Supplementary Material 1, www.jocmr.org). Index hospitalization discharges occurring in the month of December were excluded from the 30-day readmission analysis. Elective readmissions and patients who died in the index hospitalization were excluded from the readmission analysis.
Our primary outcomes were the prevalence of acute pancreatitis among patients with CD and the factors independently associated with having acute pancreatitis in this patient population. Secondary outcomes included inpatient mortality, the LOS, all-cause 30-day nonelective readmission rate, and total cost of hospitalization. We calculated the rates for the most common causes of 30-day nonelective readmission.
Statistical analysis
We extracted and analyzed the data using SPSS Version 25 (IBM Corporation, Armonk, NY, USA). Median and interquartile ranges (IQR) were used to summarize numeric variables (not normally distributed) and then compared using the Mann-Whitney test. Categorical variables were summarized with percentages and compared using the Pearson χ2 test. The factors that were significant in univariate analyses at P < 0.05 were included in the multivariate regression analysis to estimate the odds ratio (OR) and 95% confidence interval (CI) for factors associated with acute pancreatitis among patients with CD. We also used multivariate regression analysis to evaluate the effect of acute pancreatitis on inpatient mortality. A P value < 0.05 was considered statistically significant.
| Results | ▴Top |
Demographic and clinical characteristics of CD patients with and without acute pancreatitis
We extracted 333,359 hospital discharge records with a diagnosis of CD. We excluded records with missing information or age < 18. We analyzed 214,622 index hospital discharges with CD, of whom 2,264 (1.1%) patients had acute pancreatitis, and 1,842 (0.9%) patients had chronic pancreatitis.
CD patients with acute pancreatitis were younger (51; IQR: 38 - 64 vs. 53; IQR: 36 - 68, P = 0.003) compared to CD patients without acute pancreatitis. CD patients with acute pancreatitis were more commonly to belong to the lowest income category (25.5% vs. 23.2%, P = 0.015) and less commonly to the highest income category (21.4% vs. 23.7%, P = 0.015) compared to CD patients without acute pancreatitis.
CD patients with acute pancreatitis had higher prevalence of hypertension (34.2% vs. 30%, P < 0.001), diabetes mellitus (18.7% vs. 15.4%, P < 0.001), and obesity (13.7% vs. 11.8%, P = 0.005) compared to CD patients without acute pancreatitis. CD patients with acute pancreatitis were more commonly to have gallstone disease (5.3% vs. 1.2%, P > 0.001) and nonalcoholic fatty liver disease (NAFLD) (9.6% vs. 2.3%, P < 0.001) compared to CD patients without acute pancreatitis. Demographic and clinical characteristics of CD patients with and without acute pancreatitis are summarized in Table 1.
 Click to view | Table 1. Demographic and Clinical Characteristics of Crohn’s Disease Patients With and Without Acute Pancreatitis |
Of CD patients with acute pancreatitis, 360 (15.9%) had biliary acute pancreatitis and 252 (11.1%) had alcohol-induced acute pancreatitis. The etiology of acute pancreatitis among patients with CD is summarized in Table 2.
 Click to view | Table 2. Etiology of Acute Pancreatitis in Patients With Crohn’s Disease |
Hospitalization outcomes for CD patients with and without acute pancreatitis
CD patients with acute pancreatitis had higher inpatient mortality (1.9% vs. 1.2%, P = 0.002) and increased median LOS (4; IQR: 2 - 6 vs. 3; IQR: 2 - 6, P < 0.001) compared to CD patients without acute pancreatitis. After adjusting for sex, age, insurance type, hospital bed size, and comorbid conditions, acute pancreatitis was associated with increased odds of inpatient mortality (hazard ratio (HR): 1.831; 95% CI: 1.345 - 2.492, P < 0.001).
There was no significant difference in median total charges ($29,562; IQR: $16,593 - $58,424 vs. $30,803; IQR: $16,884 - $58,708, P = 0.418) between CD patients with and without acute pancreatitis, respectively. There was no significant difference in all-cause 30-day nonelective readmission rate (9.7% vs. 9.9%, P = 0.709) between CD patients with and without acute pancreatitis, respectively. CD patients with chronic pancreatitis had a statistically significant higher rate of all-cause 30-day nonelective readmissions (15.7% vs. 9.9%, P < 0.001) compared to CD patients without chronic pancreatitis.
The most common cause of 30-day nonelective readmission among CD patients with acute pancreatitis was another episode of acute pancreatitis. CD flare, sepsis, acute kidney failure, and Clostridium difficile enterocolitis were among the most common causes of 30-day readmission in CD patients with acute pancreatitis (Table 3).
 Click to view | Table 3. Most Common Causes of 30-Day Nonelective Readmission Among CD Patients With Acute Pancreatitis |
Multivariate analysis for factors associated with acute pancreatitis in patients with CD
Multivariate analysis demonstrated that gallstone disease (OR: 4.047; 95% CI: 3.343 - 4.9, P < 0.001), NAFLD (OR: 3.568; 95% CI: 3.08 - 4.133, P < 0.001), and hypercalcemia (OR: 1.964; 95% CI: 1.302 - 2.965, P = 0.001) had increased odds of having acute pancreatitis. Age ≥ 65 was associated with decreased odds of having acute pancreatitis (OR: 0.639; 95% CI: 0.567 - 0.72, P < 0.001).
Hepatic failure (OR: 1.505; 95% CI: 1.086 - 2.086, P = 0.014), acute kidney failure (OR: 1.288: 95% CI: 1.149 - 1.444, P < 0.001), and thrombocytopenia (OR:1.236; 95% CI: 1.024 - 1.49, P = 0.031) were independently associated with acute pancreatitis (Table 4).
 Click to view | Table 4. Multivariate Analysis for Factors Associated With Acute Pancreatitis in Patients With Crohn’s Disease |
| Discussion | ▴Top |
There are few studies to evaluate an association between acute pancreatitis and CD. Our study is significant as we used a nationally representative database to study the association between acute pancreatitis and CD.
The reported incidence of acute pancreatitis in the USA ranges around 43.8 cases per 100,000 adults [19]. In our cohort, 1.1% (1,100 per 100,000) of hospitalized CD patients had acute pancreatitis, and 0.9% had chronic pancreatitis. While our study cohort included only hospitalized CD patients, the observed high prevalence of acute pancreatitis supports the studies suggesting an increased risk of developing acute pancreatitis in patients with CD [7-9]. Even after adjusting for sex, age, insurance type, hospital bed size, and comorbid conditions, our study showed that patients with CD and acute pancreatitis had increased odds of in-hospital mortality compared to CD patients without acute pancreatitis.
CD patients with acute pancreatitis were younger than CD patients without acute pancreatitis. An age ≥ 65 years was associated with lower odds of having acute pancreatitis. There was no significant difference in the distribution of gender between the two groups, although patients in both groups were more commonly females; this supports previous studies from Europe that showed a similar risk of developing acute pancreatitis in both genders [8].
Gallstone disease, alcoholism, medications, and postoperative complications are among the most commonly suggested etiologies for acute pancreatitis in patients with CD [5, 20, 21]. In our study, patients with acute pancreatitis had a higher prevalence of gallstone disease, and the presence of gallstones was associated with a greater than four-fold increased odds of having acute pancreatitis. After a gallstone pancreatitis episode, it is recommended to perform a cholecystectomy as soon as possible to eliminate the risk of future attacks [3]. Given the significantly higher odds of developing acute pancreatitis and the associated morbidity and mortality, further prospective studies would be needed to estimate the benefits of closer monitoring and elective management of gallstone disease in patients with CD.
Liver diseases of various etiologies have been associated with risk of acute pancreatitis [10, 22]. We found that NAFLD was independently associated with acute pancreatitis in hospitalized CD patients. Hepatic failure and acute kidney failure were independently associated with acute pancreatitis. Acute kidney failure is a common complication of severe acute pancreatitis and is associated with a poor prognosis [23].
Hypercalcemia is associated with acute pancreatitis in patients with breast cancer, multiple myeloma, or primary hyperparathyroidism [24, 25]. Our data showed that hypercalcemia was independently associated with increased odds of having acute pancreatitis in patients with CD. We also showed an independent association between acute pancreatitis and thrombocytopenia, an observation that has been suggested by previous studies [26].
Preventable nonelective readmissions possess a significant burden on the healthcare system. Readmission analysis showed that having another episode of acute pancreatitis was the most common cause for nonelective 30-day readmission in CD patients with acute pancreatitis. Management and elimination of modifiable risk factors are recommended to improve clinical outcomes. We provide clinicians with multiple factors associated with having acute pancreatitis in patients with CD that might benefit from more aggressive monitoring.
Several limitations should be considered while interpreting the results of this study. NRD contains inpatient records only, and no outpatient records were included. The NRD file does not track patients hospitalized in one state and readmitted or transferred to a hospital in another state [27]. NRD does not provide data on prescribed medications and several CD medications have been associated with development with acute pancreatitis. NRD does not provide data on habitual alcohol consumption, smoking, or prescribed medications yet we were able to classify acute pancreatitis based on etiology. NRD does not provide data on laboratory test results, and we were unable to report data on pertinent continuous variables including lipase and amylase. The use of administrative codes (ICD-10-CM) is subject to misclassification. The study population has a high prevalence of gallstones and elevated calcium, both of which are known to cause acute pancreatitis. However, our study has several strengths. We used a large database, which is nationally representative of the US population. The NRD is a validated database used in clinical and epidemiological research and includes discharge data from 30 geographically dispersed states.
In conclusion, we observed a significant association between acute pancreatitis and worse hospitalization outcomes in our national cohort of CD patients. CD patients with acute pancreatitis were more likely to experience in-hospital mortality, hepatic failure, acute kidney failure, thrombocytopenia, and longer LOS. Gallstone disease, NAFLD, and hypercalcemia were associated with increased odds of having acute pancreatitis in patients with CD. As we aspire to control healthcare expenditure in CD patients, it becomes a priority to study comorbidities associated with worsening morbidity and mortality and to apply preventive measures to eliminate causes of nonelective preventable readmissions.
| Supplementary Material | ▴Top |
Suppl 1. International Classification of Diseases, Tenth Revision, Clinical Modification codes.
Acknowledgments
No acknowledgments to be declared.
Financial Disclosure
No financial relationships to be declared.
Conflict of Interest
Authors had no conflict of interest to be declared.
Informed Consent
No consent was required for the analysis as there were no patient-specific identifiers.
Author Contributions
Concept and design of the study: Ahmed Abomhya. AA, EC, FK, ZA, and HH contributed to the literacy search. All authors contributed to the analysis and interpretation of data. All authors contributed to drafting the manuscript and revising it critically for intellectual content: All authors approved the final version of the manuscript to be published.
Data Availability
The NRD is available at: https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
| References | ▴Top |
- Lee PJ, Papachristou GI. New insights into acute pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16(8):479-496.
doi pubmed - Khurana A, Nelson LW, Myers CB, Akisik F, Jeffrey BR, Miller FH, Mittal P, et al. Reporting of acute pancreatitis by radiologists-time for a systematic change with structured reporting template. Abdom Radiol (NY). 2020;45(5):1277-1289.
doi pubmed - Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1252-1261.
doi pubmed - Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet. 2017;389(10080):1741-1755.
doi - Moolsintong P, Loftus EV, Jr., Chari ST, Egan LJ, Tremaine WJ, Sandborn WJ. Acute pancreatitis in patients with Crohn's disease: clinical features and outcomes. Inflamm Bowel Dis. 2005;11(12):1080-1084.
doi pubmed - Feuerstein JD, Cheifetz AS. Crohn disease: epidemiology, diagnosis, and management. Mayo Clin Proc. 2017;92(7):1088-1103.
doi pubmed - Rasmussen HH, Fonager K, Sorensen HT, Pedersen L, Dahlerup JF, Steffensen FH. Risk of acute pancreatitis in patients with chronic inflammatory bowel disease. A Danish 16-year nationwide follow-up study. Scand J Gastroenterol. 1999;34(2):199-201.
doi pubmed - Weber P, Seibold F, Jenss H. Acute pancreatitis in Crohn's disease. J Clin Gastroenterol. 1993;17(4):286-291.
doi pubmed - Barthet M, Hastier P, Bernard JP, Bordes G, Frederick J, Allio S, Mambrini P, et al. Chronic pancreatitis and inflammatory bowel disease: true or coincidental association? Am J Gastroenterol. 1999;94(8):2141-2148.
doi pubmed - Yoon SB, Lee IS, Choi MH, Lee K, Ham H, Oh HJ, Park SH, et al. Impact of fatty liver on acute pancreatitis severity. Gastroenterol Res Pract. 2017;2017:4532320.
doi pubmed - Lorusso D, Leo S, Mossa A, Misciagna G, Guerra V. Cholelithiasis in inflammatory bowel disease. A case-control study. Dis Colon Rectum. 1990;33(9):791-794.
doi pubmed - Lapidus A, Bangstad M, Astrom M, Muhrbeck O. The prevalence of gallstone disease in a defined cohort of patients with Crohn's disease. Am J Gastroenterol. 1999;94(5):1261-1266.
doi pubmed - Parente F, Pastore L, Bargiggia S, Cucino C, Greco S, Molteni M, Ardizzone S, et al. Incidence and risk factors for gallstones in patients with inflammatory bowel disease: a large case-control study. Hepatology. 2007;45(5):1267-1274.
doi pubmed - Weersma RK, Peters FT, Oostenbrug LE, van den Berg AP, van Haastert M, Ploeg RJ, Posthumus MD, et al. Increased incidence of azathioprine-induced pancreatitis in Crohn's disease compared with other diseases. Aliment Pharmacol Ther. 2004;20(8):843-850.
doi pubmed - Park KT, Ehrlich OG, Allen JI, Meadows P, Szigethy EM, Henrichsen K, Kim SC, et al. The cost of inflammatory bowel disease: an initiative from the Crohn's & colitis foundation. Inflamm Bowel Dis. 2020;26(1):1-10.
doi pubmed - HCUP-US NRD Overview. Online July 21, 2021. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
- Rothstein MA. Is deidentification sufficient to protect health privacy in research? Am J Bioeth. 2010;10(9):3-11.
doi pubmed - Abomhya A, Mahmoodurrahman M, Ayaz S, Hamad H, Khan F. Burden and predictors of non-alcoholic fatty liver disease in a retrospective cohort of patients with Crohn's disease. Gastroenterology Res. 2022;15(2):82-90.
doi pubmed - Frey CF, Zhou H, Harvey DJ, White RH. The incidence and case-fatality rates of acute biliary, alcoholic, and idiopathic pancreatitis in California, 1994-2001. Pancreas. 2006;33(4):336-344.
doi pubmed - Kadayakkara DK, Beatty PL, Turner MS, Janjic JM, Ahrens ET, Finn OJ. Inflammation driven by overexpression of the hypoglycosylated abnormal mucin 1 (MUC1) links inflammatory bowel disease and pancreatitis. Pancreas. 2010;39(4):510-515.
doi pubmed - Pitchumoni CS, Rubin A, Das K. Pancreatitis in inflammatory bowel diseases. J Clin Gastroenterol. 2010;44(4):246-253.
doi pubmed - Ichihara S, Sato M, Kozuka S. Prevalence of pancreatitis in liver diseases of various etiologies: an analysis of 107,754 adult autopsies in Japan. Digestion. 1992;51(2):86-94.
doi pubmed - Tran DD, Oe PL, de Fijter CW, van der Meulen J, Cuesta MA. Acute renal failure in patients with acute pancreatitis: prevalence, risk factors, and outcome. Nephrol Dial Transplant. 1993;8(10):1079-1084.
- Kumar A, Kumar PG, Pujahari AK, Sampath S. Hypercalcemia Related Pancreatitis. Med J Armed Forces India. 2010;66(4):385-386.
doi - Jo IH, Paik CN. Acute pancreatitis with hypercalcemia as initial manifestation of multiple myeloma. Korean J Gastroenterol. 2020;75(4):220-224.
doi pubmed - Vaquero E, Casellas F, Bisbe V, Puig-Divi V, Bermejo B, Guarner L, Malagelada JR. [Thrombocytopenia onset in acute episodes of pancreatitis]. Med Clin (Barc). 1995;105(9):334-337.
- HCUP-US NRD Introduction. [Online, July 21. 2021]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2010-2018.pdf.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


