| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 9, September 2022, pages 377-387
A Newly Developed Interprofessional In-Situ Simulation-Based Training for Airway Management of COVID-19 Patients: Identification of Challenges and Safety Gaps, and Assessment of the Participants’ Reaction
Abdulrahman Y. Sabbagha, b, c, Hala M. Alzaida, Abdullah A. Almarshedb, Amani A. Azizalrahmanb, d, Shady Elmasrye, Claudia A. Rosuf, Usamah Alzoraigib, e, Abdulrahman Alzahrania, g, Ameera A. Cluntunc
aEmergency Department, King Fahad Medical City, Riyadh, Saudi Arabia
bCenter of Research, Education, Simulation, and Enhanced Training (CRESENT), King Fahad Medical City, Riyadh, Saudi Arabia
cSaudi Commissions for Health Specialties, Riyadh, Saudi Arabia
dPediatric Emergency Department, King Fahad Medical City, Riyadh, Saudi Arabia
eAnesthesia Department, King Fahad Medical City, Riyadh, Saudi Arabia
fCenter for Interprofessional Studies and Innovation, MGH Institute for Health Profession, Boston, MA, USA
gCorresponding Author: Abdulrahman Alzahrani, Emergency Department, King Fahad Medical City, Riyadh, Saudi Arabia
Manuscript submitted June 3, 2022, accepted July 18, 2022, published online September 29, 2022
Short title: ISS Training for Airway Management of COVID-19
doi: https://doi.org/10.14740/jocmr4756
| Abstract | ▴Top |
Background: Healthcare providers performing aerosol-generating procedures like airway management are at the highest risk for contamination with coronavirus disease 2019 (COVID-19). We developed an in-situ simulation (ISS) airway management training in confirmed or suspected COVID-19 patients for emergency and anesthesiology staff, evaluated participants’ reactions, and identified perceived challenges.
Methods: We used a cross-sectional study design incorporating a quantitative questionnaire to describe participants’ reaction to the ISS and a qualitative group interview using the plus-delta debriefing modality to explore participants’ challenges in acquiring the knowledge and skills required for each learning objective. Data were analyzed using descriptive statistics and deductive content analysis.
Results: Two hundred and ninety-nine healthcare providers participated in 62 ISS training sessions. Over 90% of our study participants agreed or strongly agreed that: they understood the learning objectives; the training material appropriately challenged them; the course content was relevant, easy to navigate, and essential; the facilitators’ knowledge, teaching, and style were appropriate; the simulation facilities were suitable; and they had ample opportunities to practice the learned skills. The main challenges identified were anticipating difficult airways, preparing intubation equipment, minimizing the number of personnel inside the room, adhering to the proper doffing sequence, preparing needed equipment outside the intubation room, speaking up, and ensuring closed-loop communication.
Conclusion: The newly developed ISS training was feasible for busy healthcare practitioners to safely perform airway management procedures for suspected or confirmed COVID-19 patients without affecting bedside care. Anticipation of difficult airways and speaking up were the most frequent challenges identified across all specialties in this study.
Keywords: Simulation-based education; COVID-19; Airway management; PPE; Kirkpatrick level 1; Evaluation; Interprofessional training; In-situ simulation
| Introduction | ▴Top |
Coronavirus disease 2019 (COVID-19), the infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), quickly became a worldwide threat to health and, particularly, to the health of healthcare providers. In Italy, healthcare professionals comprised 10.7% of the total number of cases [1]. In China, healthcare professionals represented 3.8% of all COVID-19 registered cases by February 2020, and 14.8% of these suffered severe or critical disease [2]. Rare breakthrough infections have been reported even among the healthcare providers immunized with the highly efficient BNT162b2 messenger RNA vaccine against SARS-CoV-2 [3]. The primary transmission mode of COVID-19 is via large respiratory droplets and direct contact (fomite) transfer. These virus-laden droplets have a diameter of more than 5 - 10 µm and usually disperse within a 2-m radius when emitted through sneezing and coughing by an infected patient. This contrasts with airborne transmission, which generally refers to particles smaller than 5 µm in diameter [4]. These particles can remain in the air for a prolonged period, disperse further by following the airflow, and penetrate standard surgical facemasks.
COVID-19 is currently not considered an airborne pathogen by the World Health Organization except in the context of aerosol-generating procedures (AGPs) [5]. AGPs are medical interventions that can produce virus-laden aerosolized droplet nuclei of sizes small enough to be considered airborne (e.g., tracheal intubation, non-invasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, bronchoscopy, airway suctioning, nebulization, and high-flow nasal oxygen) [4]. Airway management is a complicated procedure. Airway management of a critically ill patient suffering from infectious diseases comes with even more difficulties for the involved healthcare personnel. Existing literature showed that healthcare workers were at significant risk of infection during the SARS epidemic of 2003 [6], with tracheal intubation posing the highest risk for viral transmission [7]. However, the correct use of personal protective equipment (PPE) reduced transmission incidence significantly [8, 9]. Thus, special PPE donning and doffing procedures and algorithms were recommended for the healthcare practitioners performing airway management procedures [10]. Training of non-intensive care workers on critical care through healthcare courses can be supplied as a short-term education option in practice for a national emergency situation that requires immediate reactions in the event of a national emergency [11]. In-situ simulation (ISS) has been recognized as an essential tool for safety preparedness during the COVID-19 pandemic [12, 13]. To contribute to the COVID-19 prevention among healthcare professionals, we developed a novel ISS. Our goal was to train interprofessional adult and pediatric emergency and anesthesiology teams at King Fahad Medical City in Saudi Arabia in airway management for suspected or confirmed COVID-19 patients. The purpose of this multi-methods research study was to evaluate healthcare providers’ reactions to such training (Kirkpatrick evaluation level 1) and to identify the challenges encountered while adapting to the unique requirements of airway management in suspected or confirmed COVID-19 patients.
| Materials and Methods | ▴Top |
Study design
Following a pragmatic approach, we used a multi-method cross-sectional research design incorporating a quantitative questionnaire and a qualitative group interview using open-ended questions [14].
Participants and setting
A total of 299 healthcare providers were enrolled to participate in 62 ISS training sessions between April 5 and 24, 2020. We recruited adult emergency medicine, pediatric emergency medicine, and anesthesia departments’ staff to form teams of five healthcare professionals for each ISS session. We arranged the participants’ selection with the clinical department chairpersons and immediate supervisors for each discipline to randomly schedule an interprofessional team in each session. The team members were physicians, nurses, and respiratory therapists, or anesthesia technologists. The selection of the members of each team was decided the day before the ISS training session. Those selected were released from their clinical duties for the ISS training day. All participants signed an informed consent before enrolling in the study. Participation was voluntary and did not impact the participants’ job standing in any way. Participants had various professional backgrounds and had been involved in simulation-based learning activities at the Center of Research, Education, Simulation, and Enhanced Training (CRESENT); however, most participants were not exposed to ISS before this study. The researchers explained to participants the purpose of the study, and their participation in the study is voluntary and can be terminated at any point. The researchers explained to the participants that their decision to participate or refusal to participate would not impact their job standing in any way. This research was performed following the Declaration of Helsinki, and the Ethics Review Committee of the King Fahad Medical City in Riyadh, Saudi Arabia approved the study protocol (No. 20-199 on April 9, 2020).
Simulation scenario
Following the six-step curriculum development approach [15], six of the authors (Sabbagh AY, Cluntun A, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH) developed a simulation curriculum targeting the following competencies: 1) Airway management for COVID-19 patients; 2) Infection control measures in AGPs for COVID-19 patients; and 3) Multidisciplinary teamwork and communication skills. We chose plus-delta as a debriefing modality to analyze actions as it is simple and easy to implement and standardize. This modality allows participants to self-reflect on what went well and what needed improvement. In our situation, plus-delta is more advantageous because it can help busy healthcare staff to properly utilize the short time they are present there and allow debriefers to collect as many points as possible [3, 16-23]. The course’ authors designed a standardized format for debriefers when using plus-delta to guide the discussion toward main objectives (Supplementary Material 1, Table S1, www.jocmr.org), and all instructors used Flipchart to collect debriefing points and fill them in the format immediately after the course. The debriefing guide included five steps: reaction, case description, analysis using plus-delta, summarizing, and report and evaluation [24]. The aim of the step, a description of how to conduct it and what questions to ask were provided for each step.
Scenario validation and intervention
The simulation case scenario was reviewed and approved by the Curriculum Development Department at CRESENT. Between April 5 and 24, 2020, we conducted 62 1-h ISS sesstions to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients at the King Fahad Medical City departments. All ISS sessions took place in an unoccupied emergency room (ER) in the emergency department (ED), the pediatric ED, or an unoccupied operationg room (OR) during working hours. The study flow is presented in Figure 1.
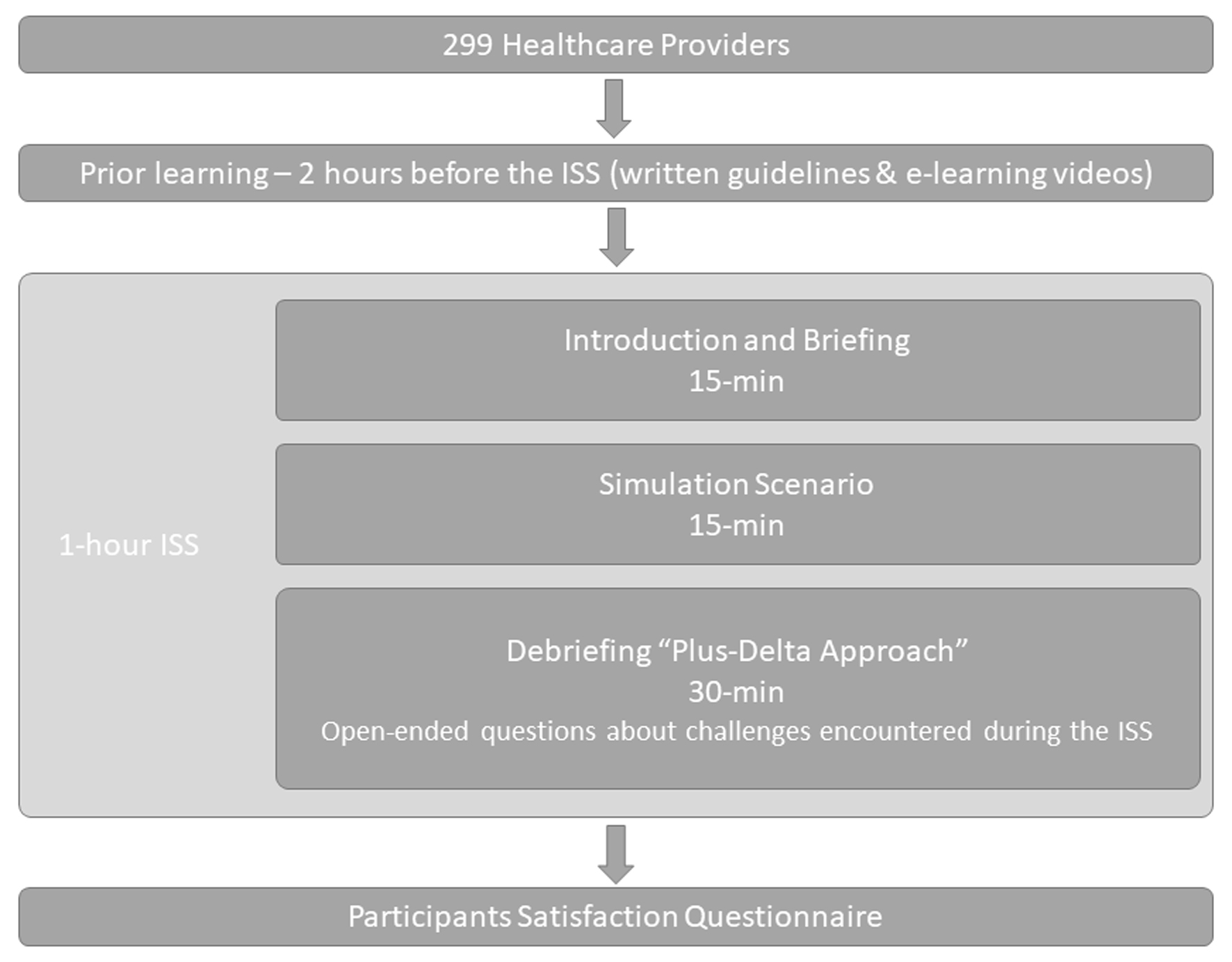 Click for large image | Figure 1. Study flow for in-situ simulation to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients. COVID-19: coronavirus disease 2019. |
All participants were encouraged to read pre-course learning materials 2 h before the ISS. Learning materials were optional refreshers of knowledge about the correct use of PPE and included a checklist of tasks for each team member’s role (Supplementary Material 2, www.jocmr.org) and a video. The 15-min video was created at CRESENT and demonstrated appropriate PPE donning and doffing techniques.
Each ISS session started with a 15-min introduction and briefing in which the facilitator explained to the participants the nature of the simulation-based learning and addressed participants’ psychological safety, fictional contract, simulation fidelity, and confidentiality issues. The learners were also oriented on the simulation equipment. The facilitator explicitly stated the specific learning objectives for each competency. After the introduction and briefing, a simulation case scenario was conducted for 15 min. This specific length of time was determined based on the expected duration for the selected procedures and to provide learning time in-situ. During this time, the participating team practiced airway management of a simulated COVID-19 patient. Simulation intubation instruments were identical to those used in our emergency and anesthesia departments, except for the N95 masks, replaced by simple surgical masks to overcome the shortage during that period. The simulation equipment included the iPad application “Simple Patient Monitor” developed by Michael George, Intubating Airman® task trainer, simulated PPE powered air-purifying respirator (PAPR), yellow gowns, head cover, shoe cover, and protective eyewear (shield or goggles). The simulation developers provided all facilitators with a facilitator guide for the briefing to minimize individual variability (Supplementary Material 3, www.jocmr.org). ISS session facilitators were consultant-level experts in adult emergency medicine, pediatric emergency medicine, and anesthesia, with formal clinical simulation training. During each debriefing, the facilitator asked the participants open-ended questions about the challenges they experienced during the simulation, both individually and as interprofessional team members. The facilitator summarized and reported the emerging topics linked to each objective from the discussion with the participants. The facilitators used the same approach for all sessions. After the simulation scenario ended, the facilitator followed a debriefing guide using the plus-delta approach and a reflection on takeaways points (Supplementary Material 1, www.jocmr.org) to facilitate the debriefing session (30 min duration). The participants were given a chance to be engaged and self-reflected on the experience in a safe learning environment. During each debriefing, the facilitator asked the participants open-ended questions about the challenges they experienced during the simulation, both individually and as interprofessional team members.
Data collection
After participating in the ISS training, each participant completed an online, self-administered survey focused on three different elements: topic content, delivery, and facilitator evaluation. The survey contained 21 close-ended questions adapted from Kirkpatrick’s learner-centered reaction sheet and a free narrative space for the participants to write takeaway points to see if they had achieved the desired learning outcomes (Supplementary Material 4, www.jocmr.org). The closed-ended questions were anchored on a four-point Likert scale ranging from 1 - strongly disagree to 4 - strongly agree.
The qualitative data were collected via group interviews during the plus-delta debriefing for all the simulation sessions. The debriefing facilitator wrote the participants’ answers to the open-ended questions on a board during each debriefing, then transcribed them verbatim into an Excel file immediately following the debriefing session.
Main outcome measures
We assessed participants’ reaction to the ISS training regarding the session’s objectives, materials, content relevance, simulation facilitator’s knowledge, delivery, and style, and program and facilities evaluation. We also investigated participants’ perceptions regarding the achievement of desired competencies (Kirkpatrick evaluation level 1).
Secondary outcome measures
We explored participants’ challenges - both individually and as members of the interprofessional team - in acquiring the knowledge and skills required for each learning objective.
Data analysis
We performed a descriptive statistical analysis to describe participants’ reactions to the simulation training. All statistical analyses were performed using Microsoft Excel (2021). The debriefing transcripts of responses to the open-ended questions were analyzed using deductive qualitative content analysis, drawing on the course objectives as the coding frame. The themes for our analysis were preset according to the course learning objectives. Several researchers performed individual open coding then met to discuss and agree on codes and code definitions (analysts triangulation) for credibility. Following open coding, similar codes were grouped into categories and subcategories. Each category was fitted into the corresponding theme. To ensure the confirmability of the findings, categories and subcategories were revised and discussed with Rosu CA, who has extensive experience in qualitative research (peer debriefing).
| Results | ▴Top |
Statistical analysis
A total of 62 ISS sessions were conducted: 15 for pediatric emergency teams, 20 for adult emergency teams, and 27 for anesthesia teams, respectively. Two hundred seventy-eight responses were collected from 299 participants (100% response rate from adult and pediatric emergency and 91.7% response rate from anesthesia participants). The description of our teams’ demographic characteristics is presented in Table 1.
 Click to view | Table 1. Teams’ Characteristics |
Participants’ reaction to the simulation training
Over 90% of the participants in our study agreed or strongly agreed that they understood and could relate each learning objective to the achieved learning and were appropriately challenged by the training material (Table 2). Similar percentages agreed or strongly agreed that course materials were easy to navigate and essential for the procedure’s safe practice, and the content was relevant. Facilitators’ knowledge, teaching, and style were deemed appropriate by more than 90% of the trainees. Similar percentages of study participants agreed or strongly agreed that they were given ample opportunity to practice the skills they learned and that the simulation facilities were suitable for such training.
 Click to view | Table 2. Participants’ Satisfaction With the Session’s Objectives, Materials, Content Relevance, and Facilitator’s Knowledge, Delivery, and Style |
Content analysis
Airway management challenges identified by the participants
Sixty-two Excel data files with the transcripts gathered from 62 simulations were analyzed. The absolute frequencies of the codes for each theme are presented in Table 3. The qualitative analysis identified themes and sub-themes common across the three specialties: pediatric emergency, adult emergency, and anesthesia for the three main learning competencies.
 Click to view | Table 3. Absolute Frequencies of Codes for Each Theme |
Regarding the airway management competency, the panel identified six categories (anticipation, preparation, pre-oxygenation, protection, placement, and post-intubation management) and 14 sub-themes. For the second competency - infection control measures - seven themes (equipment, crowd control, COVID-19 protection, donning, doffing, PPE, and room ventilation) and 12 sub-themes were described. Lastly, nine themes (clear orders, speaking up, role assignment, shared mental model, communication, mutual respect, leadership, anticipation, and situation awareness) and nine sub-themes were developed for the team dynamic. Each facilitator summarized an average of nine challenges per session documented on the board during the debriefing as delta (areas needing improvement). Table 4 presents the top three challenges encountered during the ISS training by specialty.
 Click to view | Table 4. Top Three Challenges Encountered During the In-Situ Simulation Training by Specialty |
| Discussion | ▴Top |
We developed and implemented a novel ISS to train interprofessional adult emergency, pediatric emergency, and anesthesiology teams in airway management for suspected or confirmed COVID-19 patients. We verified that most of the participants in these simulations found these efforts useful for their daily practice. We also identified specific challenges for the clinical practice and areas for which the intervention might protect healthcare providers and increase the safety of performing airway management procedures [14]. Our study offers an ISS curriculum that is feasible and can provide learning opportunities in a safe, simulated environment in the clinical area and can be replicated as deliberate practice. It helped explore possible challenges of both individual and system that help plan and prepare patients’ unexpected patterns related to the COVID-19 pandemic [25]. Hospital staff training was identified among the priorities during the COVID-19 pandemic [26]. Several studies utilized ISS to enhance hospital preparedness for the expected surge of COVID-19 patients. These studies identified and tested the readiness of the hospitals for the potential threats and risks imposed by COVID-19 and uncovered areas for improvement and timely staff training in the workplace [27-30].
Furthermore, the literature reports the advantages of ISS training for airway management of COVID-19 patients conducted for interprofessional teams training in EDs, critical care units, and operating rooms [31-34]. Our results are consistent with previous reports and support the benefits of ISS with interprofessional teams training for airway management in the pediatric emergency, adult emergency, and anesthesiology departments [12, 26, 28, 35]. In general, airway management is a complicated procedure that requires a combination of healthcare providers’ knowledge, skills, and behaviors. Simulation-based airway management training is superior to non-simulation intervention to achieve desired educational outcomes [36]. Simulation-based training conducted in real clinical environments using the available equipment and resources and involving actual healthcare teams offers experiential learning that promotes safety and enhanced team communication [29, 34]. ISS is more feasible for healthcare professionals in scheduling and availability without taking staff away from their clinical work and settings. In previous applications, ISS accelerated the development of skills and agility [29, 33, 37]. Similarly, in our study, participants in different clinical areas (pediatric ED and adult ED and ORs) reported that they felt prepared to care for COVID-19 patients’ airways while working in interprofessional teams utilizing appropriate infection control measures.
Other studies utilizing simulation-based training revealed significant latent risks and provided recommendations and corrections in the systems to respond to airway management for COVID-19 patients and infection prevention measures [29]. The use of ISS helped develop workable guidelines and visual aids that enhanced infection control measures implementation [31]. Using frequent ISS in the OR in preparation for surgical management of COVID-19 patients allowed the identification of potential threats and needed logistics for the work processes [38]. A study utilizing ISS to evaluate the readiness of intesive care unit (ICU) staff for COVID-19 patients identified deficiencies in ICU isolation rooms’ operation. These findings led to corrective actions to be taken before their first COVID-19 patient admission [31]. A similar study that utilized multidisciplinary ISS to understand preparation requirements for an outbreak and to assess the status quo before implementing adjustments resulted in mindful planning and resource allocation. The interdepartmental ISS training opportunities helped identify system issues and safety hazards in acute care settings [32].
Debriefing after the ISS was also one of the leading resources to identify safety threats. Most of the participants reported that they felt more prepared to provide care for COVID-19 patients [29]. Efforts were made to explore using simulation-based disaster exercises to test planned protocols for suspected COVID-19 patients in Saudi Arabia [30]. Mock codes conducted in the ED allowed early identification of defects related to preparedness and increased staff confidence in dealing with COVID-19 patients [39]. At our medical center, we explored individual, team, and system-related challenges experienced during ISS for airway management for COVID-19 patients. Multiple challenges emerged using the plus-delta debriefing method and were grouped into themes with corresponding categories and subcategories. Anticipating difficult airways and speaking up were the two most common ones across all the specialties included in our study.
Safe and secure airway management can be challenging in the OR, extending even postoperative. What’s more, failed intubation remains a significant cause of morbidity and mortality. Previously published literature identified anticipating the possibility of difficult airway preoperatively and modifying the airway management appropriately as a challenge for all the team members involved in the care of such patients [40, 41]. The participants in our study voiced similar concerns. These concerns were discussed in the debriefing in each ISS. The simulated experience helped the participants recognize various possible challenges in airway management and the need for a comprehensive action plan in preparation for possible challenges.
Speaking up is essential in multidisciplinary care teams, particularly in the OR, where patient safety can be in immediate danger. In recent years, simulation has been used to examine this concept in the OR [42-44]. Hierarchy gradients, organizational culture, and education were the most frequent factors affecting one’s ability to speak up and effectively challenge authority. Additionally, leader inclusiveness and creating a psychologically safe environment were found to help team members to overcome professional status differences and foster collaboration [45, 46]. We, too, found speaking up to be one of the two most frequent challenges across all the medical specialties included in the study. Explaining the causes of this finding was beyond the scope of the present study, but it might be due to individual, situational, or interpersonal and cultural factors.
Limitations
Our study has several limitations. We used a convenience sample not to interrupt the staff’s workflow in their specific departments. Thus, we may not have captured the whole range of reactions to our education intervention. We cannot estimate the magnitude of the sampling error since we performed only descriptive statistical analyses. To mitigate the inherent bias in self-reporting data, we collected and analyzed quantitative and qualitative data. In addition, we are unsure when and how many times the participants watched the training video; thus, we cannot eliminate exposure bias. Furthermore, our ISS was employed for adult and pediatric emergency medicine and anesthesiology staff; more research is necessary to assess the replicability of our findings beyond our context. What’s more, while knowing how well a training program is received (Kirkpatrick level 1) is essential, future evaluations to assess participants’ acquisition of the required knowledge and skills and to what extent this training is beneficial to our medical center (Kirkpatrick levels 2 and 3) are necessary to enhance and maintain our newly developed simulation curriculum.
Conclusions
The newly developed ISS training was feasible to train adult and pediatric emergency and anesthesiology healthcare practitioners to safely perform airway management procedures for suspected or confirmed COVID-19 patients without affecting the clinical care at the bedside. “Anticipation of difficult airways” and “speaking up” were the most frequent among the challenges we identified and were shared across all specialties included in this study.
| Supplementary Material | ▴Top |
Suppl 1. Learning materials: checklist of tasks for each team member’s role.
Suppl 2. Facilitator guide for briefing.
Suppl 3. Debriefing guide for the facilitator (instructor).
Suppl 4. Kirkpatrick’s learner-centered reaction sheet.
Acknowledgments
The authors would like to thank Mohammad Alamar, Asim Alsaeed, Areej Almuwaisheer, Rawan Eskandrani, Shadi Almozaini, Mosa Alkhalifa, and Ziad Zikri for their help with this study and also Suzan Kardong-Edgren for reviewing the manuscript.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the study subjects before participating in the study.
Author Contributions
Sabbagh AY and Cluntun A contributed to study conceptualization and design. Sabbagh AY, Cluntun A, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH developed the simulation curriculum. Alzaid H and Sabbagh AY contributed to the acquisition of data. Sabbagh AY, Azizalrahman A, Almarshed A, Alzaid H, and Elmasry SH contributed to data analysis and interpretation. Rosu CA contributed to peer debriefing and provided input to the strategy for qualitative data analysis and interpretation. Sabbagh AY, Cluntun A, Almarshed A, Alzaid H, and Alzahrani A wrote the manuscript. Rosu CA and Alzoraigi U edited and revised the manuscript. Alzahrani A prepared and submitted the manscript for publication.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Lapolla P, Mingoli A, Lee R. Deaths from COVID-19 in healthcare workers in Italy-What can we learn? Infect Control Hosp Epidemiol. 2021;42(3):364-365.
doi pubmed - Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72314 cases from the chinese center for disease control and prevention. JAMA. 2020;323(13):1239-1242.
doi pubmed - Bergwerk M, Gonen T, Lustig Y, Amit S, Lipsitch M, Cohen C, Mandelboim M, et al. COVID-19 breakthrough infections in vaccinated health care workers. N Engl J Med. 2021;385(16):1474-1484.
doi pubmed - Transmission of SARS-CoV-2: implications for infection prevention precautions [Internet]. Available at: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions. Accessed May 9, 2021.
- Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, Wong MSY, Marimuthu K. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020;323(16):1610-1612.
doi pubmed - Kamming D, Gardam M, Chung F. Anaesthesia and SARS. Br J Anaesth. 2003;90(6):715-718.
doi pubmed - Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797.
doi pubmed - Nicolle L. SARS safety and science. Can J Anaesth. 2003;50(10):983.
doi pubmed - Yao W, Wang T, Jiang B, Gao F, Wang L, Zheng H, Xiao W, et al. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth. 2020;125(1):e28-e37.
- Lois F, Hallet C, Samalea Suarez N, Ghuysen A, Brichant JF. In situ simulation improves perceived self-efficacy of OR nurses and anaesthesiologists during COVID-19 pandemic. BMJ Simul Technol Enhanc Learn. 2021;7(6):555-560.
doi pubmed - Alsolamy S, Cluntun A, Aldekhyl S, Sabbagh AY, Alshehri TO, Yousif S, Abuznadah WT, et al. A national initiative: training nonintensivists in critical care, an educational response to the COVID-19 pandemic. Saudi Crit Care J. 2020;4(Suppl S1):34-39.
- Fregene TE, Nadarajah P, Buckley JF, Bigham S, Nangalia V. Use of in situ simulation to evaluate the operational readiness of a high-consequence infectious disease intensive care unit. Anaesthesia. 2020;75(6):733-738.
doi pubmed - Sharara-Chami R, Sabouneh R, Zeineddine R, Banat R, Fayad J, Lakissian Z. In situ simulation: an essential tool for safe preparedness for the COVID-19 pandemic. Simul Healthc. 2020;15(5):303-309.
doi pubmed - Zuo MZ, Huang YG, Ma WH, Xue ZG, Zhang JQ, Gong YH, Che L, et al. Expert recommendations for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J. 2020;35(2):105-109.
doi pubmed - Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum development for medical education: A six-step approach. Johns Hopkins University Press; 2015.
- Sawyer T, Eppich W, Brett-Fleegler M, Grant V, Cheng A. More than one way to debrief: a critical review of healthcare simulation debriefing methods. Simul Healthc. 2016;11(3):209-217.
doi pubmed - Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc. 2007;2(2):115-125.
doi pubmed - Mullan PC, Wuestner E, Kerr TD, Christopher DP, Patel B. Implementation of an in situ qualitative debriefing tool for resuscitations. Resuscitation. 2013;84(7):946-951.
doi pubmed - Sweberg T, Sen AI, Mullan PC, Cheng A, Knight L, Del Castillo J, Ikeyama T, et al. Description of hot debriefings after in-hospital cardiac arrests in an international pediatric quality improvement collaborative. Resuscitation. 2018;128:181-187.
doi pubmed - Zinns LE, Mullan PC, O'Connell KJ, Ryan LM, Wratney AT. An Evaluation of a New Debriefing Framework: REFLECT. Pediatr Emerg Care. 2020;36(3):147-152.
- Ahmed M, Arora S, Russ S, Darzi A, Vincent C, Sevdalis N. Operation debrief: a SHARP improvement in performance feedback in the operating room. Ann Surg. 2013;258(6):958-963.
doi pubmed - Rose S, Cheng A. Charge nurse facilitated clinical debriefing in the emergency department. CJEM. 2018;20(5):781-785.
doi pubmed - Eppich W, Cheng A. Promoting excellence and reflective learning in simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015;10(2):106-115.
doi pubmed - Gardner R. Introduction to debriefing. Semin Perinatol. 2013;37(3):166-174.
doi pubmed - COVID-19 Public Health Emergency of International Concern (PHEIC) Global research and innovation forum [Internet]. Available at: https://www.who.int/publications/m/item/covid-19-public-health-emergency-of-international-concern-(pheic)-global-research-and-innovation-forum. Accessed May 9, 2021.
- Munzer BW, Bassin BS, Peterson WJ, Tucker RV, Doan J, Harvey C, Sefa N, et al. In-situ simulation use for rapid implementation and process improvement of COVID-19 airway management. West J Emerg Med. 2020;21(6):99-106.
doi pubmed - Brazil V, Lowe B, Ryan L, Bourke R, Scott C, Myers S, Kaneko H, et al. Translational simulation for rapid transformation of health services, using the example of the COVID-19 pandemic preparation. Adv Simul (Lond). 2020;5:9.
doi pubmed - Daly Guris RJ, Doshi A, Boyer DL, Good G, Gurnaney HG, Rosenblatt S, McGowan N, et al. Just-in-time simulation to guide workflow design for coronavirus disease 2019 difficult airway management. Pediatr Crit Care Med. 2020;21(8):e485-e490.
doi pubmed - Dharamsi A, Hayman K, Yi S, Chow R, Yee C, Gaylord E, Tawadrous D, et al. Enhancing departmental preparedness for COVID-19 using rapid-cycle in-situ simulation. J Hosp Infect. 2020;105(4):604-607.
doi pubmed - Lababidi HMS, Alzoraigi U, Almarshed AA, AlHarbi W, AlAmar M, Arab AA, Mukahal MA, et al. Simulation-based training programme and preparedness testing for COVID-19 using system integration methodology. BMJ Simul Technol Enhanc Learn. 2021;7:126-133.
doi - Choi GYS, Wan WTP, Chan AKM, Tong SK, Poon ST, Joynt GM. Preparedness for COVID-19: in situ simulation to enhance infection control systems in the intensive care unit. Br J Anaesth. 2020;125(2):e236-e239.
doi pubmed - Jee M, Khamoudes D, Brennan AM, O'Donnell J. COVID-19 Outbreak Response for an Emergency Department Using In Situ Simulation. Cureus. 2020;12(4):e7876.
doi pubmed - Muret-Wagstaff SL, Collins JS, Mashman DL, Patel SG, Pettorini K, Rosen SA, Shaffer VO, et al. In situ simulation enables operating room agility in the COVID-19 pandemic. Ann Surg. 2020;272(2):e148-e150.
doi pubmed - Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Saf. 2013;22(6):468-477.
doi pubmed - Fong S, Li E, Violato E, Reid A, Gu Y. Impact of aerosol box on intubation during COVID-19: a simulation study of normal and difficult airways. Can J Anaesth. 2021;68(4):496-504.
doi pubmed - Kennedy CC, Cannon EK, Warner DO, Cook DA. Advanced airway management simulation training in medical education: a systematic review and meta-analysis. Crit Care Med. 2014;42(1):169-178.
doi pubmed - Dieckmann P, Torgeirsen K, Qvindesland SA, Thomas L, Bushell V, Langli Ersdal H. The use of simulation to prepare and improve responses to infectious disease outbreaks like COVID-19: practical tips and resources from Norway, Denmark, and the UK. Adv Simul (Lond). 2020;5:3.
doi pubmed - Tong QJ, Chai JX, Tan LH, Prit S, Ong LT, Wu MYL, Ng LXL. Assessing operating room preparedness for COVID-19 patients through in situ simulations. Anesth Analg. 2020;131(2):e104-e106.
doi pubmed - Aljahany M, Alassaf W, Alibrahim AA, Kentab O, Alotaibi A, Alresseeni A, Algarni A, et al. Use of in situ simulation to improve emergency department readiness for the COVID-19 pandemic. Prehosp Disaster Med. 2021;36(1):6-13.
doi pubmed - Gende G, Xing Y, Wen J, Raymond J, Laim E, Konga V, Dimugu L, et al. Management of difficult airways in surgical patients at the Port Moresby General Hospital operating theatre and intensive care unit. P N G Med J. 2012;55(1-4):67-75.
- Kollmeier BR, Boyette LC, Beecham GB, Desai NM, Khetarpal S. Difficult airway. StatPearls. Treasure Island (FL). 2021.
- Belyansky I, Martin TR, Prabhu AS, Tsirline VB, Howley LD, Phillips R, Sindram D, et al. Poor resident-attending intraoperative communication may compromise patient safety. J Surg Res. 2011;171(2):386-394.
doi pubmed - Lyndon A, Sexton JB, Simpson KR, Rosenstein A, Lee KA, Wachter RM. Predictors of likelihood of speaking up about safety concerns in labour and delivery. BMJ Qual Saf. 2012;21(9):791-799.
doi pubmed - Pian-Smith MC, Simon R, Minehart RD, Podraza M, Rudolph J, Walzer T, Raemer D. Teaching residents the two-challenge rule: a simulation-based approach to improve education and patient safety. Simul Healthc. 2009;4(2):84-91.
doi pubmed - Edmondson AC. Speaking up in the operating room: how team leaders promote learning in interdisciplinary action teams. Journal of Management Studies. 2003;40:1419-1452.
doi - Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. Journal of Organizational Behavior. 2006;27:941-966..
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


