| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Case Report
Volume 14, Number 7, July 2022, pages 287-290
Making Emergency Surgical Decisions Without any Imaging Evidence: A Case Report of Complicated Diverticular Phlegmon
Paschalis Gavriilidisa, c, Francisco Reyes Miliana, Derek Burkeb, Peter Mossb
aDepartment of Surgery, Saint Helena General Hospital, Jamestown, STHL 1ZZ Saint Helena, South Atlantic Ocean, UK
bDepartment of General Medicine, Saint Helena General Hospital, Jamestown, STHL 1ZZ Saint Helena, South Atlantic Ocean, UK
cCorresponding Author: Paschalis Gavriilidis, Department of Surgery, Saint Helena General Hospital, Jamestown, STHL 1ZZ Saint Helena, South Atlantic Ocean, UK
Manuscript submitted May 29, 2022, accepted July 8, 2022, published online July 29, 2022
Short title: A Case of Complicated Diverticular Phlegmon
doi: https://doi.org/10.14740/jocmr4750
| Abstract | ▴Top |
Acute left-sided diverticulitis is the third most common gastrointestinal disease after acute pancreatitis and cholecystitis requiring hospitalization. From those patients, 15% to 20% were diagnosed with abscess on the computed tomography (CT) scan. Usually, abscess larger than 5 cm are not amenable for medical treatment. A 61-year-old woman presented to emergency department of the general hospital in the remote island with 48-h history of fever, tachypnea, and tachycardia. Physical examination revealed 15 × 7 cm mass occupying the left mid-abdomen and iliac fossa. Patient did not report any unintentional loss of weight or change of bowel habits. She only reported that the last month she felt her lower tummy bloated. Due to absence of radiographer during this period in the hospital there was no possibility for any imaging investigations. Diagnostic laparoscopy revealed a phlegmon in the left abdomen consisting of the sigmoid colon, loops of the small bowel and wrapped by the omentum. Hartmann procedure was performed. Patient recovered uneventfully and was scheduled for reversal procedure. Surgical intervention is the treatment of choice for complicated large diverticular abscess; in the remote island, any delayed diagnosis may lead to life-threatening complications.
Keywords: Diverticulitis; Diverticular phlegmon; Diverticular abscess
| Introduction | ▴Top |
There is evidence of increase of prevalence of diverticulosis in the last century. Recent data demonstrated that prevalence ranges 5% and 50% among patients younger than 40 years and elder than 60 years, respectively [1]. Moreover, the incidence of diverticulitis increased by 60% and the rates of hospital admission and elective surgery for this condition increased by 26% and 38%, respectively. In addition, the mean age of hospitalized patients decreased from 64.6 to 61.8 years old [2]. Use of nonsteroidal anti-inflammatory drugs, smoking, obesity, and physical inactivity were reported as risk factors for diverticulitis [2]. The diagnostic investigation of choice is the multi-slice computed tomography (CT) scan with intravenous and luminal contrast material; its reported sensitivity and specificity are 98% and 99%, respectively [3]. Abscess larger than 5 cm usually, is not amenable to medical treatment [2]. It has been reported that 14% to 24% of patients with acute diverticulitis undergo emergency surgical procedures; in particular, only half of this cohort undergo Hartmann procedure, and 30% of these patients will not have their stomas reversed [4].
Decision making under stressful conditions of emergency department and for patients with acute surgical pathologies requiring urgent treatment is always treacherous and difficult. Moreover, in the remote island and in some periods of the year without the help of any imaging evidence, treatment decisions can be based only on adept clerking and sound clinical judgement [5].
The aim of the present study was to present the management of acute complicated diverticular abscess without the help of any imaging evidence in the remote island.
| Case Report | ▴Top |
An otherwise healthy 61-year-old woman with body mass index (BMI) 39.8 presented to emergency department of the general hospital in the remote island with 48-h history of fever, tachypnea, and tachycardia. Past medical history was unremarkable; she was not on any medications and did not report any allergies. Vital signs were respiratory rate 25 (breaths/min), temperature 38.8 °C, heart rate 104 beats/min, and blood pressure 110/60 mm Hg. Physical examination revealed 15 × 7 cm mass occupying the left mid-abdomen and iliac fossa. Notably there were unremarkable tenderness on palpation without aggravating factors. Patient did not report any change of bowel habits or unintentional loss of weight. She only reported that the last month she felt her lower tummy bloated. She smokes 20 cigarettes and drinks a glass of alcoholic beverage daily. Laboratory results were white blood cells 18.300 (4.0 - 11.0), neutrophils 13.11 (2.5 - 6.0), platelet (PLT) 594 (150 - 450), C-reactive protein (CRP) 280 (0 - 9) mg/L, alkaline phosphatase 241 (38 - 126) IU/L. Due to absence of the radiographer during this period there was no possibility for further imaging investigations in the hospital. Considering that the patient was septic we decided further to investigate her with the only tool that we have at this time, the diagnostic laparoscopy. It revealed a phlegmon in the left abdomen consisting of the sigmoid colon, loops of the small bowel and wrapped by the omentum. Blunt dissection of the mass released a large amount of pus. The operation was converted to open one. Consequently, sigmoidectomy (Hartmann procedure) and concomitant small bowel resection were performed (Fig. 1). Patient recovered uneventfully and was transferred to surgical ward. Histology report came back as diverticulosis in the sigmoid colon complicated by diverticulitis and perforation. No invasive malignancy was detected in the examined surgical specimen. Patient was discharged home and scheduled for reversal procedure in 3 months.
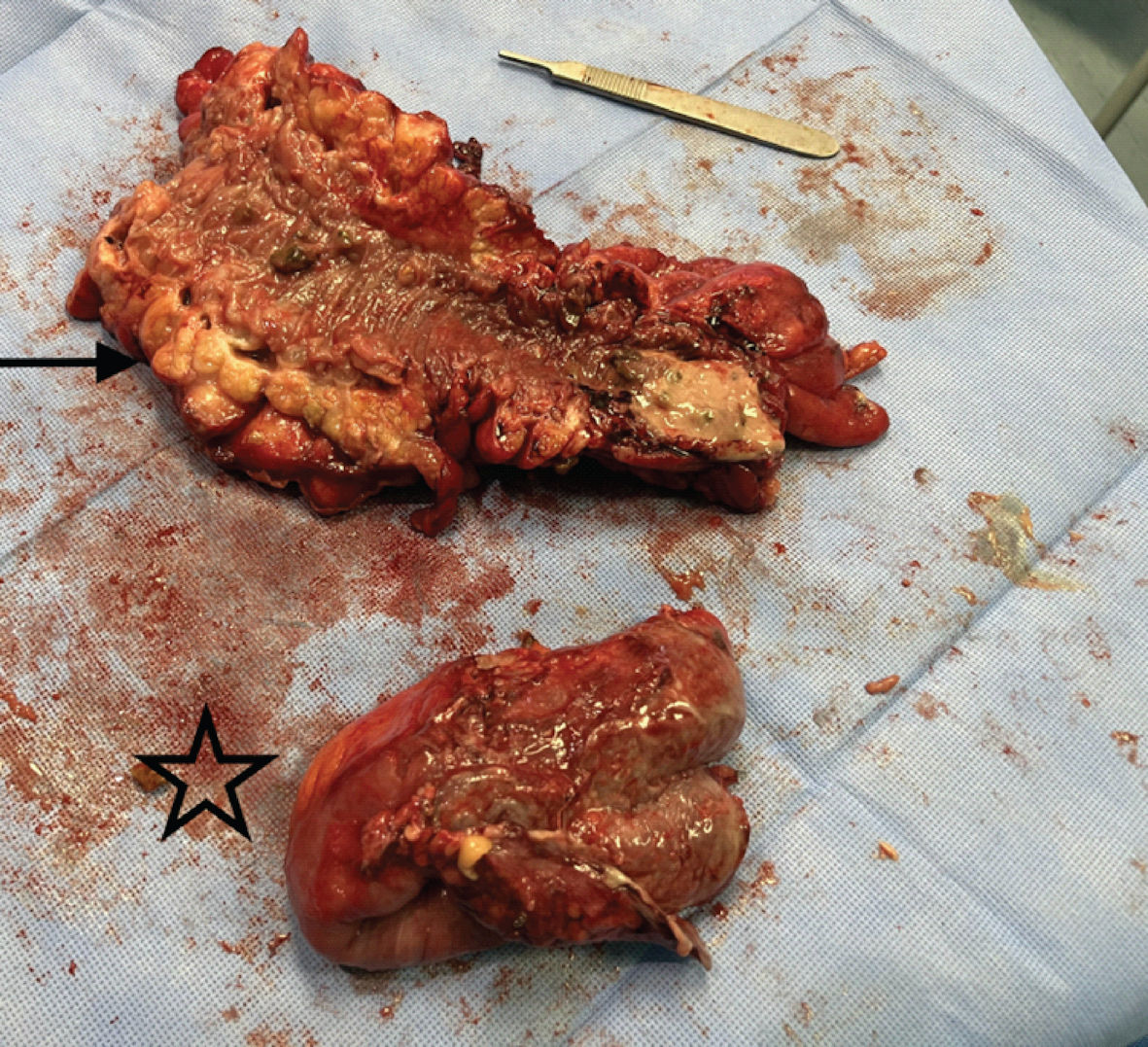 Click for large image | Figure 1. Surgical specimen of sigmoid 218 × 210 × 75 mm demonstrating diverticulosis complicated by diverticulitis and perforation (arrow). Star: small bowel 220 × 48 × 37 mm consisting part of the diverticular phlegmon. |
| Discussion | ▴Top |
Although acute diverticulosis is one of the most common diseases encountered by surgeon in emergency settings there is no common classification so far [6, 7]. Hinchey classification, Kohler modification, modified Hinchey and Hansen/Stock are the most common used classifications [6-11]. However, none of them conclusively has been proven to be superior to each other [6, 7]. Notably, recent evidence challenges the established knowledge that states that patients diagnosed with colonic diverticulosis have 10% to 25% lifetime risk to develop acute diverticulitis [12]. Shahedi et al demonstrated that these conclusions were based on before population-based colonoscopy, thus the real prevalence rate of diverticulosis was not known. Data based on colonoscopic diagnoses of diverticulosis demonstrate that the cumulative lifetime risk of developing acute diverticulitis is 4% only [12].
Admissions for acute diverticulitis are the third most common one after acute pancreatitis and cholecystitis and costing more than colorectal cancer, acute appendicitis, and inflammatory bowel disease [7]. From those admissions approximately 15-20% were diagnosed with an abscess on the CT scan [13]. The size of 4 - 5 cm is the limit between the medical and surgical treatment. Before the invention of radiologically guided drainage, 15% of operations for complicated diverticulitis were for abscess drainage [14]. There is an ongoing debate for the best treatment option for abscess bigger than 4 cm. Siewert et al demonstrated that 40% of patients with abscesses > 4 cm avoided surgery when treated with CT-guided drainage [15]. In addition, Singh et al in a cohort stated that with median abscess size 8.5 cm, 50% of patients avoided surgery when undergo CT drainage [16]. However, any progression of the inflammatory markers and CT scan findings of non-reduction of the abscess are absolute indications for surgical intervention [6]. In our case, all the inflammatory markers were remarkably high and there was palpable abscess of 15 × 7 cm. It has been reported that CRP cut-off value of 170 mg/L significantly discriminates mild from severe diverticulitis [6]. Makela et al demonstrated that CRP of 149.5 mg/L significantly discriminates between complicated and uncomplicated diverticulitis. In addition, patient who died had mean CRP of 207 mg/L [17]. In our case, CRP was 280 mg/L. However, low values of CRP should be treated cautiously considering to exclude acute diverticulitis because peak values are reached in 48 h from the onset of the episode [18]. It has been reported that positive and negative predictive values of clinical diagnosis of acute diverticulitis were 0.65 and 0.98, respectively. Diagnostic accuracy has been improved by 37% with radiology examinations but changed the treatment plan in only 7% of cases [19]. The most characteristic criteria for clinical diagnosis were described the localized tenderness over the left lower quadrant, aggravation of pain on movement, the absence of vomiting, and CRP of > 50mg/L [6]. In our case, although the inflammatory markers were high and mass were easily palpable, the clinical symptoms were not remarkable. The most probable explanation is that the abscess was well wrapped by the omentum and the high BMI.
An Australian study based on data of eight tertiary referral colorectal centers confirmed that the most common used intervention in treating diverticular peroration worldwide is the Hartmann procedure [20].
Recent update of guidelines recommends in clinically stable patients with no comorbidities a surgical alternative to Hartmann procedure can be primary resection with anastomosis and with or without defunctioning stoma. However, the above recommendation is based on low-quality evidence, 2B [6].
Conclusions
Surgical intervention is the treatment of choice for large complicated diverticular abscess; in the remote island, any delayed diagnosis may lead to life-threatening complications. Surgical decisions should be based on adept clerking and sound clinical judgement.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None to declare.
Informed Consent
Patient consented his case to be published anonymized in the medical literature.
Author Contributions
Gavriilidis P: conceptualization, formal analysis, investigation, methodology, software, validation, writing-original draft, editing, approval; Reyes Milian F: formal analysis, investigation, validation, editing, approval; Burke D: formal analysis, investigation, validation, editing, approval, Moss P: conceptualization, formal analysis, investigation, methodology, software, validation, writing-original draft, editing, approval, supervision.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Weizman AV, Nguyen GC. Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25(7):385-389.
doi pubmed - Young-Fadok TM. Diverticulitis. N Engl J Med. 2018;379(17):1635-1642.
doi pubmed - Lameris W, van Randen A, Bipat S, Bossuyt PM, Boermeester MA, Stoker J. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18(11):2498-2511.
doi pubmed - Etzioni DA, Mack TM, Beart RW, Jr., Kaiser AM. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg. 2009;249(2):210-217.
doi pubmed - Gavriilidis P, Reyes Milian F, Kacarevic D, Burke D. Combined gluteal and posterior thigh compartment syndrome without associated fracture: a case report. J Clin Med Res. 2022;14(4):170-173.
doi pubmed - Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15(1):32.
doi pubmed - Collins D, Winter DC. Modern concepts in diverticular disease. J Clin Gastroenterol. 2015;49(5):358-369.
doi pubmed - Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85-109.
- Kohler L, Sauerland S, Neugebauer E. Diagnosis and treatment of diverticular disease: results of a consensus development conference. The Scientific Committee of the European Association for Endoscopic Surgery. Surg Endosc. 1999;13(4):430-436.
- Wasvary H, Turfah F, Kadro O, Beauregard W. Same hospitalization resection for acute diverticulitis. Am Surg. 1999;65(7):632-635; discussion 636.
- Hansen O, Graupe F, Stock W. [Prognostic factors in perforating diverticulitis of the large intestine]. Chirurg. 1998;69(4):443-449.
doi pubmed - Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, Agarwal N, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11(12):1609-1613.
doi pubmed - Andersen JC, Bundgaard L, Elbrond H, Laurberg S, Walker LR, Stovring J, Danish Surgical S. Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59(5):C4453.
- Rodkey GV, Welch CE. Changing patterns in the surgical treatment of diverticular disease. Ann Surg. 1984;200(4):466-478.
doi pubmed - Siewert B, Tye G, Kruskal J, Sosna J, Opelka F, Raptopoulos V, Goldberg SN. Impact of CT-guided drainage in the treatment of diverticular abscesses: size matters. AJR Am J Roentgenol. 2006;186(3):680-686.
doi pubmed - Singh B, May K, Coltart I, Moore NR, Cunningham C. The long-term results of percutaneous drainage of diverticular abscess. Ann R Coll Surg Engl. 2008;90(4):297-301.
doi pubmed - Makela JT, Klintrup K, Takala H, Rautio T. The role of C-reactive protein in prediction of the severity of acute diverticulitis in an emergency unit. Scand J Gastroenterol. 2015;50(5):536-541.
doi pubmed - Gewurz H, Mold C, Siegel J, Fiedel B. C-reactive protein and the acute phase response. Adv Intern Med. 1982;27:345-372.
doi - Toorenvliet BR, Bakker RF, Breslau PJ, Merkus JW, Hamming JF. Colonic diverticulitis: a prospective analysis of diagnostic accuracy and clinical decision-making. Colorectal Dis. 2010;12(3):179-186.
doi pubmed - Hong MK, Tomlin AM, Hayes IP, Skandarajah AR. Operative intervention rates for acute diverticulitis: a multicentre state-wide study. ANZ J Surg. 2015;85(10):734-738.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


