| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 14, Number 5, May 2022, pages 196-201
Mean Arterial Pressure Goal in Critically Ill Patients: A Meta-Analysis of Randomized Controlled Trials
Sauradeep Sarkara, d, Sahib Singhb, Amit Routc
aDepartment of Pulmonary and Critical Care, West Virginia University School of Medicine, Morgantown, WV, USA
bDepartment of Internal Medicine, Sinai Hospital of Baltimore, Baltimore, MD, USA
cDepartment of Cardiology, University of Louisville, Louisville, KY, USA
dCorresponding Author: Sauradeep Sarkar, Department of Pulmonary and Critical Care, West Virginia University School of Medicine, Morgantown, WV, USA
Manuscript submitted March 6, 2022, accepted April 20, 2022, published online May 10, 2022
Short title: MAP Goal in Critically Ill Medical Patients
doi: https://doi.org/10.14740/jocmr4702
| Abstract | ▴Top |
Background: Current guidelines recommend targeting a mean arterial pressure (MAP) goal of 65 mm Hg or more in critically ill medical patients. Prospective studies have shown that a higher MAP goal can improve survival and decrease end-organ damage. However, randomized controlled trials (RCTs) have failed to show similar results. Thus, we performed this meta-analysis to evaluate whether a high MAP goal compared to a standard or low MAP goal will improve clinical outcomes in critically ill medical patients.
Methods: We searched electronic databases for RCTs comparing standard MAP goals versus high MAP goals in critically ill medical patients. A standard MAP goal was defined as a MAP of 60 - 70 mm Hg, and a MAP of 70 mm Hg or more was considered a high MAP goal. Outcomes of interest were mortality, duration of mechanical ventilation, and intensive care unit (ICU) length of stay. Subgroup analysis was performed based on the type of critically ill patients: cardiac arrest and septic shock. We used random-effects meta-analysis to estimate risk ratio (RR) with a 95% confidence interval (CI) for a dichotomous outcome. For continuous outcomes, the inverse variance method was used to calculate the standardized mean difference (SMD) with 95% CI. A P value of 0.05 or less was considered significant.
Results: Six RCTs with a total of 3,753 patients (standard MAP goal: n = 1,872 and high MAP goal: n = 1,881) were included in the final analysis. Both standard/low MAP goal and high MAP goal were associated with similar risk for mortality (RR 0.94, 95% CI (0.87, 1.01), P = 0.11), duration of mechanical ventilation (SMD 0.51, 95% CI (-0.29, 1.31), P = 0.21) and ICU length of stay (SMD 0.22, 95% CI (-0.07, 0.5), P = 0.14). Subgroup analysis in cardiac arrest patient showed decreased ICU stay (SMD 0.55, 95% CI (0.31, 0.80), P < 0.000001) in patients with higher MAP goal compared to the standard MAP goal group without any difference in mortality or duration of mechanical ventilation. Subgroup analysis of patients with septic shock had similar outcomes in both MAP targets.
Conclusions: In critically ill patients, a higher MAP goal of > 70 mm Hg was associated with a similar risk of mortality, duration of mechanical ventilation, and ICU length of stay when compared with a standard MAP goal of 60 - 70 mm Hg.
Keywords: Mean arterial pressure; Septic shock; Cardiac arrest
| Introduction | ▴Top |
Septic shock or vasodilatory shock and post-cardiac arrest patients contribute to the majority of critically ill patients in the medical intensive care unit (ICU). The current surviving sepsis guidelines recommend targeting a mean arterial pressure (MAP) of 65 mm Hg with no benefit of targeting a higher MAP in septic shock patients [1]. Similarly, the 2010 American Heart Association guidelines recommend a MAP of more than 65 mm Hg for cardiac arrest patients [2]. However, several prospective studies have shown that targeting higher MAP goals were associated with improved neurological outcomes as well as survival among cardiac arrest patients [3-5]. Several studies have shown that a MAP greater than 70 mm Hg may avoid acute kidney injury and improve microcirculation in the setting of septic shock [6-9]. However, randomized controlled trials (RCTs) in critically ill patients so far have failed to show any benefits. We, therefore, performed this meta-analysis of all the available RCT to evaluate whether a higher MAP goal will improve outcomes in critically ill patients.
| Materials and Methods | ▴Top |
Two reviewers (SS and SS) independently searched electronic databases for RCTs comparing standard MAP goals versus a high MAP goal in critically ill medical patients. The studies were included if they met the following criteria: RCTs of adult human subjects, reporting clinical outcomes in critically ill patients who were treated with a higher MAP goal versus a standard MAP goal, reporting at least one clinical outcome of interest. The main exclusion criteria were nonrandomized control trials. A standard MAP goal was defined as a MAP of 60 - 70 mm Hg, and a MAP of 70 mm Hg or more was considered a high MAP goal. From the eligible RCTs, study characteristics including study design, year of publication, inclusion and exclusion criteria, sample size, follow-up period, baseline patient characteristics, treatment data, and clinical outcomes at the longest available follow-up were collected. Outcomes of interest were mortality, duration of mechanical ventilation, and ICU length of stay. Subgroup analysis was performed based on the type of critical care admission; cardiac arrest and septic shock/vasodilatory shock patients.
This meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [10]. We used Cochrane review manager, version 5.4 RevMan for study analysis [11]. For dichotomous clinical data, pooled risk ratio (RR) and 95% confidence intervals (CIs) were calculated using the random-effects models with the Mantel-Haenszel method. For continuous variables, we computed standardized mean difference (SMD) with 95% CI using the inverse variance method. A P value of 0.05 or less was considered statistically significant. Study heterogeneity was assessed by calculating I-squared statistic; heterogeneity was considered significant in the case of I2 > 50%. Mean and standard deviations were extrapolated from median and range using the statistical method outlined by Hozo et al [12]. Forest plots were generated to demonstrate the relative effect size of high MAP goals versus standard MAP goals for individual clinical endpoints.
The Institutional Review Board (IRB) approval was not applicable. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Six RCTs with a total of 3,753 patients (standard MAP goal: n = 1,872 and high MAP goal: n = 1,881) were included in the final study analysis [13-18]. Three studies included septic/vasodilatory shock patients [13-15], and three included post-cardiac arrest patients [16-18]. The 65 Trial (Lamontagne et al, 2020) contributed to 65% of the total study population (2,463 patients) [15]. The duration of follow-up ranged from 1 month to 6 months. Baseline patient characteristics and study inclusion and exclusion criteria are shown in Table 1 [13-18]. The mean age of the study population was 65 in both groups and almost 70% were male. All six trials reported mortality, while four trials reported the duration of mechanical ventilation, and five trials reported ICU length of stay. Out of 3,753, a total of 1,532 patients died, with 740 in the standard MAP group and 792 in the MAP group. Both standard MAP goals and high MAP goals were associated with similar risk for mortality (RR 0.94, 95% CI (0.87, 1.01), P = 0.11) with no evidence of heterogeneity between studies (I2 = 0%) (Fig. 1) [13-18]. Similarly, there was no difference in the duration of mechanical ventilation (SMD 0.51, 95% CI (-0.29, 1.31), P = 0.21) (Fig. 2) [15-18], and ICU length of stay (SMD 0.22, 95% CI (-0.07, 0.5), P = 0.14) (Fig. 3) [13, 15-18], between standard MAP versus high MAP goal but with significant heterogeneity between studies.
 Click to view | Table 1. Baseline Characteristics of the Patients and Characteristics of Trials Included |
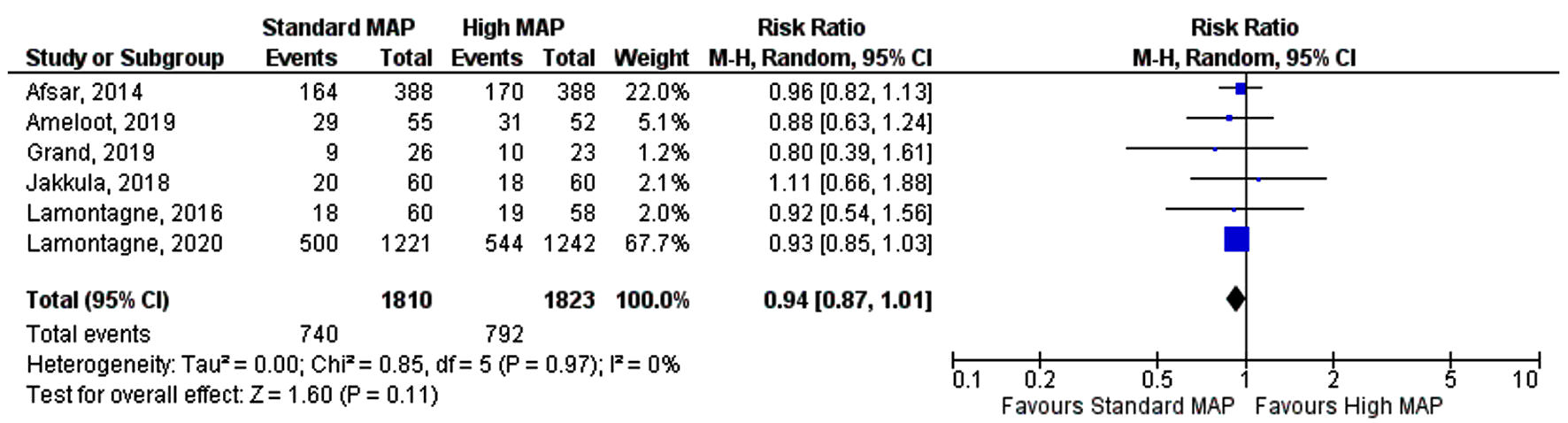 Click for large image | Figure 1. Forest plot showing risk ratio of overall mortality. MAP: mean arterial pressure; CI: confidence interval. |
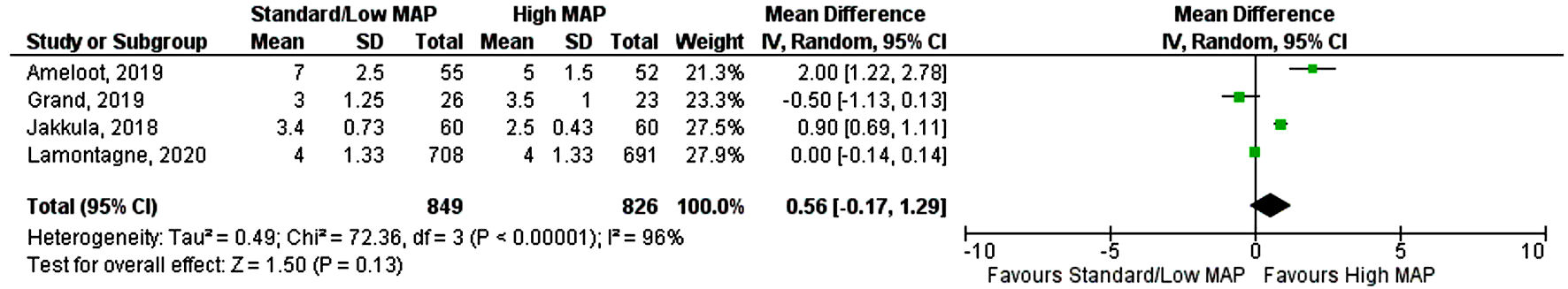 Click for large image | Figure 2. Forest plot showing risk ratio of the duration of mechanical ventilation. MAP: mean arterial pressure; CI: confidence interval. |
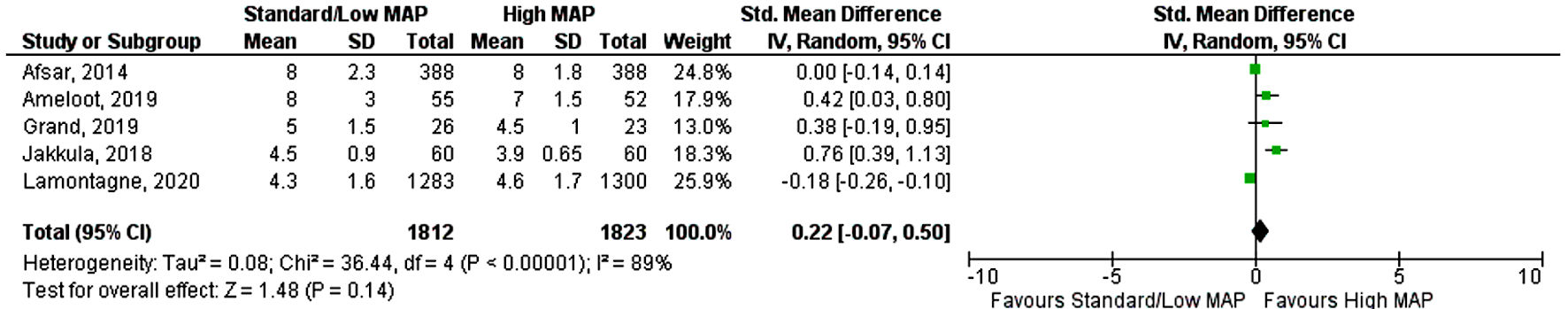 Click for large image | Figure 3. Forest plot showing risk ratio of ICU length of stay. MAP: mean arterial pressure; CI: confidence interval; ICU: intensive care unit. |
Subgroup analysis was performed based on type of critical care admission with 3,357 patients in the septic shock subgroup and only 276 patients included in the cardiac arrest subgroup. Post-cardiac arrest patients with higher MAP goal had a lower duration of ICU stay (SMD 0.55, 95% CI (0.31, 0.80), P < 0.000001, I2 = 2%) when compared to the standard MAP goal (Fig. 4) [13, 15-18]. However, both MAP goals had similar risk of mortality (RR 0.92, 95% CI (0.71, 1.2), P = 0.55) and duration of mechanical ventilation (SMD 0.69, 95% CI (-0.31, 1.69), P = 0.21) (Figs. 5, 6) [13-18]. In patients with septic shock both standard and high MAP goals had a similar risk of mortality (RR 0.92, 95% CI (0.87, 1.02), P = 0.55) and ICU length of stay (SMD -0.10, 95% CI (-0.28, 0.08), P = 0.26) (Figs. 4, 5) [13-18].
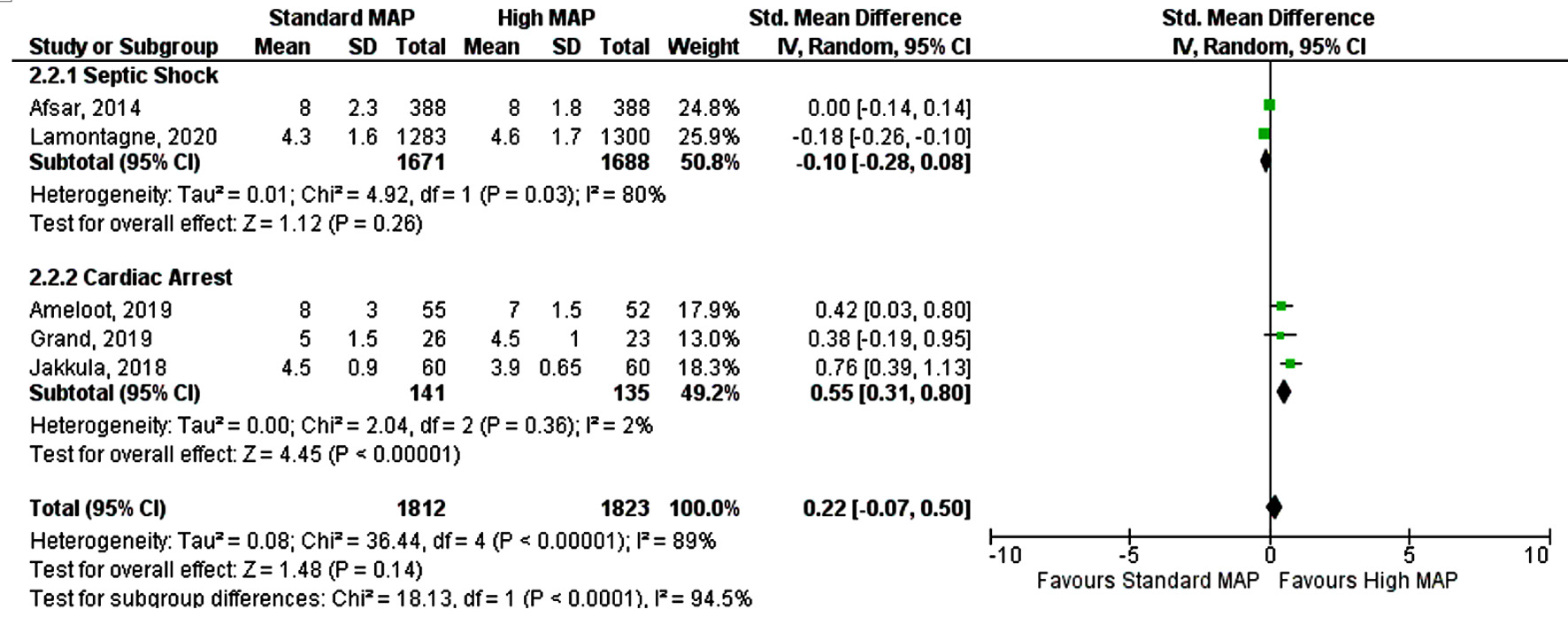 Click for large image | Figure 4. Forest plot showing ICU length of stay by subgroup analysis. MAP: mean arterial pressure; CI: confidence interval; ICU: intensive care unit. |
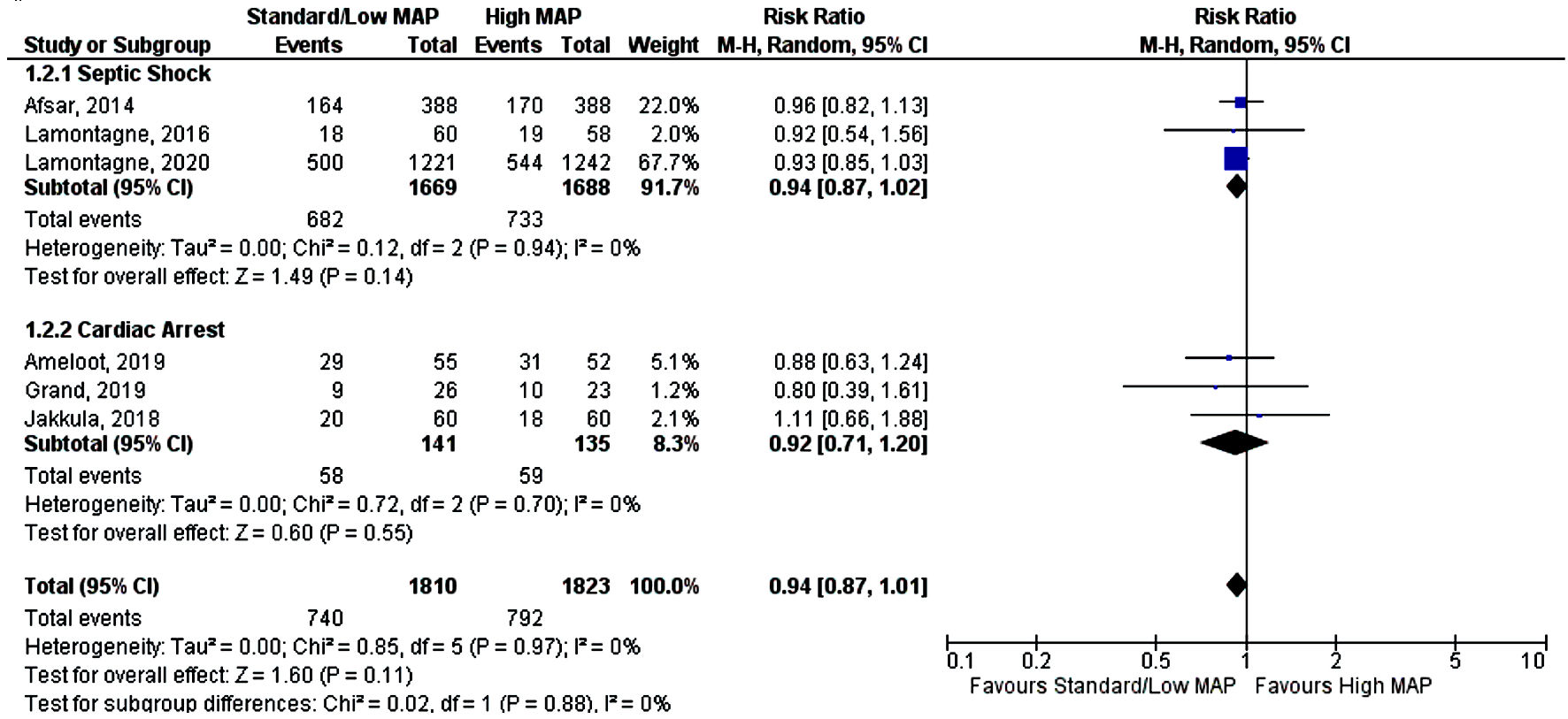 Click for large image | Figure 5. Forest plot showing mortality by subgroup analysis. MAP: mean arterial pressure; CI: confidence interval. |
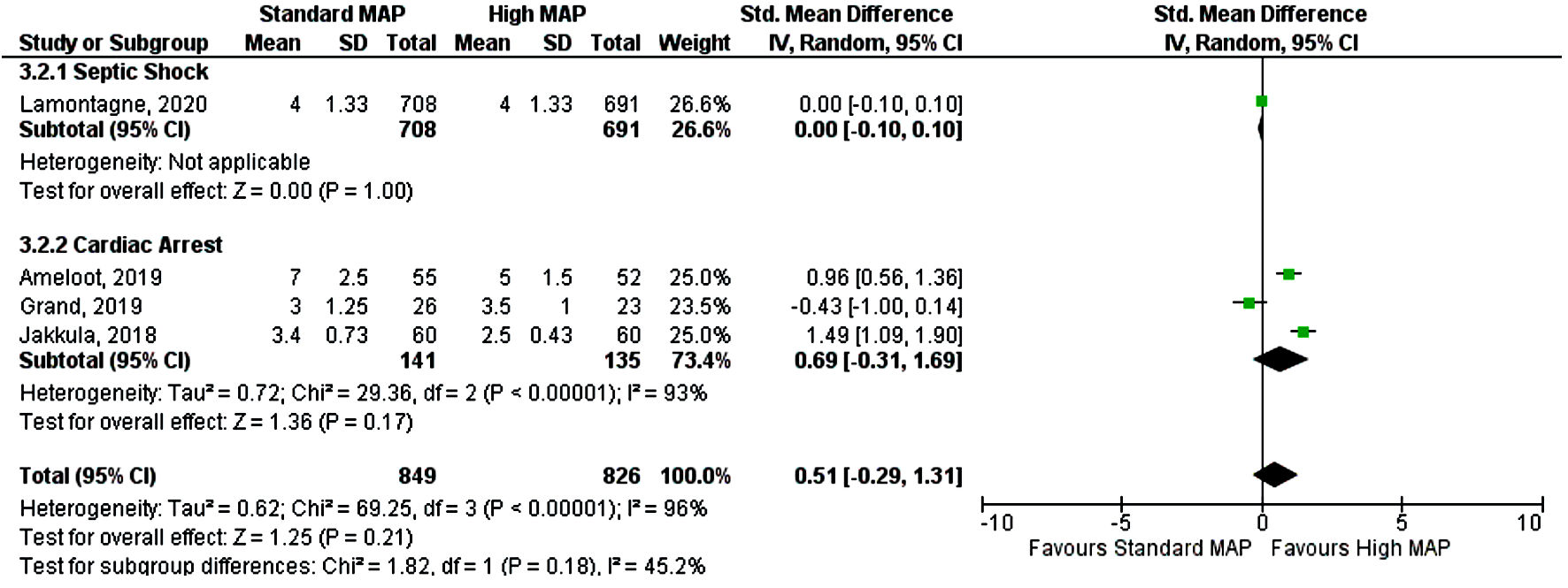 Click for large image | Figure 6. Forest plot showing duration of mechanical ventilation by subgroup analysis. MAP: mean arterial pressure; CI: confidence interval. |
| Discussion | ▴Top |
This meta-analysis of RCTs shows that targeting a high MAP goal in critically ill patients with septic shock and post-cardiac arrest was associated with a similar risk of mortality, duration of mechanical ventilation, and ICU length of stay when compared with standard MAP goal. In patients with chronic hypertension, higher MAP targets have been shown to reduce the rate of acute kidney injury as well as renal replacement therapy [13]. Retrospective studies have shown that MAP less than 80 mm Hg may worsen the myocardial injury and acute kidney injury [19]. A large-scale retrospective study in more than 5,000 patients showed the prolonged duration of MAP below 65 mm Hg to be associated with increased mortality [20]. Despite this, our meta-analysis failed to show any benefits of a high MAP goal in survival. The results of our meta-analysis are in line with the RCTs included in this study. This shows that a specific MAP goal or a one-size-fits-all approach might not be clinically beneficial.
A prior meta-analysis that pooled data from two septic shock RCTs [11, 13] did not find any improvement in overall 28-day survival in the higher MAP group; however, it showed increased mortality with higher MAP group in the elderly patients exposed to vasopressors greater than 6 h [21]. We did not find any increased mortality with a high MAP goal; however, there was a numerical but non-significant increase in mortality in the high MAP group. Further, we were not able to perform age-related analysis because of a lack of data. Subgroup analysis based on the type of ICU admission showed no significant difference in mortality with different MAP goals but there was again a numerical non-significant increase in mortality in the septic shock group. This increase was mainly driven by the 65 Trial (Lamontagne et al, 2020 [15]), which was designed as permissive hypotension versus usual care and found no difference between them. Two of the included post-cardiac arrest RCTs reported improved cerebral oxygenation in the higher MAP group [16, 17]. In one post hoc analysis of these trials, patients with cardiogenic shock-related cardiac arrest with higher MAP goals had a lower area under the troponin T curve suggesting lesser myocardial injury [22]. Though, despite evidence of some benefits the results failed to translate into a significant improvement in clinical outcomes. In the cardiac arrest subgroup, we found that patients with higher MAP had a shorter length of ICU stay compared to patients with standard MAP goals. These results should be interpreted cautiously as the number of patients in this subgroup was limited, length of stay was not a standardized outcome and depend on individual centers. However, this is hypothesis-generating and future studies should aim to identify possible subgroups where higher MAP goals might be beneficial.
The 2015 American Heart Association guidelines modified its recommendation for MAP goal of 65 mm Hg, stating that different organs and individuals may have different optimal pressures leading to the concept of patient-specific optimal MAP goals [23]. Recently a systematic review investigated the concept of cerebral autoregulation to study the role of optimal MAP goals in improving cerebral oxygenation in post-cardiac arrest patients but failed to show any improvement in neurological outcomes [24]. Our findings support current guidelines for targeting a MAP goal of 65 mm Hg in critically ill medical patients [1, 2]. Studies with a focus on improved hemodynamic monitoring and specific end-organ perfusion outcomes are necessary to provide more consistent data. This meta-analysis has some limitation which includes, the presence of a heterogeneous trial population including different MAP goals in both the groups, non-standardized blood pressure monitoring, and a lack of data on end-organ outcomes and biomarkers. Future trials might benefit from more precise hemodynamic monitoring and strict adherence to MAP goals [25]. Newer ongoing RCT, like Optimal VAsopressor TitraTION in patients 65 years and older (OVATION-65 trial) will evaluate the impact of MAP goals specifically on biological markers of end organs, which will likely improve our understanding further [26].
Conclusions
Targeting a high MAP goal in critically ill patients offers no benefits over the current standard MAP goal in terms of mortality, duration of mechanical ventilation, and ICU length of stay.
Acknowledgments
None to declare.
Financial Disclosure
No financial disclosures to declare.
Conflict of Interest
This article has no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Sauradeep Sarkar: conception, design, acquisition of data, and draft writing. Sahib Singh: acquisition of data and draft revising. Amit Rout: statistical analysis and interpretation of data, draft revising.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580-637.
doi pubmed - Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(Suppl 3):18 S768-786.
- Beylin ME, Perman SM, Abella BS, Leary M, Shofer FS, Grossestreuer AV, Gaieski DF. Higher mean arterial pressure with or without vasoactive agents is associated with increased survival and better neurological outcomes in comatose survivors of cardiac arrest. Intensive Care Med. 2013;39(11):1981-1988.
doi pubmed - Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Shea L, Donnino M, Jones C, et al. Association between elevated mean arterial blood pressure and neurologic outcome after resuscitation from cardiac arrest: results from a multicenter prospective cohort study. Crit Care Med. 2019;47(1):93-100.
doi pubmed - Ameloot K, Meex I, Genbrugge C, Jans F, Boer W, Verhaert D, Mullens W, et al. Hemodynamic targets during therapeutic hypothermia after cardiac arrest: A prospective observational study. Resuscitation. 2015;91:56-62.
doi pubmed - Moman RN, Ostby SA, Akhoundi A, Kashyap R, Kashani K. Impact of individualized target mean arterial pressure for septic shock resuscitation on the incidence of acute kidney injury: a retrospective cohort study. Ann Intensive Care. 2018;8(1):124.
doi pubmed - Badin J, Boulain T, Ehrmann S, Skarzynski M, Bretagnol A, Buret J, Benzekri-Lefevre D, et al. Relation between mean arterial pressure and renal function in the early phase of shock: a prospective, explorative cohort study. Crit Care. 2011;15(3):R135.
- Leone M, Asfar P, Radermacher P, Vincent JL, Martin C. Optimizing mean arterial pressure in septic shock: a critical reappraisal of the literature. Crit Care. 2015;19:101.
doi pubmed - Xu JY, Ma SQ, Pan C, He HL, Cai SX, Hu SL, Liu AR, et al. A high mean arterial pressure target is associated with improved microcirculation in septic shock patients with previous hypertension: a prospective open label study. Crit Care. 2015;19:130.
doi pubmed - Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
doi pubmed - Review Manager (RevMan) [Computer program]. Version 5.4. Copenhagen: the Nordic Cochrane Centre, the Cochrane Collaboration. 2014.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
doi pubmed - Asfar P, Meziani F, Hamel JF, Grelon F, Megarbane B, Anguel N, Mira JP, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370(17):1583-1593.
doi pubmed - Lamontagne F, Meade MO, Hebert PC, Asfar P, Lauzier F, Seely AJE, Day AG, et al. Higher versus lower blood pressure targets for vasopressor therapy in shock: a multicentre pilot randomized controlled trial. Intensive Care Med. 2016;42(4):542-550.
doi pubmed - Lamontagne F, Richards-Belle A, Thomas K, Harrison DA, Sadique MZ, Grieve RD, Camsooksai J, et al. Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA. 2020;323(10):938-949.
doi pubmed - Ameloot K, De Deyne C, Eertmans W, Ferdinande B, Dupont M, Palmers PJ, Petit T, et al. Early goal-directed haemodynamic optimization of cerebral oxygenation in comatose survivors after cardiac arrest: the Neuroprotect post-cardiac arrest trial. Eur Heart J. 2019;40(22):1804-1814.
doi pubmed - Jakkula P, Pettila V, Skrifvars MB, Hastbacka J, Loisa P, Tiainen M, Wilkman E, et al. Targeting low-normal or high-normal mean arterial pressure after cardiac arrest and resuscitation: a randomised pilot trial. Intensive Care Med. 2018;44(12):2091-2101.
doi pubmed - Grand J, Meyer AS, Kjaergaard J, Wiberg S, Thomsen JH, Frydland M, Ostrowski SR, et al. A randomised double-blind pilot trial comparing a mean arterial pressure target of 65 mm Hg versus 72 mm Hg after out-of-hospital cardiac arrest. Eur Heart J Acute Cardiovasc Care. 2020;9(4_suppl):S100-S109.
- Maheshwari K, Nathanson BH, Munson SH, Khangulov V, Stevens M, Badani H, Khanna AK, et al. The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients. Intensive Care Med. 2018;44(6):857-867.
doi pubmed - Vincent JL, Nielsen ND, Shapiro NI, Gerbasi ME, Grossman A, Doroff R, Zeng F, et al. Mean arterial pressure and mortality in patients with distributive shock: a retrospective analysis of the MIMIC-III database. Ann Intensive Care. 2018;8(1):107.
doi pubmed - Lamontagne F, Day AG, Meade MO, Cook DJ, Guyatt GH, Hylands M, Radermacher P, et al. Pooled analysis of higher versus lower blood pressure targets for vasopressor therapy septic and vasodilatory shock. Intensive Care Med. 2018;44(1):12-21.
doi pubmed - Ameloot K, Jakkula P, Hastbacka J, Reinikainen M, Pettila V, Loisa P, Tiainen M, et al. Optimum blood pressure in patients with shock after acute myocardial infarction and cardiac arrest. J Am Coll Cardiol. 2020;76(7):812-824.
doi pubmed - Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, et al. Part 8: post-cardiac arrest care: 2015 American Heart Association Guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(Suppl 2):18 S465-482.
- Rikhraj KJK, Wood MD, Hoiland RL, Thiara S, Griesdale DEG, Sekhon MS. Determining optimal mean arterial pressure after cardiac arrest: a systematic review. Neurocrit Care. 2021;34(2):621-634.
doi pubmed - Khanna AK. Defending a mean arterial pressure in the intensive care unit: Are we there yet? Ann Intensive Care. 2018;8(1):116.
doi pubmed - Masse MH, Battista MC, Wilcox ME, Pinto R, Marinoff N, D'Aragon F, St-Arnaud C, et al. Optimal VAsopressor TitraTION in patients 65 years and older (OVATION-65): protocol and statistical analysis plan for a randomised clinical trial. BMJ Open. 2020;10(11):e037947.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


