| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 13, Number 9, September 2021, pages 479-486
Development of a Method for Estimating Dietary Salt Intake Using the Overnight Urinary Sodium/Potassium Ratio
Yuta Sumikamaa, c, Hiroshige Aoyamab, Norifumi Isub, Masaaki Nagatab, Takumi Katoa, Takayoshi Tsukaharaa
aGraduate School of Nutritional Sciences, Nagoya University of Arts and Sciences, Aichi, Japan
bLIXIL Corporation, Tokyo, Japan
cCorresponding Author: Yuta Sumikama, Graduate School of Nutritional Sciences, Nagoya University of Arts and Sciences, 57 Iwasaki-cho, Nisshin, Aichi 470-0196, Japan
Manuscript submitted September 10, 2021, accepted September 29, 2021, published online September 30, 2021
Short title: Method of Estimating Dietary Salt Intake
doi: https://doi.org/10.14740/jocmr4596
| Abstract | ▴Top |
Background: There are many patients who need to restrict and assess salt in their diet. However, it is difficult to estimate daily salt intake accurately and easily. Therefore, a method for estimating dietary salt intake using the overnight urinary sodium (Na)/potassium (K) ratio was developed.
Methods: The study involved 43 healthy adults (13 males, 30 females). From 2018 to 2020, subjects consumed a salt-adjusted diet for 11 - 30 days continuously, and overnight urine was collected daily. Using the previous day’s salt intake as the objective variable, an equation for estimating the salt intake was developed using a general linear model. To verify the accuracy of the estimating equation, the estimated salt intake of the previous day was calculated using our equation and Tanaka’s equation, which is an estimating equation from spot urine widely used in clinical practice and epidemiological studies to estimate dietary salt intake, and they were compared with the actual salt intake.
Results: The results of the analysis showed that model 1 (previous day’s salt intake (g) = 3.62 + 0.64 × urinary Na/K ratio + 0.18 × conductivity (mS/cm) - 0.43 × sex (male 0, female 1)) was the optimal model. Then, salt intake was estimated using model 1 and Tanaka’s equation, and compared with actual salt intake. The Pearson’s product-moment correlation coefficient between the actual and estimated salt intake was r = 0.618 (P < 0.001) and r = 0.573 (P < 0.001) for model 1 estimates and Tanaka’s equation estimates, respectively. The percentages of errors within ±30% from the actual salt intake were 64.2% and 58.4% for model 1 and Tanaka’s equation, respectively.
Conclusion: An equation for estimating salt intake was developed using the Na/K ratio and conductivity of overnight urine. Although the applicability of this method to hypertensive patients and the elderly has not been studied and needs to be clarified in the future, the estimating equation developed is simple and may be a useful method for daily monitoring of dietary salt intake.
Keywords: Salt intake; Na/K ratio; Sodium; Potassium; Urine
| Introduction | ▴Top |
The relationship between salt intake and blood pressure has been reported by many epidemiological studies [1, 2], and excessive salt intake is a risk factor for cardiovascular disease and stomach cancer [2-6]. In addition, some intervention studies have demonstrated that reducing dietary salt intake lowers blood pressure [7-9], and salt restriction is recommended in guidelines for hypertension [10].
One of the barriers to successful salt restriction is the difficulty in estimating dietary salt intake. The gold standard for estimating an individual’s daily salt intake is the 24-h urine collection method [11, 12], but this method is not suitable for daily monitoring because of the high burden on patients. Several other simple methods for estimating salt intake by spot urine have been reported [13-15], but they are not recommended because of their low accuracy for individual estimation [16]. In addition, estimation by spot urine requires measurement of creatinine (Cr), which is difficult to measure at home and therefore cannot be used for daily monitoring. There are methods for estimating salt intake at home using electrical conductivity (conductivity), but these methods have problems in daily monitoring, such as overestimation of salt intake due to increased potassium (K) intake and the need to collect whole urine [17].
The Na/K ratio, which is calculated by dividing the urinary sodium (Na) concentration by the K concentration, is being used in medical examinations as an index to evaluate daily dietary content [18, 19]. The World Health Organization (WHO) recommends a decrease in salt intake and an increase in K intake and suggests that the guideline-targeted Na and K intake levels would yield a Na/K molar ratio of approximately 1.0 [20, 21]. Furthermore, the urinary Na/K ratio can be easily measured by a portable device. Thus, we investigated an equation for estimating dietary salt intake using the overnight urinary Na/K ratio as a simple measurement without the need for Cr measurements for daily monitoring. In our previous study, we developed an equation for estimating salt intake, but the range of possible estimates was too narrow, and the equation tended to overestimate the low-salt zone [22]. One of the reasons for the overestimation was thought to be the lack of data for low-salt meals, so this study was conducted to improve the accuracy of the estimating equation by adding data for low-salt meals.
| Materials and Methods | ▴Top |
Subjects
This study included 43 healthy adults (13 males, 30 females) who were recruited from 2018 to 2020. Of the 43 volunteers, 31 were recruited from students at Nagoya University of Arts and Sciences and 12 were recruited from the general population at HUMA R&D Corp. (Tokyo, Japan). The participants were healthy volunteers without hypertension, kidney disease, or other known diseases, and who were not taking regular medication. Smokers were excluded from this study. Weight and blood pressure were measured daily during the study period to confirm that there were no fluctuations. This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Research Ethics Committee of Nagoya University of Arts and Sciences (186, 234, 242, 338, and 437).
Intake of salt formula diet
The subjects consumed a salt-adjusted meal for 11 - 30 days. The amount of salt was adjusted every few days in the range of 2 - 19 g. All nutrient intakes were calculated by confirming nutrient amounts from the Standard Tables of Food Composition in Japan 2015 (seventh revised edition) or from food packaging. The meals were cooked with all ingredients strictly weighed, and the subjects consumed everything completely, including seasonings, sauce and soup. Additional and reduced dietary intakes were allowed only if the exact amount of the nutrient was known, and all these intakes were recorded. Consumption of alcohol was prohibited during this study.
Urine collection and measurement
The overnight urine, which is the first morning voided urine, was collected daily. The Na concentration, K concentration, Na/K ratio, and Cr concentration in the collected urine samples were measured at the Nagoya Medical Cooperative Association Nagoya Clinical Laboratory Center. Specific gravity was measured using a PAL-09S (ATAGO Co., Ltd, Tokyo, Japan), and the conductivity was measured using a LAQUAtwin <EC-33B> (HORIBA Ltd, Kyoto, Japan). In addition, urine weight was measured.
Statistical analysis
The following variables were used for analysis in this study: previous day’s salt intake, urinary Na, K, and Cr concentrations, urinary Na/K ratio, conductivity, specific gravity, urine weight, height, body weight, body mass index (BMI), age, and sex. Data are expressed as means ± standard deviation (SD), with differences between the two groups examined for significance using Student’s t-test or Mann-Whitney U test. The association between each variable was determined using Pearson’s product-moment correlation coefficient. Using the previous day’s salt intake as the objective variable, an equation for estimating salt intake was developed using a general linear model. To verify the accuracy of the estimating equation, the estimated salt intake of the previous day was calculated using our equation and Tanaka’s equation [13], and the results were compared with the actual measured salt intake. All analyses were performed using R version 4.0.3. P values < 0.05 were considered significant.
| Results | ▴Top |
Subjects’ characteristics
The characteristics of the subjects are shown in Table 1. All subjects completed this study. The average age of the 43 subjects, which included 13 males and 30 females, was 28.2 ± 10.8 years overall, 32.9 ± 13.0 years for males, and 26.2 ± 9.3 years for females (P-value between males and females = 0.008). Height and weight were both significantly higher in males than in females (P < 0.001 for both). The BMI was not significantly different between males and females.
 Click to view | Table 1. Characteristics, Urinary Findings and Dietary Salt Intakes of Study Subjects |
Salt intake and urine measurements
Salt intake and urine measurements are shown in Table 1. Salt intake was 8.44 ± 3.42 g overall, 7.91 ± 3.54 g in males, and 8.62 ± 3.36 g in females (P = 0.006). There were significant differences in urinary Na concentration, urinary Na/K ratio, and conductivity between males and females (all P < 0.001). There was no difference in urinary K concentration and specific gravity between males and females.
Equation for estimating salt intake using the overnight urinary Na/K ratio
Pearson’s product-moment correlation coefficient was calculated for each variable (previous day’s salt intake, urinary Na/K ratio, urinary Na concentration, urinary K concentration, conductivity, specific gravity, urine weight, height, weight, and age). Results are shown as a correlation matrix between each of the variables (Table 2). The urinary Na/K ratio and conductivity were significantly positively related to the previous day’s salt intake (r = 0.522, P < 0.001 and r = 0.433, P < 0.001, respectively). Since there were significant differences in the urinary Na/K ratio and conductivity between sexes, a regression equation to estimate the previous day’s salt intake was developed using a general regression model with urinary Na/K ratio, conductivity, and sex as explanatory variables. The results of the analysis showed that model 1 (previous day’s salt intake (g) = 3.62 + 0.64 × urinary Na/K ratio + 0.18 × conductivity (mS/cm) - 0.43 × sex (male 0, female 1)) was the optimal model (Table 3).
 Click to view | Table 2. Correlation Matrix of Measurements |
 Click to view | Table 3. Regression Equation for Estimating the Previous Day’s Salt Intake From Na/K Ratio |
Relationship between the value obtained by the estimating equation and the actual measured value
Table 4 presents actual salt intake and the estimated values calculated by model 1 or Tanaka’s equation. The mean ± SD values of the actual salt intake, the model 1 estimate, and Tanaka’s equation estimate were 8.44 ± 3.42 g, 8.51 ± 2.13 g, and 7.14 ± 1.79 g, respectively. The medians (interquartile range) were 8.70 (5.80 - 10.73) g, 8.12 (6.85 - 9.75) g, and 7.02 (5.87 - 8.25) g, respectively. Model 1 was closer to the actual salt intake in the high salt zone (75th percentile), but overestimated the values in the low salt zone (25th percentile). On the other hand, Tanaka’s equation was closer to the actual salt intake in the low-salt zone, but underestimated the value in the high-salt zone. Pearson’s product-moment correlation coefficient between the actual and estimated salt intake was r = 0.618 (P < 0.001) and r = 0.573 (P < 0.001) for the model 1 estimate and Tanaka’s equation estimate, respectively. The percentages of errors within ±30% from the actual salt intake were 64.2% and 58.4% for model 1 and Tanaka’s equation, respectively (Fig. 1). The percentages of errors within ± 1.0 g from the actual salt intake were 25.0% and 25.6% for model 1 and Tanaka’s equation, respectively (Fig. 1).
 Click to view | Table 4. Comparison of Measured and Estimated Previous Day’s Salt Intake |
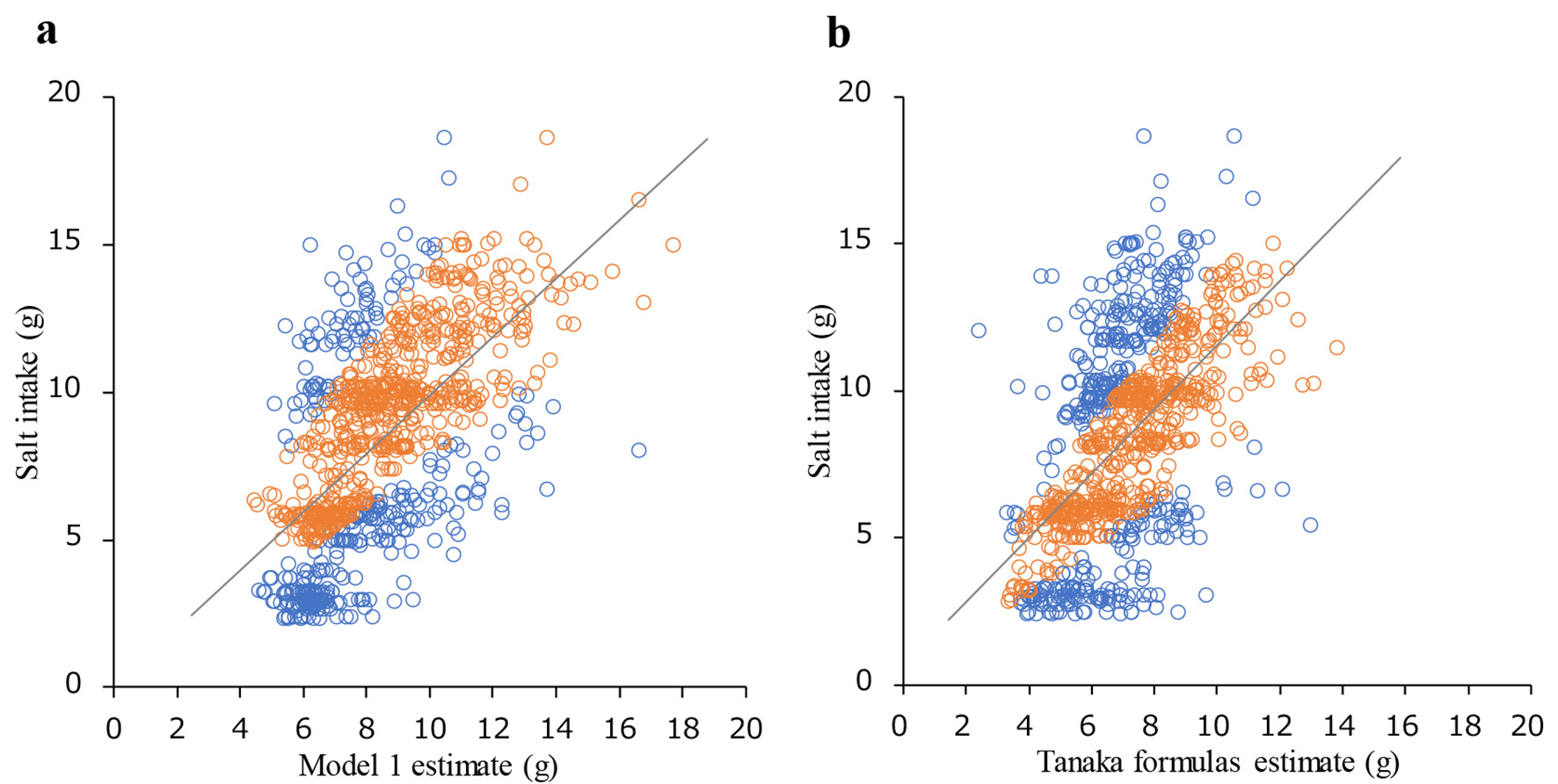 Click for large image | Figure 1. Relationship between measured and estimated previous day’s salt intake. (a) Relationship between salt intake estimated by model 1 and actual salt intake. (b) Relationship between salt intake estimated by Tanaka formulas and actual salt intake. Blue plot: relative difference > 30%, orange plot: relative difference ≤ 30%. The percentages of relative difference ≤ 30% for model 1 and Tanaka formulas were 64.2% and 58.4%, respectively. The percentages of absolute difference ≤ 1 g for model 1 and Tanaka formulas were 25.0% and 25.6%, respectively. |
| Discussion | ▴Top |
A regression equation to estimate the previous day’s salt intake using a general regression model with the urinary Na/K ratio, conductivity, and sex as explanatory variables was developed. Model 1 (previous day’s salt intake (g) = 3.62 + 0.64 × urinary Na/K ratio + 0.18 × conductivity (mS/cm) - 0.43 × sex (males 0, females 1)) was found to be the optimal model.
There is diurnal variation in urinary Na and K excretion and the urinary Na/K ratio [23]. Cogswell et al [24] reported that the estimation of salt intake using spot urine varied depending on the timing of urine collection. Thus, the accuracy of these estimating equations may depend on the timing of collection. Therefore, in this study, an estimating equation limited to overnight urine was developed, considering the variability of the estimate due to this diurnal variation. Overnight urine may be useful for daily monitoring because it has a longer urine storage time and is often voided at home or in a limited location for each individual.
In the present study, not only the urinary Na/K ratio, but also the conductivity was used as an explanatory variable in the estimating equation. Conductivity is an indicator that reflects the concentration of electrolytes in a substance and can be used to measure the concentration of electrolytes in urine. A simple measurement device for estimating salt intake using overnight urine conductivity has been developed by Yamasue et al [17]. However, this device calculates the urinary Na and K excretion ratio as 7:3 (Na/K ratio 2.3) because the conductivity cannot measure urinary Na and K separately. Therefore, if the Na and K intake ratio deviates from this assumption, it becomes an error factor in the estimation of salt intake. The use of two variables in the estimating equation of this study, urinary Na/K, which decreases with increasing K intake, and conductivity, which increases, may reduce the error due to K intake.
The estimating equation developed in this study was compared with Tanaka’s equation to verify its accuracy. Tanaka’s equation was developed using data from 591 Japanese individuals and is now widely used in clinical practice and epidemiological studies to estimate dietary salt intake [25, 26]. Pearson’s product-moment correlation coefficient between the actual salt intake and estimated salt intake was r = 0.618 (P < 0.001) and r = 0.573 (P < 0.001) for the model 1 equation estimates and Tanaka’s equation estimates, respectively. The percentages of errors within ±30% from the actual salt intake were 64.2% and 58.4% for model 1 and Tanaka’s equation, respectively. Zhou et al [16] reported that the percentage of errors within ±30% for the three estimating equations, Tanaka’s equation, Kawasaki’s equation, and the INTERSALT equation, were 64.5%, 57.4%, and 41.8%, respectively, in a Chinese population. Cogswell et al [24] reported that the correlation between estimated and measured 24-h urinary sodium excretion using Tanaka’s equation with overnight urine was r = 0.47 in 406 residents of Washington. Model 1 developed in the present study had accuracy equal to or better than the accuracy of Tanaka’s equation reported in previous studies. Zhou et al [16] reported that, among the three estimating equations, Tanaka’s equation, Kawasaki’s equation, and the INTERSALT equation, Tanaka’s equation had the lowest error in the Chinese population, whereas Mayer et al [27] reported that the INTERSALT equation had the lowest error in the Norwegian population. Thus, the accuracy of the estimating equation varies depending on the validation population. Tanaka’s equation was developed in the Japanese population, which has a relatively high salt intake, whereas the INTERSALT equation was developed in the Western population, which has a relatively low salt intake. Therefore, the estimation accuracy of the estimating equation may depend on the average salt intake of the population to be estimated.
The medians (interquartile range) of the actual salt intake, the model 1 equation estimates, and Tanaka’s equation estimates were 8.70 (5.80 - 10.73) g, 8.12 (6.85 - 9.75) g, and 7.02 (5.87 - 8.25) g, respectively. Model 1 was closer to the actual values in the high salt zone (75th percentile), but overestimated the values in the low salt zone (25th percentile). In contrast, Tanaka’s equation was closer to the actual value in the low-salt zone, but underestimated the value in the high-salt zone. Estimating equations based on spot urine tend to overestimate in the low-salt zone and underestimate in the high-salt zone, because the range of possible estimates is narrow, and the estimated values are close to the mean value [28]. The same trend was observed in the present study. One of the reasons why the estimated low-salt zone by Tanaka’s equation was close to the actual value is that the median of the estimated value was lower than the actual value. Furthermore, Tanaka’s equation is a nonlinear estimating equation, whereas model 1 is a linear estimating equation. Model 1, which is linear, may overestimate the low salt zone because there is an intercept. It is necessary to examine the estimating equation from this point of view in the future.
One of the strengths of this study is the development of an equation for estimating salt intake using actual salt intake, rather than the amount of Na excretion by 24-h urine collection. The equations of the previous study for estimating salt intake from spot urine, such as Tanaka’s and Kawasaki’s equations, estimate salt intake by a 24-h sodium excretion estimate. Although 24-h urine collection is considered the gold standard for estimating salt intake, the correlation between salt intake and estimates from a single 24-h urine collection is approximately r = 0.7, and differences occur between intake and excretion [29]. To omit this gap, an estimating equation was developed using actual salt intake as the objective variable in the present study, which may reduce the error in the process of calculating salt intake.
Second, the formula in this study is simple and easy to use for daily monitoring. Takada et al showed that daily monitoring using a simple urine salt analyzer was effective in reducing salt intake and lowering blood pressure [30]. If a urine measurement device using the equation in this study is developed, it may be useful as a daily home monitoring tool. Previous studies have reported a linear association between cardiovascular disease events and estimated sodium intake using multiple 24-h urine collections, the gold standard for salt intake estimation [31-33]. On the other hand, WHO has recommended reducing salt intake as a population approach not only in individuals with hypertension but also in individuals without hypertension [20]. Therefore, daily monitoring of salt intake in individuals without hypertension may contribute to the reduction of the risk for hypertension and cardiovascular disease in the general population.
However, there are some limitations in this study. First, in this study, data from persons aged 28.2 ± 10.8 years were used to develop the estimating equation, which is a narrow age range with many young people. Although the prevalence of hypertension increases with aging, the applicability of the estimating equation developed in the present study has not yet been validated in patients older than the subjects in this study. Several previous studies have reported higher overnight urinary Na excretion in hypertensive patients and patients with chronic kidney disease [34-36]. On the other hand, these previous studies also reported higher overnight urinary K excretion in these patients. Iwahori et al have observed the diurnal variation of Na/K ratio in 122 participants and reported that diurnal variations in urinary Na/K ratios were comparable between normotensive and hypertensive individuals, and among age and gender-specific subgroups [23]. There may not have been a difference in the Na/K ratio because the overnight urinary excretion of both Na and K is increased in hypertensive patients. Therefore, it may be applicable to these patients. We have not investigated the applicability of our estimating equation to hypertensive patients or elderly patients, so it is necessary to clarify its applicability in the future.
Second, there is insufficient validation of accuracy in external populations. Tanaka’s equation and Kawasaki’s equation were validated with external populations in their development [13, 14]. In the present study, accuracy validation was conducted using data from the population for which the estimating equation was developed, so the estimating equation may have been overfitted. Finally, the effect of K intake has not been investigated. The urinary Na/K ratio decreases with increasing K intake. However, to what extent increased K intake decreases the urinary Na/K ratio is unknown because increased K intake enhances Na excretion [37]. In contrast, conductivity increases with increasing K intake. Therefore, whether the present estimating equation will underestimate due to increased K intake is not known. Further studies are needed to investigate the effects of K intake.
Accurate salt intake estimation requires 24-h urine collection [11, 12], but this is a burden on the patient, and incomplete collection is a problem [38, 39]. In addition, several estimating equations by spot urine have been developed [13-15], but these equations are difficult to measure at home because they require Cr measurement and are not suitable for daily monitoring. However, the Na/K ratio and conductivity used in the present estimating equation can be easily measured at home. Therefore, although there are some limitations in the present estimating equation, it can be used for daily monitoring of patients who require salt restriction, and it can contribute to improving the adherence of patients to salt restriction.
Conclusion
An equation for estimating salt intake was developed using the Na/K ratio and conductivity of overnight urine without the need for Cr measurement. This estimating equation is simple and may be a useful method for daily monitoring of dietary salt intake.
Acknowledgments
The authors would like to thank all of the subjects who graciously took part in this study despite having to contend with undergoing long-term strict dietary intake and daily urine collection.
Financial Disclosure
This study was conducted in collaboration with LIXIL Corporation.
Conflict of Interest
HA, NI and MN were employees of LIXIL Corporation at the time of the studies.
Informed Consent
Written informed consent was obtained from all study participants.
Author Contributions
HA, NI and TT designed the study; HA, YS and TK performed the data acquisition and analysis; all authors contributed to the interpretation of the data. YS drafted the manuscript and TT contributed in revising the manuscript critically for important intellectual content. All authors agree to the submission of this paper.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297(6644):319-328.
doi pubmed - Mente A, O'Donnell M, Rangarajan S, McQueen M, Dagenais G, Wielgosz A, Lear S, et al. Urinary sodium excretion, blood pressure, cardiovascular disease, and mortality: a community-level prospective epidemiological cohort study. Lancet. 2018;392(10146):496-506.
doi - Wang YJ, Yeh TL, Shih MC, Tu YK, Chien KL. Dietary Sodium Intake and Risk of Cardiovascular Disease: A Systematic Review and Dose-Response Meta-Analysis. Nutrients. 2020;12(10):2934.
doi pubmed - Mente A, O'Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, Diaz R, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388(10043):465-475.
doi - O'Donnell MJ, Yusuf S, Mente A, Gao P, Mann JF, Teo K, McQueen M, et al. Urinary sodium and potassium excretion and risk of cardiovascular events. JAMA. 2011;306(20):2229-2238.
doi pubmed - Tsugane S, Sasazuki S, Kobayashi M, Sasaki S. Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer. 2004;90(1):128-134.
doi pubmed - He FJ, Marciniak M, Visagie E, Markandu ND, Anand V, Dalton RN, MacGregor GA. Effect of modest salt reduction on blood pressure, urinary albumin, and pulse wave velocity in white, black, and Asian mild hypertensives. Hypertension. 2009;54(3):482-488.
doi pubmed - He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325.
doi pubmed - He FJ, MacGregor GA. Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens. 2002;16(11):761-770.
doi pubmed - Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269-1324.
doi pubmed - Dennis B, Stamler J, Buzzard M, Conway R, Elliott P, Moag-Stahlberg A, Okayama A, et al. INTERMAP: the dietary data—process and quality control. J Hum Hypertens. 2003;17(9):609-622.
doi pubmed - Rose G, Stamler J. The INTERSALT study: background, methods and main results. INTERSALT Co-operative Research Group. J Hum Hypertens. 1989;3(5):283-288.
- Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16(2):97-103.
doi pubmed - Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20(1):7-14.
doi pubmed - Brown IJ, Dyer AR, Chan Q, Cogswell ME, Ueshima H, Stamler J, Elliott P, et al. Estimating 24-hour urinary sodium excretion from casual urinary sodium concentrations in Western populations: the INTERSALT study. Am J Epidemiol. 2013;177(11):1180-1192.
doi pubmed - Zhou L, Tian Y, Fu JJ, Jiang YY, Bai YM, Zhang ZH, Hu XH, et al. Validation of spot urine in predicting 24-h sodium excretion at the individual level. Am J Clin Nutr. 2017;105(6):1291-1296.
doi pubmed - Yamasue K, Tochikubo O, Kono E, Maeda H. Self-monitoring of home blood pressure with estimation of daily salt intake using a new electrical device. J Hum Hypertens. 2006;20(8):593-598.
doi pubmed - Iwahori T, Ueshima H, Ohgami N, Yamashita H, Miyagawa N, Kondo K, Torii S, et al. Effectiveness of a self-monitoring device for urinary sodium-to-potassium ratio on dietary improvement in free-living adults: a randomized controlled trial. J Epidemiol. 2018;28(1):41-47.
doi pubmed - Kogure M, Nakaya N, Hirata T, Tsuchiya N, Nakamura T, Narita A, Suto Y, et al. Sodium/potassium ratio change was associated with blood pressure change: possibility of population approach for sodium/potassium ratio reduction in health checkup. Hypertens Res. 2021;44(2):225-231.
doi pubmed - WHO. Guidelinee: Sodium intake for adults and children. 2012.
- WHO. Guideline: potassium intake for adults and children. Geneva: World Health Organization, Department of Nutrition for Health and Development. 2012.
- Kato T, Aoyama H, Isu N et al. Estimation of salt intake based on Na/K ratio in overnight urine sample. Nagoya Journal of Nutritional Sciences. 2021 (in press).
- Iwahori T, Ueshima H, Torii S, Saito Y, Kondo K, Tanaka-Mizuno S, Arima H, et al. Diurnal variation of urinary sodium-to-potassium ratio in free-living Japanese individuals. Hypertens Res. 2017;40(7):658-664.
doi pubmed - Cogswell ME, Wang CY, Chen TC, Pfeiffer CM, Elliott P, Gillespie CD, Carriquiry AL, et al. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18-39 y. Am J Clin Nutr. 2013;98(6):1502-1513.
doi pubmed - Jensen PN, Bao TQ, Huong TTT, Heckbert SR, Fitzpatrick AL, LoGerfo JP, Ngoc TLV, et al. The association of estimated salt intake with blood pressure in a Viet Nam national survey. PLoS One. 2018;13(1):e0191437.
doi pubmed - Yasutake K, Moriguchi R, Kajiyama T, Miyazaki H, Abe S, Masuda T, Imai K, et al. Interannual study of spot urine-evaluated sodium excretion in young Japanese women. J Clin Hypertens (Greenwich). 2017;19(7):653-660.
doi pubmed - Meyer HE, Johansson L, Eggen AE, Johansen H, Holvik K. Sodium and potassium intake assessed by spot and 24-h urine in the population-based Tromso study 2015-2016. Nutrients. 2019;11(7).
doi pubmed - He FJ, Ma Y, Campbell NRC, MacGregor GA, Cogswell ME, Cook NR. Formulas to estimate dietary sodium intake from spot urine alter sodium-mortality relationship. Hypertension. 2019;74(3):572-580.
doi pubmed - Lerchl K, Rakova N, Dahlmann A, Rauh M, Goller U, Basner M, Dinges DF, et al. Agreement between 24-hour salt ingestion and sodium excretion in a controlled environment. Hypertension. 2015;66(4):850-857.
doi pubmed - Takada T, Imamoto M, Sasaki S, Azuma T, Miyashita J, Hayashi M, Fukuma S, et al. Effects of self-monitoring of daily salt intake estimated by a simple electrical device for salt reduction: a cluster randomized trial. Hypertens Res. 2018;41(7):524-530.
doi pubmed - Mills KT, Chen J, Yang W, Appel LJ, Kusek JW, Alper A, Delafontaine P, et al. Sodium excretion and the risk of cardiovascular disease in patients with chronic kidney disease. JAMA. 2016;315(20):2200-2210.
doi pubmed - Cook NR, Appel LJ, Whelton PK. Sodium intake and all-cause mortality over 20 years in the trials of hypertension prevention. J Am Coll Cardiol. 2016;68(15):1609-1617.
doi pubmed - Olde Engberink RHG, van den Hoek TC, van Noordenne ND, van den Born BH, Peters-Sengers H, Vogt L. Use of a single baseline versus multiyear 24-hour urine collection for estimation of long-term sodium intake and associated cardiovascular and renal risk. Circulation. 2017;136(10):917-926.
doi pubmed - Bankir L, Bochud M, Maillard M, Bovet P, Gabriel A, Burnier M. Nighttime blood pressure and nocturnal dipping are associated with daytime urinary sodium excretion in African subjects. Hypertension. 2008;51(4):891-898.
doi pubmed - Miura T, Fukuda M, Naito T, Togawa H, Sato R, Sasagawa Y, Tomonari T, et al. Circadian rhythm of urinary potassium excretion in patients with CKD. Clin Nephrol. 2012;78(3):169-173.
doi pubmed - Dyer AR, Martin GJ, Burton WN, Levin M, Stamler J. Blood pressure and diurnal variation in sodium, potassium, and water excretion. J Hum Hypertens. 1998;12(6):363-371.
doi pubmed - Terker AS, Zhang C, McCormick JA, Lazelle RA, Zhang C, Meermeier NP, Siler DA, et al. Potassium modulates electrolyte balance and blood pressure through effects on distal cell voltage and chloride. Cell Metab. 2015;21(1):39-50.
doi pubmed - Mann SJ, Gerber LM. Addressing the problem of inaccuracy of measured 24-hour urine collections due to incomplete collection. J Clin Hypertens (Greenwich). 2019;21(11):1626-1634.
doi pubmed - John KA, Cogswell ME, Campbell NR, Nowson CA, Legetic B, Hennis AJ, Patel SM. Accuracy and usefulness of select methods for assessing complete collection of 24-hour urine: a systematic review. J Clin Hypertens (Greenwich). 2016;18(5):456-467.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


