| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Original Article
Volume 12, Number 11, November 2020, pages 699-704
Relationship Between Gastroesophageal Reflux Disease and Endoscopic Finding “Iodine-Unstained Streak”
Kazu Hamadaa, b, Tohru Itohb, Ken Kawaurab, Hidekazu Kitakatab, Hiroaki Kunob, Junji Kamaib, Rika Kobayasib, Sadahumi Azukisawab, Taishi Ishisakaa, Yuta Igarashia, Kumie Koderaa, Tazuo Okunoa, Takuro Moritaa, Taroh Himenoa, Hiroshi Yanoa, Toshihiro Higashikawaa, Osamu Iritania, Kunimitsu Iwaia, Shigeto Morimotoa, Masashi Okuroa, c
aDepartment of Geriatric Medicine, Kanazawa Medical University, Uchinada, Kahoku-gun, Ishikawa 920-0293, Japan
bDepartment of Gastroenterological Endoscopy, Kanazawa Medical University, Uchinada, Kahoku-gun, Ishikawa 920-0293, Japan
cCorresponding Author: Masashi Okuro, Kanazawa Medical University, Uchinada, Kahoku-gun, Ishikawa 920-0293, Japan
Manuscript submitted August 24, 2020, accepted September 22, 2020, published online November 3, 2020
Short title: GERD and “Iodine-Unstained Streak”
doi: https://doi.org/10.14740/jocmr4331
| Abstract | ▴Top |
Background: Esophagogastroduodenoscopy (EGD) with iodine stain is a useful and diffused method for diagnosing esophageal cancer. We can perform the procedure easily with endoscopic system which does not comprise image-enhanced endoscopy. Several studies advocated that iodine-unstained streaks are a characteristic finding of gastroesophageal reflux disease (GERD). However, there are only a few reports about the subject. In this study, we investigated the usefulness of iodine chromoendoscopy for GERD consultation.
Methods: The study was conducted with 154 GERD cases in which EGD with iodine stain to the esophagus was performed. For the 154 cases, we analyzed the existence of reflux esophagitis finding and iodine-unstained streaks. In 47 GERD cases (proton pump inhibitor (PPI): 45 cases, histamine H2-receptor antagonist (H2-RA): two cases) where medication was started after EGD, we examined predictive factors of the symptom improvement such as sex, age, weight, reflux esophagitis finding, and iodine-unstained streak.
Results: An iodine-unstained streak was observed in 50/154 cases (32.5%). For 50 cases with iodine-unstained streak, there were only 24/50 cases (48.0%) that had both reflux esophagitis findings (≥ Los Angeles classification: grade M) and an iodine-unstained streak. For 47 cases in which medication was started, 34 cases showed improvement in their symptoms, and 13 cases did not show improvement. An iodine-unstained streak was observed more often in “Improved” group rather than in “Not improved” group (P < 0.01). When we supposed an iodine-unstained streak to be the predictive factor of the medication effect for GERD, sensitivity was 61.8% and specificity was 84.6%.
Conclusions: No erosion was often found in the GERD cases without reflux esophagitis, and iodine-unstained streak was observed more often in “Improved” group rather than in “Not improved” group. We think that iodine-unstained streak can be useful for diagnosing of GERD and predictive factor of the medication effect.
Keywords: Esophagogastroduodenoscopy; Gastroesophageal reflux disease; Iodine-unstained streak; Gastric secretion inhibitor
| Introduction | ▴Top |
Gastroesophageal reflux disease (GERD) is the disease mainly caused by reflux of gastric acid. Because of the reduced Helicobacter pylori infection rate and the increased gastric acid secretion ability, the GERD prevalence increased in late years. GERD is a benign disorder but a disease that could trigger Barrett esophagus and esophagus adenocarcinoma. In addition, it is known that GERD causes symptoms other than in esophagus such as chronic coughing, asthma, and sleep disorder [1, 2].
Esophagogastroduodenoscopy (EGD) is one of the important tools for diagnosing GERD, but we often encounter symptomatic GERD cases without esophagitis finding in ordinary white light imaging, which is called non-erosive reflux disease (NERD). There is a report that mentions only around 24% of the symptomatic GERD cases have esophagitis finding in EGD [3]. In addition, there are many asymptomatic GERD cases having esophagitis findings in EGD, which is called NERD.
An iodine stain is an endoscopic technique which is examined to be a useful method for GERD diagnosis. An iodine stain is widely used as a classic and standard technique in which we can use for the endoscopy system without image-enhanced endoscopy (IEE), such as narrow band imaging (NBI) and blue laser imaging (BLI). When the normal esophageal mucosa reacts to iodine solution, it quickly changes to a dark brown color because glycogen rich in the prickle-cell layer reacts with iodine. An iodine stain is not seen in the lesion that lacks of a normal prickle cell layer, such as in esophageal dysplasia, and cancer [4]. We can recognize them as “iodine-unstained streak” by iodine chromoendoscopy, so it is a useful and diffused method for diagnosing of esophageal cancer. On the other hand, it is known that an iodine-unstained streak is observed not only in esophageal neoplasia but also in GERD with mucosal break or regenerative epithelium [4]. Several advocated that iodine-unstained streaks are characteristic findings of NERD [5, 6], but there are only a few reports about it. In this study, we investigated the usefulness of iodine chromoendoscopy for GERD examination.
| Materials and Methods | ▴Top |
Iodine-unstained streak
In general, the normal esophageal mucosa changes into a uniform dark brown color when it reacts to iodine solution (Fig. 1a).
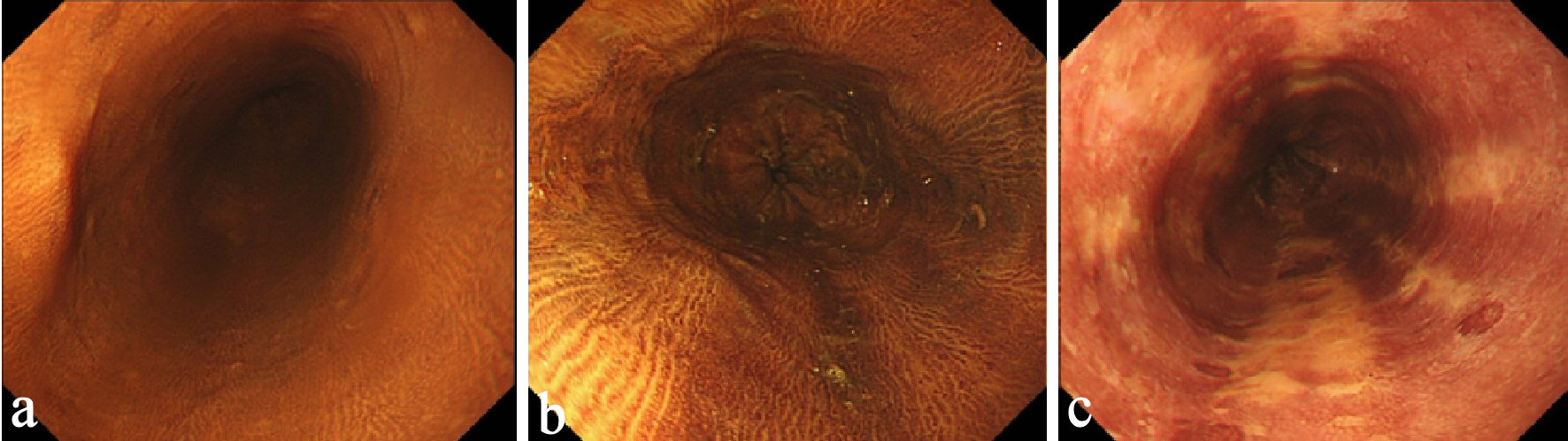 Click for large image | Figure 1. Findings of iodine chromoendoscopy (esophageal mucosa; non-carcinoma) (a) Normal. The normal esophageal mucosa changes its color uniformly to dark brown with iodine chromoendoscopy. (b) Iodine-unstained streak “slight”. There are thin longitudinal iodine-unstained streaks appearing slightly. (c) Iodine-unstained streak “clear”. There are thick radial iodine-unstained streaks appearing clearly. |
On the other hand, we often experience cases which have the esophageal mucosa with radial, longitudinal iodine-unstained streak in iodine chromoendoscopy. There are differences in the density of iodine-unstained streak depending on the case (Fig. 1b, c). We evaluated the case which has iodine-unstained streak equal to Figure 1b or more as positive in this study. We sprayed 20 mL of iodine solution (1 g iodine + 2 g potassium iodide + 5 mL mint oil/100mL) onto the esophageal mucosa with endoscope.
Patients and methods
There were 164 cases who had the GERD-like symptom (Frequency Scale for the Symptoms of GERD (FSSG) ≥ 8) [7] and was performed iodine chromoendoscopy onto the esophageal mucosa between September 2008 and February 2015 in Kanazawa Medical University Hospital. Ten cases which were diagnosed as esophageal cancer by the endoscopy were not chosen for this study; and 154 cases were included in this study.
We examined only for symptomatic GERD; symptomatic reflux esophagitis and NERD, so asymptomatic reflux esophagitis was not included in this study.
Examination 1
For the 154 cases, we analyzed the existence of reflux esophagitis finding (≥ Los Angeles classification: grade M) and iodine-unstained streak retrospectively.
Examination 2
There were 47 cases where administration of proton pump inhibitor (PPI) or histamine H2-receptor antagonist (H2-RA) was started and continued for more than 14 days. The exclusion cases were as follows: 1) Those who already taken medical treatment for GERD (56 cases); 2) Those who did not agree to medical treatment (49 cases); 3) Those who stopped medical treatment under 14 days by oneself (one case); and 4) Those the GERD symptom of the 14th day was unidentified because of no visiting our hospital (one case).
The patients were prescribed PPI in 45 cases (omeprazole 20 mg/day: n = 11, lansoprazole 30 mg/day: n = 11, rabeprazole 10 mg/day: n = 17, esomeprazole 20 mg/day: n = 6), and H2-RA in two cases (nizatidine 300 mg/day: n = 1, famotidine: n = 1). We confirmed the improvement of their symptom at the 14th day after the medical treatment was started. Furthermore, we examined predictive factors of the symptom improvement such as sex, age, weight, reflux esophagitis finding, and iodine-unstained streak retrospectively.
Statistical analysis was performed using JMP 9 (SAS Institute Japan Ltd.). Comparison of the prevalence between the two groups was made by univariate analysis using t-test or Chi-square test, and multivariate analysis using logistic regression. Statistical significance was taken as P value < 0.05.
We got the approval (approval number: I429) of the Ethical Review Board in this hospital and carried out this study according to guidelines on Helsinki Declaration.
| Results | ▴Top |
Examination 1
The study was conducted with 154 patients (95 men; 59 women; mean age ± standard deviation (SD): 65.4 ± 10.1 years) (Table 1). An iodine-unstained streak was observed in 50/154 cases (32.5%). For 50 cases with iodine-unstained streak, there were only 24/50 cases (48.0%) who had both reflux esophagitis finding and an iodine-unstained streak (Table 1).
 Click to view | Table 1. The Backgrounds and the Endoscopic Findings of the Patients (Examination 1) |
Examination 2
For 47 cases (PPI: 45 cases, H2-RA: two cases) in which medication was started, the symptom was improved in 34 cases, and did not improve in 13 cases. An iodine-unstained streak was observed more often in “Improved” group rather than in “Not improved” group. Significant difference in reflux esophagitis finding was not found in either groups (Table 2).When we supposed the esophagitis findings to be the predictive factor of the medication effect for GERD, accuracy was 59.6%, sensitivity was 55.9%, specificity was 69.2%, positive predictive value (PPV) was 82.6%, and negative predictive value(NPV) was 37.5%.When we supposed the iodine-unstained streak to be the predictive factor of the medication effect for GERD, accuracy was 68.1%, sensitivity was 61.8%, specificity was 84.6%, PPV was 91.3%, and NPV was 45.8%.
 Click to view | Table 2. Relationship Between the Progress of the GERD Symptom With Gastric Secretion Inhibitor and Each Factor (Examination 2) |
| Discussion | ▴Top |
The study was conducted only with GERD patients and we performed iodine chromoendoscopy regardless of the existence of reflux esophagitis finding. Iodine-unstained streak and reflux esophagitis findings were at the same level for the ability of GERD diagnosis and were not highly precise as seen in the existing reports [3, 6]. We had supposed most patients with reflux esophagitis finding had an iodine-unstained streak, but the number of patients who had a reflux esophagitis finding and iodine-unstained streak was actually less than the half of the group with reflux esophagitis finding in this study. There were many GERD cases which had either a reflux esophagitis finding or iodine-unstained streak positive, so it was considered that they might contribute to the advancement of the GERD diagnosis rate in EGD due to the combination of these factors.
In this study, only 25.0% (26/104) of GERD cases without reflux esophagitis finding had an iodine-unstained streak although 48.7% (19/39) of them had it in the report of Yoshikawa et al [6]. They used the iodine solution that was three times higher concentration than what we used [6], and it might have affected the result. Endoscopists usually use 1-2% iodine solution when they perform iodine chromoendoscopy for esophageal cancer [8, 9], but apposite iodine solution or composition for GERD may be different from that of esophageal cancer. It was considered that adjustments of iodine solution and composition may have advanced iodine chromoendoscopy further in GERD.
In addition, the cases with iodine-unstained streak tend to improve GERD symptoms with medicine. We often have to treat GERD cases which have resistance PPI [10] or functional heartburn [11]. The evaluation of iodine-unstained streak onto the esophageal mucosa was suggested in not only the diagnosis but also for the treatment of GERD.
Since there were some histologic features in biopsy specimens from iodine-unstained streak, Yoshikawa et al examined that the iodine-unstained streak in GERD was the endoscopic finding that indicates gastric juice reflux without mucosal break. These histologic features appear in GERD, such as, basal zone thickness, and papillary length of the epithelium [6]. There were many patients with iodine-unstained streak in the group in which gastric secretion inhibitor was effective. This result suggests the association of gastric acid with iodine-unstained streak; and it is considered that the main factor causing an iodine-unstained streak onto esophageal mucosa of GERD is gastric juice reflux. However, the gastric juice reflux was found not only in iodine-unstained streak but also mucosal break in GERD [12]. Since there were relatively few cases that had both an iodine-unstained streak and reflux esophagitis finding, it may be that the gastric juice reflux is not the only outbreak condition of each finding.
Various elements are involved in outbreak of GERD, such as, esophageal hiatal hernia [13], peristaltic dysfunction [14], and hypersensitivity [15]. In addition, the ratio of these elements is different from erosive reflux esophagitis in NERD [16, 17]. Although it was considered that some kind of elements influenced the presence of iodine-unstained streak and reflux esophagitis finding, it was difficult to perform enough examination about the hypothesis in this study.
There are some advantages of iodine chromoendoscopy in GERD, as follows: 1) It has better GERD diagnosis ability than ordinary white light imaging as showed in this study; 2) It is applicable and usable in various endoscope systems; 3) It may have better visibility than conventional NBI.
For advantage 2), there are some reports which indicate that the magnifying NBI has a good GERD diagnosis ability [18, 19]. There are a lot of hospitals and clinics performing EGD with the conventional endoscope system and the nasal, non-magnifying scope. We think that the technique for supporting GERD diagnosis can be done with every endoscope system because it is a disease treated in various hospitals and clinics. Iodine chromoendoscopy is low-cost and used by endoscopists, so various hospitals and clinics can introduce it for GERD diagnosis relatively easily. For advantage 3), conventional NBI is unfit for the observation in the middle-range distance because light quantity is poor [20]. We often experience cases which have radial, longitudinal darkness onto esophageal mucosa with non-magnifying NBI. However, we feel that the iodine chromoendoscopy is superior to conventional NBI in visibility. Addition, conventional NBI often trouble us for the judgment which radial, longitudinal darkness is either GERD finding or shadow caused by poor in light quantity (Fig. 2). On the other hand, new NBI or BLI-bright have high enough light quantity and image quality, therefore, we can perform good observation for non-magnifying observation and the middle-range distance [20]. These may have equal or greater ability than iodine chromoendoscopy to diagnose GERD.
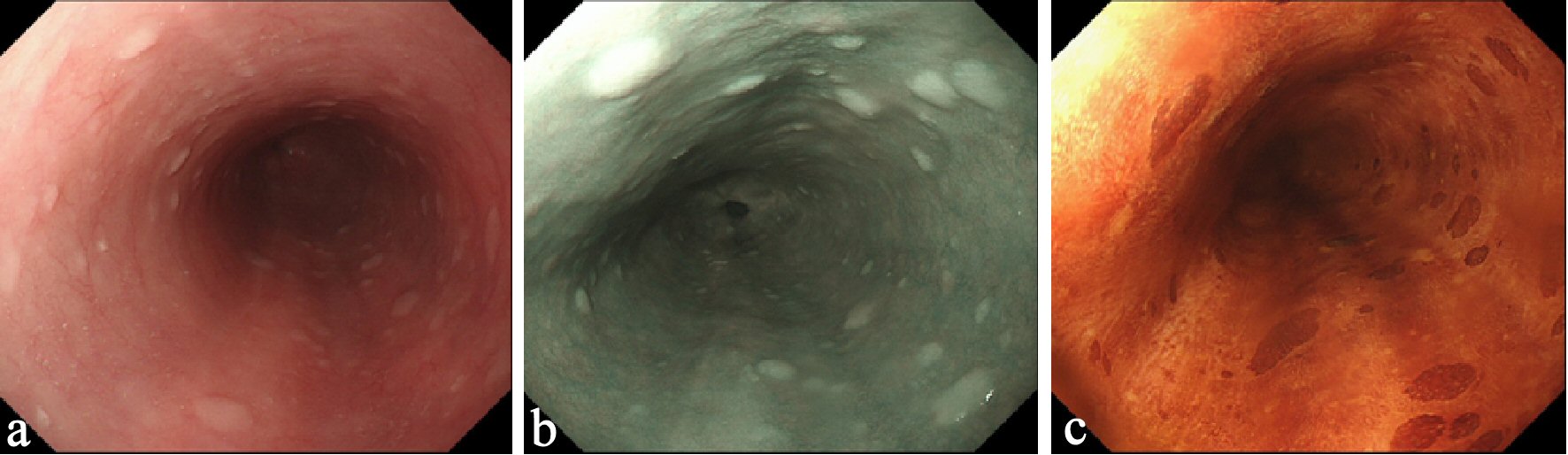 Click for large image | Figure 2. Endoscopic findings on lower esophagus of a GERD case. (a) Ordinary white light. There is neither redness nor erosion. It looks like the normal esophagus mucosa. (b) NBI. Few dark longitudinal areas were found. It is less visible than iodine. (c) Iodine chromoendoscopy. Clear iodine-unstained streaks were found. It is more visible than NBI. NBI: narrow band imaging; GERD: gastroesophageal reflux disease. |
There are some disadvantages of iodine chromoendoscopy in GERD, as follows: 1) It is more complicated than NBI and BLI; 2) Patients often have chest pain after the procedure [21]; 3) It must not be performed in patients with iodine allergy or thyroid dysfunction [21].
There is the case report of the acute esophageal erosions and gastric ulcerations that was caused by iodine chromoendoscopy with 5% of iodine solution [22], but it does not usually have side effects in particular unless the use was prohibited to the patients [21, 22].
There are some limitations to this study. Firstly, some cases prescribed H2-RA were included in “Examination 2”. Secondly, there were multiple kinds of PPI. H2-RA is inferior to PPI in the effect for GERD [23, 24]; but in all cases where H2-RA was prescribed it was effective in iodine-unstained streak and GERD symptom in this study. From these factors, we presume that some cases where H2-RA was prescribed did not influence on this result because the cases, in which 2H-RA was prescribed for GERD symptoms, were more likely to be improved even if PPI was prescribed. There are many reports which found the difference of PPI does not have the influence on the effect for GERD symptom [25, 26]. In other reports, the duration which had the influence was only in the interval of 2 - 5 days [27] or 1 week [28] after the PPI administration was started. It was considered that there were few influences on this examination results about the several kinds of PPI because we evaluated it on the 14th day from the start of the medical treatment.
Conclusions
An iodine-unstained streak and reflux esophagitis finding were at the same level for ability of GERD diagnosis and they did not often overlap on GERD cases in this study. It was considered that they might contribute to the advancement of the GERD diagnosis rate in EGD due to the combination of these factors. In addition, we consider that Lugol-unstained streaks can become a predictive factor of the effective medication for GERD symptoms.
Acknowledgments
We thank all the study investigators and staff and participants who participated in this study, for helpful discussions during manuscript development.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Patients were not required to give informed consent to the study because the retrospective analysis used anonymous clinical data that were obtained after each patient agreed to the treatment schedule by written consent.
Author Contributions
Kazu Hamada wrote the manuscript; Masashi Okuro and Ken Kawaura collected data for review; all authors read and approved the final version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus G. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900-1920; quiz 1943.
doi pubmed - Kusano M, Kouzu T, Kawano T, Ohara S. Nationwide epidemiological study on gastroesophageal reflux disease and sleep disorders in the Japanese population. J Gastroenterol. 2008;43(11):833-841.
doi pubmed - Okamoto K, Iwakiri R, Mori M, Hara M, Oda K, Danjo A, Ootani A, et al. Clinical symptoms in endoscopic reflux esophagitis: evaluation in 8031 adult subjects. Dig Dis Sci. 2003;48(12):2237-2241.
doi pubmed - Yoshikawa I. Efficacy of lugol chromoendoscopy in diagnosing gastro-esophageal reflux disease. Digestive medicine 2004;38(2):177-181.
- Hoffman A, Basting N, Goetz M, Tresch A, Mudter J, Biesterfeld S, Galle PR, et al. High-definition endoscopy with i-Scan and Lugol's solution for more precise detection of mucosal breaks in patients with reflux symptoms. Endoscopy. 2009;41(2):107-112.
doi pubmed - Yoshikawa I, Yamasaki M, Yamasaki T, Kume K, Otsuki M. Lugol chromoendoscopy as a diagnostic tool in so-called endoscopy-negative GERD. Gastrointest Endosc. 2005;62(5):698-703; quiz 752, 754.
doi pubmed - Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, et al. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39(9):888-891.
doi pubmed - Gotoda T, Kanzaki H, Okamoto Y, Obayashi Y, Baba Y, Hamada K, Sakae H, et al. Tolerability and efficacy of the concentration of iodine solution during esophageal chromoendoscopy: a double-blind randomized controlled trial. Gastrointest Endosc. 2020;91(4):763-770.
doi pubmed - Ide E, Carneiro FO, Frazao MS, Chaves DM, Sallum RA, de Moura EG, Sakai P, et al. Endoscopic detection of early esophageal squamous cell carcinoma in patients with achalasia: narrow-band imaging versus Lugol's staining. J Oncol. 2013;2013:736756.
doi pubmed - Miyamoto M, Haruma K, Takeuchi K, Kuwabara M. Frequency scale for symptoms of gastroesophageal reflux disease predicts the need for addition of prokinetics to proton pump inhibitor therapy. J Gastroenterol Hepatol. 2008;23(5):746-751.
doi pubmed - Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Esophageal Disorders. Gastroenterology. 2016;150(6):1368-1379.
doi pubmed - Hayashi Y, Iwakiri K, Kotoyori M, Sakamoto C. Mechanisms of acid gastroesophageal reflux in the Japanese population. Dig Dis Sci. 2008;53(1):1-6.
doi pubmed - Emerenziani S, Habib FI, Ribolsi M, Caviglia R, Guarino MP, Petitti T, Cicala M. Effect of hiatal hernia on proximal oesophageal acid clearance in gastro-oesophageal reflux disease patients. Aliment Pharmacol Ther. 2006;23(6):751-757.
doi pubmed - Kahrilas PJ, Dodds WJ, Hogan WJ, Kern M, Arndorfer RC, Reece A. Esophageal peristaltic dysfunction in peptic esophagitis. Gastroenterology. 1986;91(4):897-904.
doi - Miwa H, Minoo T, Hojo M, Yaginuma R, Nagahara A, Kawabe M, Ohkawa A, et al. Oesophageal hypersensitivity in Japanese patients with non-erosive gastro-oesophageal reflux diseases. Aliment Pharmacol Ther. 2004;20(Suppl 1):112-117.
doi pubmed - Iwakiri K, Hayashi Y, Kotoyori M, Tanaka Y, Kawami N, Sano H, Takubo K, et al. Defective triggering of secondary peristalsis in patients with non-erosive reflux disease. J Gastroenterol Hepatol. 2007;22(12):2208-2211.
doi pubmed - Conchillo JM, Schwartz MP, Selimah M, Samsom M, Sifrim D, Smout AJ. Acid and non-acid reflux patterns in patients with erosive esophagitis and non-erosive reflux disease (NERD): a study using intraluminal impedance monitoring. Dig Dis Sci. 2008;53(6):1506-1512.
doi pubmed - Sharma P, Wani S, Bansal A, Hall S, Puli S, Mathur S, Rastogi A. A feasibility trial of narrow band imaging endoscopy in patients with gastroesophageal reflux disease. Gastroenterology. 2007;133(2):454-464; quiz 674.
doi pubmed - Fock KM, Teo EK, Ang TL, Tan JY, Law NM. The utility of narrow band imaging in improving the endoscopic diagnosis of gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2009;7(1):54-59.
doi pubmed - Yamada A, Kaise M. Characteristics of a New Generation of Endoscopy Systems. Endoscopia Digestiva. 2014;26(5):655-660.
- Toriie S, Kimoto K, Kato S, Takeda S, Kohli Y, Hashimoto Y, Nakajima M, et al. New trial for endoscopic observation of the esophageal mucosa and its application. Gastroenterological Endoscopy. 1974;16(4):386-393.
- Kato F, Matsuura A, Yoshii Y, Kasugai T, Tanaka Y, Kato K. Acute esophageal erosions and gastric ulcerations induced by Lugol's solution spray at dye scattering esophagoscopy, report of two cases. Gastroenterological Endoscopy. 1984;26(12):2408-2415.
- Haag S, Holtmann G. Onset of relief of symptoms of gastroesophageal reflux disease: post hoc analysis of two previously published studies comparing pantoprazole 20 mg once daily with nizatidine or ranitidine 150 mg twice daily. Clin Ther. 2010;32(4):678-690.
doi pubmed - Khan M, Santana J, Donnellan C, Preston C, Moayyedi P. Medical treatments in the short term management of reflux oesophagitis. Cochrane Database Syst Rev. 2007;2:CD003244.
- Pace F, Annese V, Prada A, Zambelli A, Casalini S, Nardini P, Bianchi Porro G, et al. Rabeprazole is equivalent to omeprazole in the treatment of erosive gastro-oesophageal reflux disease. A randomised, double-blind, comparative study of rabeprazole and omeprazole 20 mg in acute treatment of reflux oesophagitis, followed by a maintenance open-label, low-dose therapy with rabeprazole. Dig Liver Dis. 2005;37(10):741-750.
doi pubmed - Eggleston A, Katelaris PH, Nandurkar S, Thorpe P, Holtmann G, Treat Study G. Clinical trial: the treatment of gastro-oesophageal reflux disease in primary care—prospective randomized comparison of rabeprazole 20 mg with esomeprazole 20 and 40 mg. Aliment Pharmacol Ther. 2009;29(9):967-978.
doi pubmed - Zheng RN. Comparative study of omeprazole, lansoprazole, pantoprazole and esomeprazole for symptom relief in patients with reflux esophagitis. World J Gastroenterol. 2009;15(8):990-995.
doi pubmed - Pace F, Coudsy B, DeLemos B, Sun Y, Xiang J, LoCoco J, Casalini S, et al. Does BMI affect the clinical efficacy of proton pump inhibitor therapy in GERD? The case for rabeprazole. Eur J Gastroenterol Hepatol. 2011;23(10):845-851.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


