| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 12, Number 2, February 2020, pages 108-114
The Anatomical Characteristics of Corona Mortis: A Systematic Review of the Literature and Its Clinical Importance in Hernia Repair
George Noussiosa, Nikiforos Galanisb, Iosif Chatzisc, Sergios Konstantinidisc, Eva Filoc, George Karavasilisd, Anastasios Katsourakisc, e
aSchool of Physical Education and Sports Sciences of Serres, Aristotle University of Thessaloniki, Thessaloniki, Greece
bSchool of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
cDepartment of General Surgery, Agios Dimitrios General Hospital, Thessaloniki, Greece
dDepartment of Business Administration, Technological Educational Institute of Central Macedonia, Serres, Greece
eCorresponding Author: Anastasios Katsourakis, Department of General Surgery, Agios Dimitrios General Hospital, Elenis Zografou 2, 54634 Thessaloniki, Greece
Manuscript submitted December 9, 2019, accepted January 6, 2020
Short title: Corona Mortis and Its Clinical Importance
doi: https://doi.org/10.14740/jocmr4062
| Abstract | ▴Top |
Background: Inguinal hernia repair is one of the most common daily operations in general surgery. However, the anatomical structures of the region, such as the corona mortis (the crown of death), make this procedure quite challenging. A comprehensive knowledge of its anatomy is essential, since massive hemorrhage may occur if the vessel is injured. The current review of the literature aimed to report the frequency and anatomical variations of vascular corona mortis.
Methods: A substantial study was coordinated through PubMed, Scopus and Google Scholar. The Prisma guidelines were used for the systematic review of the articles found. A total of 13 studies and 1,455 patients were included for the statistical analysis.
Results: The results showed that corona mortis was present in about half the hemi-pelvises, and to be more accurate, the prevalence was 46%. Venous corona mortis was more frequent than the arterial type (42% vs. 25%).
Conclusions: Considering the percentages mentioned above, every surgeon who schedules an operation on the retro-pubic area, especially during a hernioplasty procedure, should evaluate the possibility of the presence of corona mortis. Anatomical knowledge of the region is vital for attempting to eliminate the risk of injuring the corona mortis during surgery.
Keywords: Corona mortis; Inguinal hernia; Hemorrhage; Anatomical variations
| Introduction | ▴Top |
The corona mortis (CMOR), also known as the “crown of death”, is a horrifying name that serves to represent the high risk of hemorrhage that may occur if this anatomical variant is injured and the difficulty of achieving hemostasis. CMOR is the vascular anastomosis between the obturator and external iliac or inferior epigastric vessels (Fig. 1); this connection is usually regarded as arterial, but it may be venous or both venous and arterial [1-7]. It has been found that, sometimes, an enlarged pubic branch of the inferior epigastric artery that descends into the obturator foramen may replace the obturator artery, and an enlarged pubic vein that joins the iliac vein may replace the obturator vein [8, 9]. Most of the studies included in the current meta-analysis identify the presence of an arterial CMOR; in those in which venous CMOR is recognized, the incidence of venous anatomical variation is higher. These divergent vessels cross the superior pubic ramus, making them prone to injury during a laparoscopic hernia repair or the placement of a mesh during open surgery.
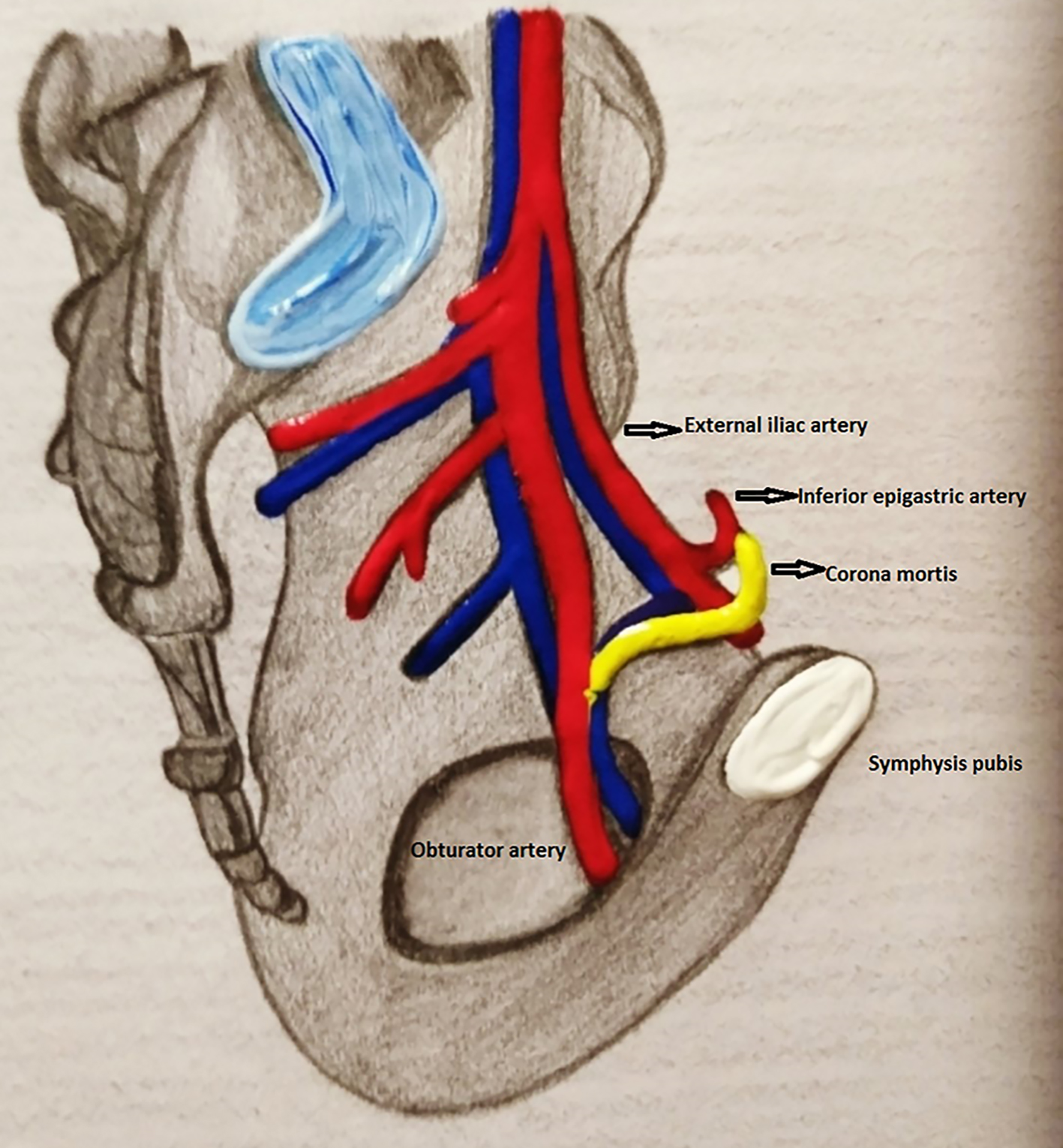 Click for large image | Figure 1. Drawing demonstrating corona mortis which connects the obturator with the inferior epigastric vessels (created by Eva Filo). |
| Materials and Methods | ▴Top |
Search method
A comprehensive search was administered through the PubMed, Scopus and Google Scholar search engines to identify the number of articles that met the inclusion criteria for analysis. The search terms that were used were as follows: CMOR, crown of death, hernia, complications, hemorrhage and anatomical variations. No review protocol existed. The references of all the included articles were searched to identify if any further relevant articles existed. For the analysis, we included only original articles written in English during the last 15 years. Case reports, conference abstracts, letters to the editor and studies reporting incomplete or irrelevant data were excluded from the study. Any differences of opinion among the authors were solved through consultation. The authors followed the Prisma guidelines for the analysis, which was conducted by two separate reviewers independently, and the reviewers were also responsible for the extraction of the data. The data included the origin of the patients, gender and CMOR prevalence (arterial, venous or both) and location (right, left or bilateral). Further statistical consultation was conducted if there was any disparity regarding the data.
Statistical analysis
The pooled data were examined for heterogeneity using the random effects model, more specifically, MetaXL 5.3, the freely available software for meta-analysis in Microsoft Excel. The pooled prevalence and Cochran’s Q test were estimated to identify heterogeneity among studies. If the confidence intervals (CIs) of the pooled prevalence estimate (PPE) overlapped poorly, this was strong evidence of statistical heterogeneity. The I2 statistics (Higgins statistics) were also calculated, describing the percentage of the variability in effect estimates that was due to heterogeneity rather than sampling error.
| Results | ▴Top |
After an extensive search of the databases, a total of 465 records were identified. Of those, 451 articles did not meet the inclusion criteria or were duplicates, and 14 full-text articles were assessed for eligibility. Finally, 13 articles were included in the qualitative and quantitative synthesis, and one study was excluded due to statistical issues (Fig. 2). Most of the included studies, a total of nine, were performed on cadavers; of the others, two reported radiological results and two dealt with intraoperative findings (Table 1) [3, 6-8, 10-18].
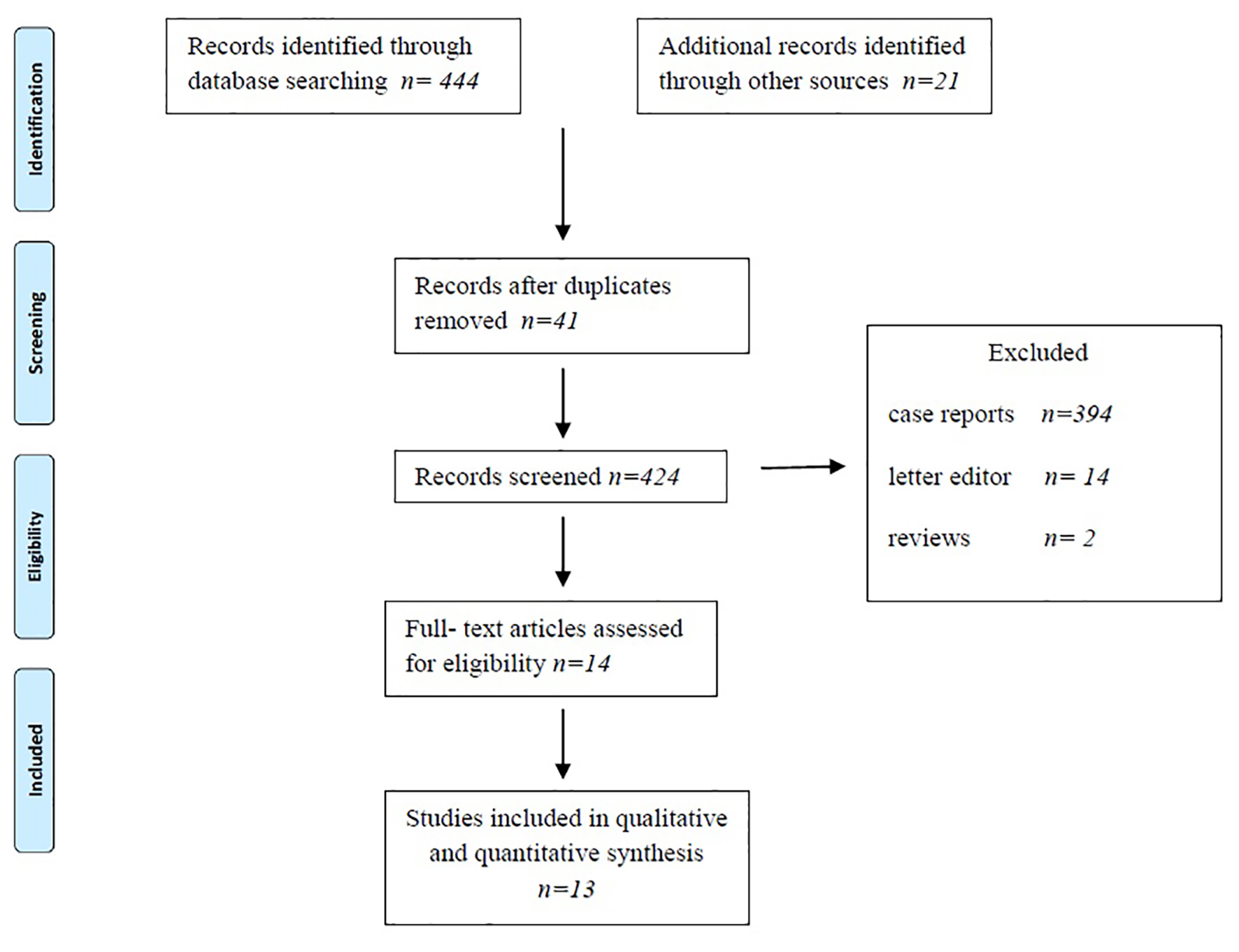 Click for large image | Figure 2. Flow diagram of included studies according to Prisma guidelines. |
 Click to view | Table 1. The Included Studies, Their Country of Origin, Type of Study and Prevalence of CMOR |
A total of 1,455 hemi-pelvises were assessed for the statistical analysis; the PPE for the full sample was 0.46 (95% CI: 0.34 - 0.58), as shown in Table 2. In terms of the geographical distribution, the PPE of the sample from the America’s was 45.66 (95% CI: 26.04 - 65.96), which was close to the total result, while a higher result was found in Europe, at 53.79 (95% CI: 22.55 - 83.67), and a lower one in Asia, at 41.52 (95% CI: 23.95 - 60.20).
 Click to view | Table 2. The Total PPE and the Statistical Heterogeneity (Higgins I2 Statistics) of CMOR as Well as the PPE and I2 According to the Continent, the Type of Study and the Location of CMOR |
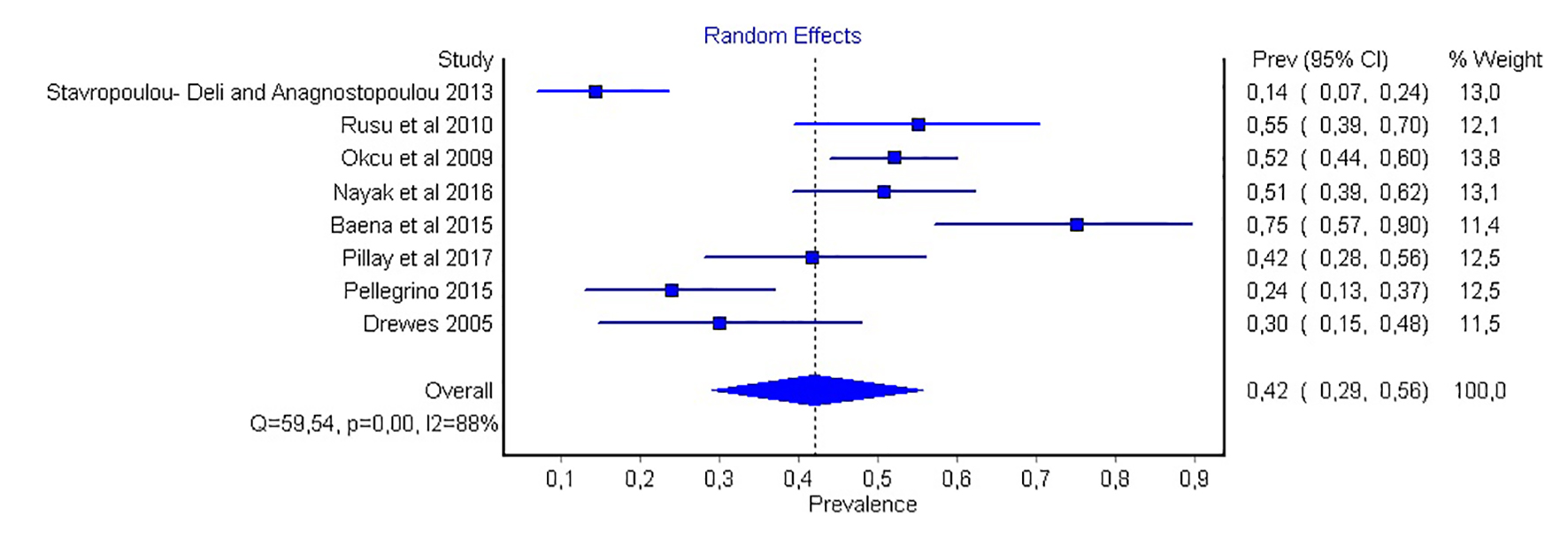
There was no difference in the PPE regarding the presence of CMOR on the sides of the hemi-pelvises (right vs. left), while the PPE for bilateral presence was half of the previous values, at 0.08 (95% CI: 0.09 - 0.22; Table 2). In all the above cases, according to the Higgins I2 statistics, the heterogeneity was quite high, except in the results from the imaging, where the relatively small sample size suggested that more studies should be conducted to generate more reliable conclusions (Figs. 3-5).
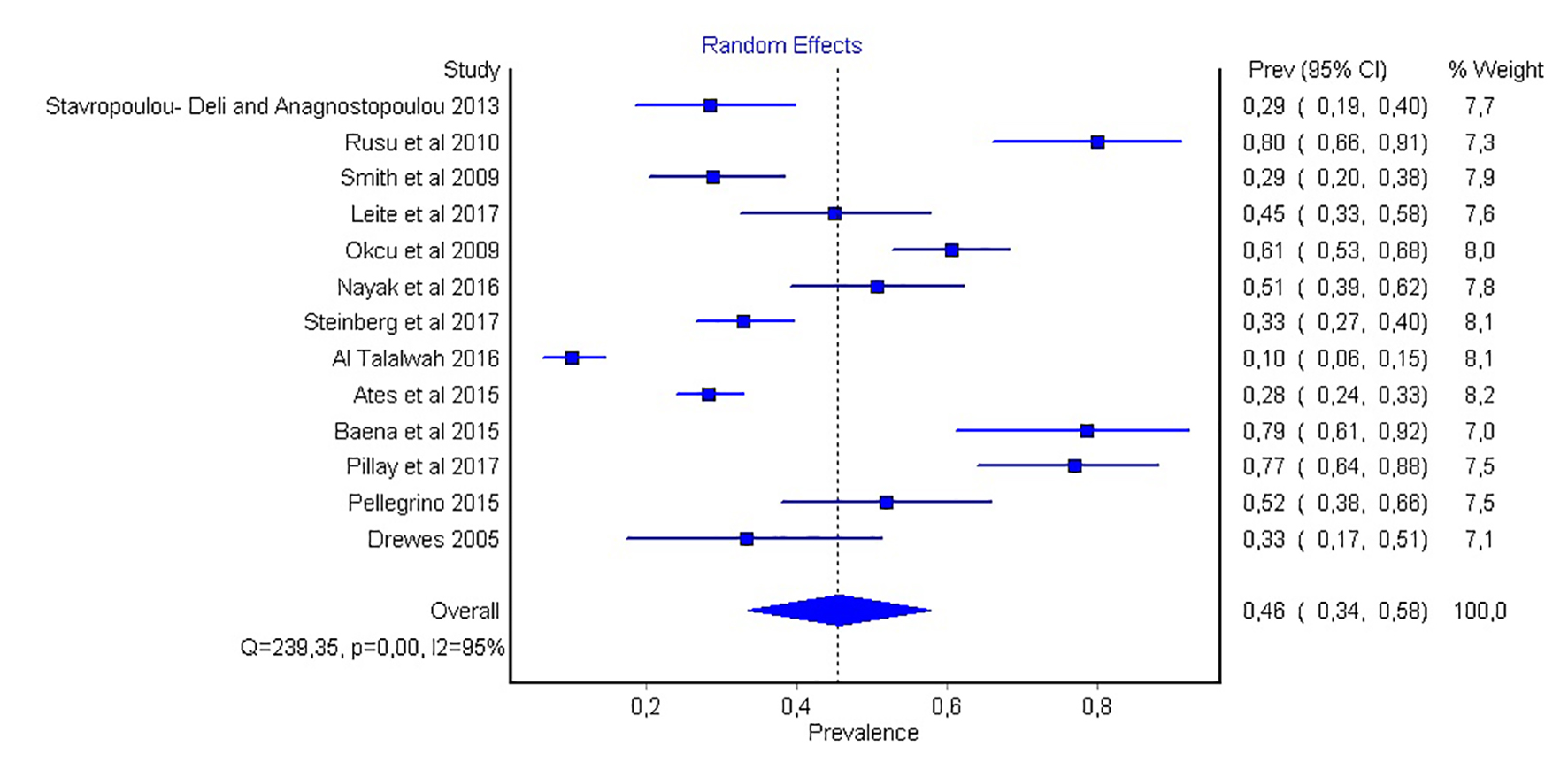 Click for large image | Figure 3. Forest plot of the total prevalence of corona mortis. |
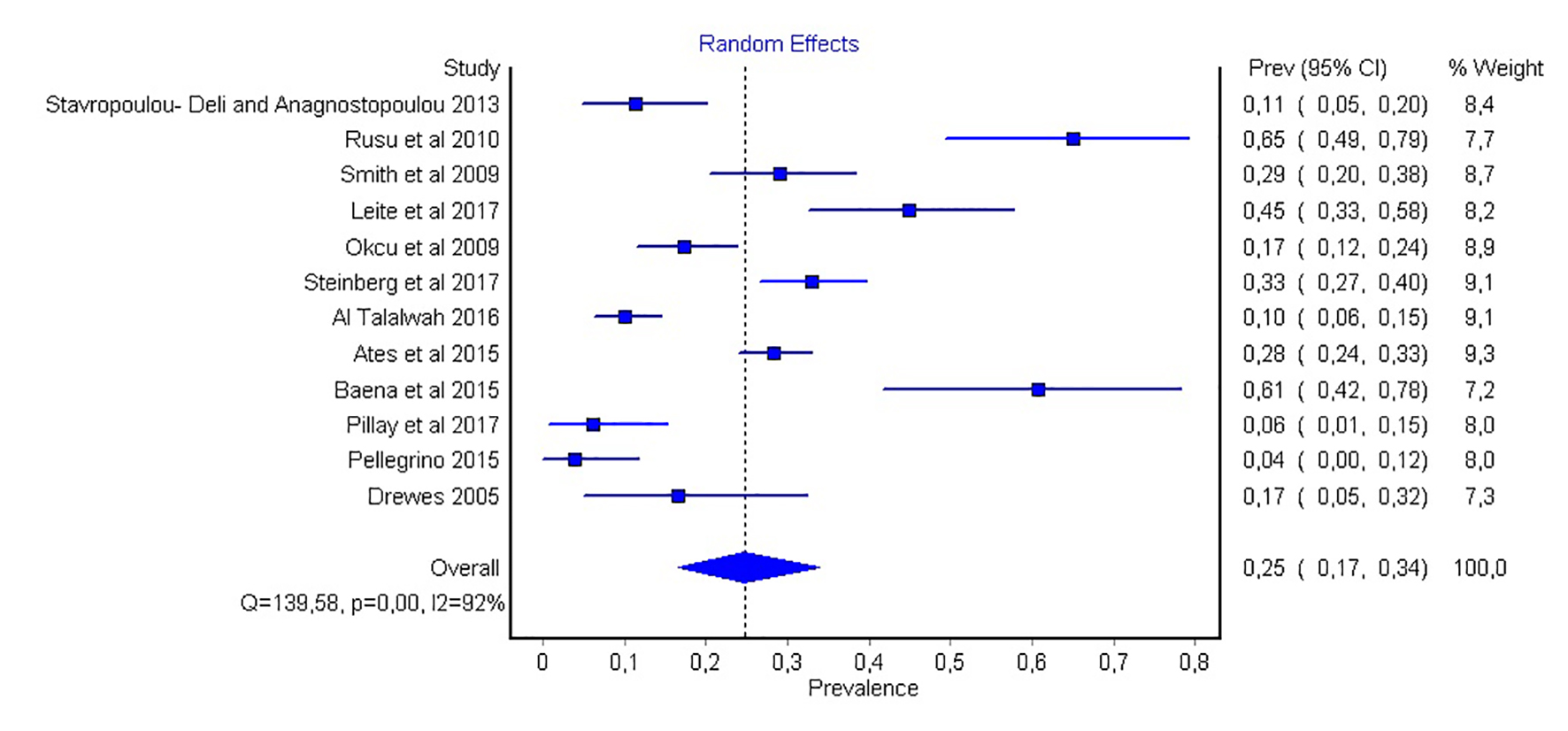 Click for large image | Figure 4. Forest plot of the prevalence of an arterial only corona mortis. |
 Click for large image | Figure 5. Forest plot of the prevalence of a venous only corona mortis. |
| Discussion | ▴Top |
The presence of CMOR can complicate fractures in the pubic ramus, as well as several surgical procedures. The open or laparoscopic technique is used, and inguinal hernia repair - one of the most common operations in general surgery daily practice - belongs to these operations. The high prevalence of CMOR in the population makes it clinically important. The exact definition of CMOR remains controversial until today. First, in their study, Damanis et al stated that there are three anatomical structures that cross the pubic ramus on its posterior area, namely, an artery or a vein and an aberrant obturator artery [19]. Today, most anatomical textbooks support that CMOR is an anastomotic vessel between the obturator and external iliac or inferior epigastric vessels. There are also some authors suggesting that CMOR is a clinical rather than anatomical structure [10]. Rusu and co-authors have categorized the venous CMOR into three types based on the drainage arrangement of the obturator vein [7]. It is type I when it drains to the external iliac vein, type II when draining into the inferior epigastric vein and type III when the obturator vein and inferior epigastric vein anastomose.
The goal of our review was determining the true prevalence of CMOR among the population, as well as its variations and anatomical characteristics, to diminish the possibility of iatrogenic perforation or cross-section of the vessel during hernia repair. When CMOR is present, it can be damaged during the laparoscopic procedure from the tacks used during the fixation of the mesh into the Cooper’s ligament. This can cause severe bleeding, which is difficult to control and often results in conversion to open surgery or retroperitoneal hematoma and reoperation. In addition, surgeons should be aware that injury of the artery can cause greater hemodynamic instability and hemorrhage, but venous CMOR is more difficult to diagnose and control. Beyond the anatomic variations of CMOR, another issue is the distance of the vessel from the pubis symphysis. Karakurt et al first reported that the distance can be 21.4 - 41 mm; however, most authors have concluded that the distance almost always exceeds 30 mm [20-23]. In addition, the diameter of the vessel is most often more than 3 mm and cannot be easily ignored, because in conventional surgery, vessels of a diameter less than 2 mm can be missed [11, 24].
In our study, the overall prevalence of CMOR in the population was relatively high, and more specifically, it was found in half of all the hemi-pelvises, with a predominance of 46%. Venous CMOR was more frequent than arterial CMOR was (42% vs. 25%). The heterogeneity of the studies included was not enough to extract safe results regarding the location of the vessel (left vs. right hemi-pelvis), as well as the presence of both the artery and vein. CMOR was more prevalent in patients from Europe than those from Asia (48.75% vs. 34.09%); concerning the patients from America, the PPE was very close to the overall one (Table 2).
Regarding the type of studies included into the study, the deviation of the PPE from the overall value was high for the cadaveric and low for the intraoperative and imaging (Table 2).
The main limitation of our analysis was the heterogeneity among the studies, which probably arose due to the anatomical differences among the continents regarding the development of the vascular system. In addition, most of the studies were performed on cadavers, possibly because the researchers had the advantage of three-dimensional vision and direct examination by hand without the risk of hemorrhage. To properly compare cadaveric with intraoperative or imaging studies, more of the latter are necessary. However, the large sample sizes included in our analysis and the statistical methods employed represent the strengths of this research. From a statistical point of view, it is necessary to organize and conduct large multicenter studies based mainly on living subjects, confined to one continent to reduce heterogeneity and bias.
In conclusion, our main results revealed that CMOR was present in nearly half the population, and it is more common in patients from Europe than from Asia, with the venous being more frequent than the arterial type. Considering its prevalence and anatomical variations, the CMOR, or crown of death, should be recognized during the hernia repair and treated with the respect the name indicates.
Acknowledgments
We would like to express our sincere appreciation to George Karavasilis, Department of Business Administration, Technological Educational Institute of Central Macedonia, Greece, for his contribution to the statistical analysis.
Financial Disclosure
There was no funding for this study.
Conflict of Interest
All authors declare that they have no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Anastasios Katsourakis and Sergios Konstantinidis. The first draft of the manuscript was written by George Noussios and Anastasios Katsourakis, and all the authors commented on previous versions. All the authors approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Berberoglu M, Uz A, Ozmen MM, Bozkurt MC, Erkuran C, Taner S, Tekin A, et al. Corona mortis: an anatomic study in seven cadavers and an endoscopic study in 28 patients. Surg Endosc. 2001;15(1):72-75.
doi pubmed - Namking M, Woraputtaporn W, Buranarugsa M, Kerdkoonchorn M. Corona mortis in Thai. FASEB Journal. 2006;20:A445.
- Okcu G, Erkan S, Yercan HS, Ozic U. The incidence and location of corona mortis: a study on 75 cadavers. Acta Orthop Scand. 2004;75(1):53-55.
doi pubmed - Lau H, Lee F. A prospective endoscopic study of retropubic vascular anatomy in 121 patients undergoing endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2003;17(9):1376-1379.
doi pubmed - Kashyap S, Diwan Y, Mahajan S, Diwan D, Lal M, Chauhan R. The Majority of Corona mortis are small calibre venous blood vessels: a cadaveric study of North Indians. Hip Pelvis. 2019;31(1):40-47.
doi pubmed - Pellegrino A, Damiani GR, Marco S, Ciro S, Cofelice V, Rosati F. Corona mortis exposition during laparoscopic procedure for gynecological malignancies. Updates Surg. 2014;66(1):65-68.
doi pubmed - Rusu MC, Cergan R, Motoc AG, Folescu R, Pop E. Anatomical considerations on the corona mortis. Surg Radiol Anat. 2010;32(1):17-24.
doi pubmed - Drewes PG, Marinis SI, Schaffer JI, Boreham MK, Corton MM. Vascular anatomy over the superior pubic rami in female cadavers. Am J Obstet Gynecol. 2005;193(6):2165-2168.
doi pubmed - Gilroy AM, Hermey DC, DiBenedetto LM, Marks SC, Jr., Page DW, Lei QF. Variability of the obturator vessels. Clin Anat. 1997;10(5):328-332.
doi - Ates M, Kinaci E, Kose E, Soyer V, Sarici B, Cuglan S, Korkmaz F, et al. Corona mortis: in vivo anatomical knowledge and the risk of injury in totally extraperitoneal inguinal hernia repair. Hernia. 2016;20(5):659-665.
doi pubmed - Stavropoulou-Deli A, Anagnostopoulou S. Corona mortis: anatomical data and clinical considerations. Aust N Z J Obstet Gynaecol. 2013;53(3):283-286.
doi pubmed - Smith JC, Gregorius JC, Breazeale BH, Watkins GE. The corona mortis, a frequent vascular variant susceptible to blunt pelvic trauma: identification at routine multidetector CT. J Vasc Interv Radiol. 2009;20(4):455-460.
doi pubmed - Leite TFO, Pires LAS, Goke K, Silva JG, Chagas CAA. Corona Mortis: anatomical and surgical description on 60 cadaveric hemipelvises. Rev Col Bras Cir. 2017;44(6):553-559.
doi pubmed - Nayak SB, Deepthinath R, Prasad AM, Shetty SD, Aithal AP. A South Indian cadaveric study on obturator neurovascular bundle with a special emphasis on high prevalence of 'venous corona mortis'. Injury. 2016;47(7):1452-1455.
doi pubmed - Steinberg EL, Ben-Tov T, Aviram G, Steinberg Y, Rath E, Rosen G. Corona mortis anastomosis: a three-dimensional computerized tomographic angiographic study. Emerg Radiol. 2017;24(5):519-523.
doi pubmed - Al Talalwah W. A new concept and classification of corona mortis and its clinical significance. Chin J Traumatol. 2016;19(5):251-254.
doi pubmed - Baena G, Rojas S, Pena E. Corona mortis: anatomical and clinical relevance and recurrence in a sample of the Colombian population. Int J Morphol. 2015;33(1):130-136.
doi - Pillay M, Sukumaran T, Mayilswanny M. Anatomical considerations on surgical implications of corona mortis: an Indian study. IJAE. 2017;122(2):127-136.
- Darmanis S, Lewis A, Mansoor A, Bircher M. Corona mortis: an anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin Anat. 2007;20(4):433-439.
doi pubmed - Tornetta P, 3rd, Hochwald N, Levine R. Corona mortis. Incidence and location. Clin Orthop Relat Res. 1996;329:97-101.
doi - Karakurt L, Karaca I, Yilmaz E, Burma O, Serin E. Corona mortis: incidence and location. Arch Orthop Trauma Surg. 2002;122(3):163-164.
doi pubmed - Walsh CA. TVT-Secur mini-sling for stress urinary incontinence: a review of outcomes at 12 months. BJU Int. 2011;108(5):652-657.
doi pubmed - Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, Kraus SR, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066-2076.
doi pubmed - Hong HX, Pan ZJ, Chen X, Huang ZJ. An anatomical study of corona mortis and its clinical significance. Chin J Traumatol. 2004;7(3):165-169.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


