| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 12, Number 1, January 2020, pages 13-17
Clinical Features of Spontaneous Isolated Dissection of Abdominal Visceral Arteries
Hiroaki Shirakia, Manabu Kasamotob, Masamichi Yasutomia, Shuichiro Kajib, Koichi Akutsuc, Yutaka Furukawab, Wataru Shimizuc, Nobutaka Inouea, d
aDepartment of Cardiovascular Medicine, Kobe Rosai Hospital, Kobe, Japan
bDepartment of Cardiovascular Medicine, Kobe City Medical Center General Hospital, Kobe, Japan
cDepartment of Cardiovascular Medicine, Nippon Medical School, Tokyo, Japan
dCorresponding Author: Nobutaka Inoue, Department of Cardiovascular Medicine, Kobe Rosai Hospital, 4-1-23, Kagoike Touri, Chuo-Ku, Kobe 651-0053, Japan
Manuscript submitted September 10, 2019, accepted October 15, 2019
Short title: Dissection of Abdominal Visceral Arteries
doi: https://doi.org/10.14740/jocmr3916
| Abstract | ▴Top |
Background: Spontaneous isolated dissection of abdominal visceral arteries without aortic dissection is rare and its pathology and prognosis are not yet clear; therefore, therapeutic strategies for this disease have not been established. The present multi-institution investigational study analyzed the clinical features of patients with spontaneous isolated dissection of abdominal visceral arteries.
Methods: A total of 36 patients diagnosed as spontaneous isolated dissection of abdominal visceral arteries from January 2010 to October 2016 were enrolled. The medical data of the patients were retrospectively reviewed. Imaging characteristics were evaluated. Spontaneous isolated dissection of abdominal visceral arteries was detected on upper abdominal computed tomography examination in almost patients, and was detected on magnetic resonance imaging in one patient.
Results: Of the 36 cases, 26 cases involved the superior mesenteric artery dissection, nine involved the celiac artery, two involved the splenic artery, one involved the common hepatic artery, one involved the gastroduodenal artery and one involved the left gastric artery. Among the 36 patients, 20 had hypertension and 14 were current smokers. Additionally, only one patient had diabetes and four patients had dyslipidemia. Moreover, 32 cases complained of pain including abdominal pain and back pain, one had cough and three had no symptoms. Of the 36 patients, 34 cases (94.4%) were treated conservatively, and two (5.6%) required intravascular treatment. All patients were discharged without complications.
Conclusions: Our findings indicate that hypertension and smoking might be closely involved in the pathogenesis of spontaneous isolated dissection of abdominal visceral arteries, whereas dyslipidemia and diabetes might be less involved. Additionally, few asymptomatic patients were accidentally diagnosed, indicating that the absence of symptoms cannot be used to rule out the presence of this disease. Randomized clinical trials cannot be performed because a considerable number of cases are required. Therefore, detailed descriptions of clinical features, as provided in our report, are important.
Keywords: Spontaneous isolated dissection; Abdominal visceral arteries; Hypertension; Smoking
| Introduction | ▴Top |
Spontaneous isolated dissection of visceral arteries affecting celiac or superior mesenteric arteries dissection without aortic dissection is considered a rare clinical entity. However, this disease is now being frequently diagnosed because the number of medical facilities capable of performing computed tomography (CT) has recently increased and the resolution of CT has markedly improved. Nevertheless, the pathogenesis, natural course and prognosis of this disease remain to be elucidated. Furthermore, a therapeutic strategy for this disease has not been established. Recently, various approaches/therapeutic algorithms have been proposed, including antihypertensive therapy, antithrombotic therapy, endovascular treatment, surgery and conservative observation without medication [1-3]. However, the validity of these therapeutic algorithms remains to be established.
A recent series of case reports on spontaneous isolated dissection of abdominal visceral arteries revealed that this disease could manifest various clinical features [1-4]. Considering the possible diversity of these features, it is important to clarify the clinical conditions of patients with spontaneous isolated dissection of abdominal visceral arteries. Thus, the present multi-institution study analyzed the clinical conditions of patients with spontaneous isolated dissection of abdominal visceral arteries.
| Materials and Methods | ▴Top |
A total of 36 patients (mean age 54.6 years; male/female, 29/7) diagnosed with spontaneous isolated dissection of abdominal visceral arteries between January 2010 and October 2016 were enrolled in this multi-institutional study. The participating institutions were Kobe Rosai Hospital, Kobe Medical Center City Hospital and Nippon Medical School. The medical data of the patients were retrospectively reviewed. Data including sex, age, medical history, medications and initial symptoms were collected. Imaging characteristics such as the location of the dissection entry point relative to the vessel origin were evaluated. The therapeutic strategy for each patient was determined according to the discretion of the attending physicians.
All enrolled patients were interviewed and clinically examined. Demographic information (age and sex) and medical history were recorded. Hypertension was defined as systolic pressure ≥ 140 mm Hg or diastolic pressure ≥ 90 mm Hg, or the use of antihypertensive drugs. Dyslipidemia was defined as plasma low-density lipoprotein ≥ 140 mg/dL, plasma triglycerides ≥ 150 mg/dL, or plasma high-density lipoprotein < 40 mg/dL or the use of lipid-lowering drugs. Diabetes mellitus was defined as a glycated hemoglobin (HbA1c) concentration of ≥ 6.5% (as per National Glycohemoglobin Standardization Program) and/or the subjects who received medication for diabetes.
Spontaneous isolated dissection of abdominal visceral arteries was detected on upper abdominal CT examination in almost patients, and was detected on magnetic resonance imaging (MRI) in one patient.
This study was approved by the ethical committee of Kobe Rosai Hospital, Kobe City Medical Center General Hospital and Nippon Medical School according to the Declaration of Helsinki (approval number 27-13).
| Results | ▴Top |
Patients’ characteristics
The risk factors and clinical characteristics of the 36 patients are presented in Table 1. Among the 36 patients, 20 patients (55.6%) had hypertension and 14 patients (38.8%) were current smokers. All patients with hypertension were diagnosed with essential hypertension, and they were treated with anti-hypertensive drugs. Additionally, diabetes and dyslipidemia were noted in one and four patients, respectively (Table 2). Six cases (patient no. 14, 19, 22, 25, 32, 35 and 36) had no atherosclerotic risk factors. More, 32 patients complained of pain including abdominal pain and back pain, one had cough and three had no symptoms (Table 2).
 Click to view | Table 1. Characteristics of Patients |
 Click to view | Table 2. Patients Clinical Data |
Localization and Sakamoto classification of diseased vessels
Of the 36 cases, 26 cases involved the superior mesenteric artery dissection, nine involved the celiac artery, two involved the splenic artery, one involved the common hepatic artery, one involved the gastroduodenal artery and one involved the left gastric artery.
According to a previous report, spontaneous isolated dissection of abdominal visceral arteries can be classified into the following categories (Sakamoto classification): type I represented false lumens with both entry and reentry; type II represented “cul-de-sac”-shaped false lumens without reentry, type III represented thrombosed false lumens with ulcer-like projections defined as localized blood filled pouches protruding from the true lumens into the thrombosed false lumens and type IV represented completely thrombosed false lumens without ulcer-like projections (Fig. 1). In our study, six cases (16%), two cases (5.5%), seven cases (19.4%) and 16 cases (44.4%) were classified as type 1, type 2, type 3 and type 4, respectively, and five cases (13%) were unclassified.
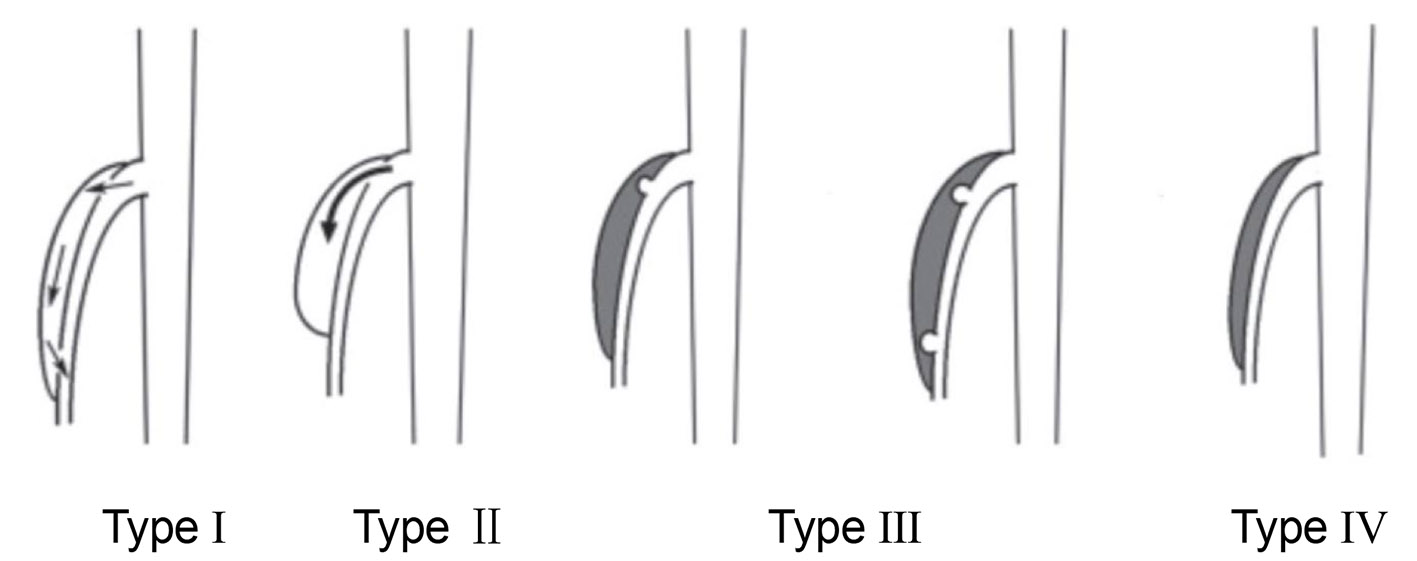 Click for large image | Figure 1. Sakamoto classification. Type I represents false lumens with both entry and reentry. Type II represents “cul-de-sac”-shaped false lumens without reentry. Type III represents thrombosed false lumens with ulcer-like projections defined as localized blood filled pouches protruding from the true lumens into the thrombosed false lumens. Type IV represents completely thrombosed false lumens without ulcer-like projections. |
Treatment and prognosis
Treatments were categorized into the following three types: conservative, endovascular and surgical treatment such as abdominal artery bypass surgery. Conservative treatments included analgesia, blood pressure control, anticoagulation and antiplatelet therapy. Endovascular treatments included stenting and coiling. Of the 36 patients, 34 (94.4%) were treated conservatively, and two cases (5.6%) required intravascular treatment. No patient required surgery. All patients were discharged without complications.
| Discussion | ▴Top |
Previous studies have reported that patient age at the onset of spontaneous isolated dissection of abdominal visceral arteries was relatively low. Male prevalence has been reported to be high, and Nagai et al reported that the male/female ratio was 4:1 [1-5]. The risk factors of this disease remain to be elucidated; however, hypertension and smoking are considered to be closely involved in its pathogenesis, whereas dyslipidemia and diabetes appear to be less involved. In our study, the median patient age was 54.6 years, and male prevalence was 80.1%. Additionally, the prevalence of hypertension was 55.6%, and smoking history was 38.8%. Only one patient had diabetes. Our findings in the present study are consistent with those of previous reports. The pathogenesis of this disease might be different from that of atherosclerotic vascular diseases, because diabetes, dyslipidemia and aging are strong risk factors of atherosclerotic vascular diseases. However, these factors such as hypertension, diabetes, obesity, or male sex are influenced by each other. Therefore, to determine the risk factor of spontaneous isolated dissection of abdominal visceral arteries, it is necessary to conduct a propensity matching analysis of control subjects and patients in a more large number. Wagner et al reported that fibromuscular dysplasia, cystic medial necrosis and the elastic tissue diseases such as Marfan disease and Ehlers-Danlos disease are possible causes of spontaneous isolated dissection of abdominal visceral arteries [6]. However, in our study, no patients presented with symptoms of connective tissue diseases or vasculitis.
Park et al demonstrated mechanical stress at the anterior wall around the convex portion of the superior mesenteric artery using computational fluid dynamic models [7]. Recently, Wu et al clearly showed a positive association between large superior mesenteric artery-distal aorta angles and the occurrence of the dissection of the superior mesenteric artery [8]. These findings strongly suggest that enhanced shear stress on the vessel wall plays a critical role in the initiation of the dissection.
In our study, patients had abdominal pain or back pain (88.9%) and few patients were asymptomatic (8.3%). Asymptomatic patients were accidentally diagnosed when they got CT. These findings indicate that the absence of symptoms cannot be used to rule out the presence of spontaneous isolated dissection of abdominal visceral arteries without aortic dissection. It is difficult to make a diagnosis based on symptoms and special examinations; therefore, imaging approaches are necessary to make a definite diagnosis. The resolutions of CT have recently markedly improved, and the condition of not only the dissection but also the surrounding tissue or intestine can be examined with CT. On the other hand, 1.5 Tesla, but not 3.0 Tesla, MRI is usually used in the abdominal lesion. In the present study, most cases were diagnosed with CT.
The most appropriate therapeutic strategy for spontaneous isolated dissection of abdominal visceral arteries remains to be established. The surgical indications have been proposed to include: 1) Rupture in the acute phase; 2) Imminent rupture; 3) Progression of organ ischemia; 4) Enlargement of the aneurysm (size > 20 mm) in the chronic phase; and 5) Frequent occurrence of chronic organ symptoms such as abdominal angina [9]. Conservative approaches such as analgesia, control of blood pressure and antithrombotic therapy could prevent organ ischemia caused by thromboembolism. However, the use of antithrombotic drugs including anti-platelet drugs or anticoagulants remains to be controversial. In the present study, two of the 36 patients had organ ischemia, and therefore, received intravascular treatment. The other cases were treated conservatively.
Recently, Satokawa et al and Subhas et al proposed treatment algorithms that were based on the presence of symptom [10, 11]. However, the validity of these therapeutic algorithms remains to be established. To establish the therapeutic strategies, randomized clinical trials (RCTs) should ideally be performed, because the RCTs avoid evaluation bias and objectively evaluate the therapeutic effects. As a considerable number of cases are needed to perform RCTs, these trials are not suitable for spontaneous isolated dissection of abdominal visceral arteries. Therefore, detailed descriptions of clinical features as provided in our study are important.
In conclusions, we clarified the clinical conditions of patients with spontaneous isolated dissection of abdominal visceral arteries. Our findings suggest that hypertension and smoking might be involved in the pathogenesis of this disease and that this disease can occur without symptoms.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
Authors declare no conflict of interest.
Informed Consent
The purpose of the present study was explained to all participants in the documents of the study, and a written informed consent was obtained from all individual participants.
Author Contributions
HS, KA, SK, YF, WS and NI conceived and designed the research. HS, MK and MY contributed to the data collection. NI wrote the first draft. KA, SK and YF contributed to the writing of the manuscript. All authors agreed with the final results and conclusions.
| References | ▴Top |
- Tanaka Y, Yoshimuta T, Kimura K, Iino K, Tamura Y, Sakata K, Hayashi K, et al. Clinical characteristics of spontaneous isolated visceral artery dissection. J Vasc Surg. 2018;67(4):1127-1133.
doi pubmed - Morgan CE, Mansukhani NA, Eskandari MK, Rodriguez HE. Ten-year review of isolated spontaneous mesenteric arterial dissections. J Vasc Surg. 2018;67(4):1134-1142.
doi pubmed - Sun J, Li DL, Wu ZH, He YY, Zhu QQ, Zhang HK. Morphologic findings and management strategy of spontaneous isolated dissection of the celiac artery. J Vasc Surg. 2016;64(2):389-394.
doi pubmed - Mousa AY, Coyle BW, Affuso J, Haser PB, Vogel TR, Graham AM. Nonoperative management of isolated celiac and superior mesenteric artery dissection: case report and review of the literature. Vascular. 2009;17(6):359-364.
doi pubmed - Nagai T, Torishima R, Uchida A, Nakashima H, Takahashi K, Okawara H, Oga M, et al. Spontaneous dissection of the superior mesenteric artery in four cases treated with anticoagulation therapy. Intern Med. 2004;43(6):473-478.
doi pubmed - Wagner WH, Allins AD, Treiman RL, Cohen JL, Foran RF, Levin PM, Cossman DV. Ruptured visceral artery aneurysms. Ann Vasc Surg. 1997;11(4):342-347.
doi pubmed - Park YJ, Park CW, Park KB, Roh YN, Kim DI, Kim YW. Inference from clinical and fluid dynamic studies about underlying cause of spontaneous isolated superior mesenteric artery dissection. J Vasc Surg. 2011;53(1):80-86.
doi pubmed - Wu Z, Yi J, Xu H, Guo W, Wang L, Chen D, Xiong J. The significance of the angle between superior mesenteric artery and aorta in spontaneous isolated superior mesenteric artery dissection. Ann Vasc Surg. 2017;45:117-126.
doi pubmed - Kimura M, Matsuda T, Fukase K, Okumoto K, Mabe K, Suzuki K, Aoyama I, et al. [Clinical study of dissection of the superior mesenteric artery]. Nihon Shokakibyo Gakkai Zasshi. 2002;99(2):145-151.
- Satokawa H, Takase S, Seto Y, Yokoyama H, Gotoh M, Kogure M, Midorikawa H, et al. Management strategy of isolated spontaneous dissection of the superior mesenteric artery. Ann Vasc Dis. 2014;7(3):232-238.
doi pubmed - Subhas G, Gupta A, Nawalany M, Oppat WF. Spontaneous isolated superior mesenteric artery dissection: a case report and literature review with management algorithm. Ann Vasc Surg. 2009;23(6):788-798.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


