| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 9, Number 3, March 2017, pages 221-224
Atypical Double Right Coronary Artery Presenting With Acute Coronary Syndrome, Cardiogenic Shock and Complete Heart Block
Santosh Kumar Sinhaa, b, Shravan Singha, Vikash Chaturvedia, Puneet Agrawala, Mahmadula Razia, Anupam Mahrotraa, Vikas Mishraa, Mukesh Kumara, Nasar Abdalia, Dibbendhu Khanraa, Ramesh Thakura, Chandra Mohan Varmaa, Umeshwar Pandeya
aDepartment of Cardiology, LPS Institute of Cardiology, G. S. V. M. Medical College, Kanpur, Uttar Pradesh 208002, India
bCorresponding Author: Santosh Kumar Sinha, Department of Cardiology, LPS Institute of Cardiology, G. S. V. M. Medical College, Kanpur, Uttar Pradesh 208002, India
Manuscript accepted for publication December 08, 2016
Short title: Atypical Double Right Coronary Artery
doi: https://doi.org/10.14740/jocmr2848w
| Abstract | ▴Top |
Double right coronary artery (RCA) is an extremely rare coronary artery anomaly. We here report an atherosclerotic double RCA which appeared after primary percutaneous intervention performed to treat a 34-year-old male presenting with acute inferior myocardial infarction, cardiogenic shock and complete heart block. This is an unusual case as double RCA had been hidden by total atherosclerotic occlusion of the proximal part of the RCA and complete restoration of patency led complete heart block back to normal sinus rhythm.
Keywords: Coronary artery anomaly; Double right coronary artery; Complete heart block; Cardiogenic shock; Myocardial infarction
| Introduction | ▴Top |
The prevalence of congenital anomalies of the coronary arteries (CAAs) is reported to be approximately 0.2-1.4% in the general population [1]. Of them, the double right coronary artery (RCA) is one of the rare coronary anomalies. It may be benign appearing as an incidental finding on routine coronary angiogram or sometimes, may be complicated with atherosclerosis and present with spectrum from stable coronary artery disease to acute coronary syndrome with stormy course.
| Case Report | ▴Top |
A 34-year-old male was admitted to emergency department with retrosternal chest pain at rest of 4 h duration with perspiration and occasional dizziness. His risk factors were smoking and dyslipidemia. On physical examination, skin was cold and clammy. Blood pressure was 94/72 mm Hg with pulse rate of 61/min. Electrocardiogram showed ST elevation in leads II, III, and aVF, reciprocal changes in leads I and aVL, and complete heart block (Fig. 1a). His routine biochemistry was normal. He was preloaded with 325 mg aspirin, 40 mg rosuvastatin and 60 mg prasugrel along with IV fluids and vasopressors. Temporary pacing wire was kept as standby. Echocardiography revealed hypokinesia in RCA territory with ejection fraction of 48%. After proper consent, he was shifted to catheterization lab. Coronary angiography was performed through right femoral artery. It showed total occlusion of the proximal RCA (Fig. 2). The left coronary arteries were of normal origin and distribution with normal flow in left anterior descending artery (LAD) and circumflex artery (LCx). Unfractionated heparin 6,000 U was administered. RCA was hooked with a 3.5 Judkin’s right 6 F guiding catheter (Medtronic, USA). Lesion was crossed with a 0.014" 140 cm fielder FC wire with help of a finecross microcatheter (Asahi, Japan) (Fig. 3). Once parked distally, finecross was advanced and fielder FC was exchanged with a 0.014" 140 cm BMW wire (Abott, USA). Finecross was removed by nanto’s technique. Distal tip of BMW wire was not in typical distribution of RCA but as we encountered, no resistance and movement of distal tip along with the feel was sufficient to say that it was in true lumen (Fig. 4a). We treated him with upstream tirofiban (10 µg/kg/3 min) and dilated with a 2 × 10 mm Minitrak balloon (Abott, USA) (Fig. 4b). Contrast injection this time showed one large branch going beyond crux giving posterior descending artery and two parallel large coronary arteries distally. Wire was parked into larger branch by further manipulation. Lesion was stented with a 3.5 × 23 mm Xience Prime drug-eluting stent (Abott, USA) (Fig. 4c) and post-dilated by a 3.5 × 10 Minitrak NC balloon (Abott, USA) achieving TIMI III flow (Fig. 4d). Control coronary angiogram demonstrated atypical double RCA as there were two parallel coronary arteries distal to the occlusion (Fig. 5). During his hospital stay, complete heart block reverted to 2:1 atrioventricular block, and then went back to normal sinus rhythm on third day (Fig. 1a, b, c, d). He was discharged in stable condition with dual antiplatelets, statin, and beta blocker.
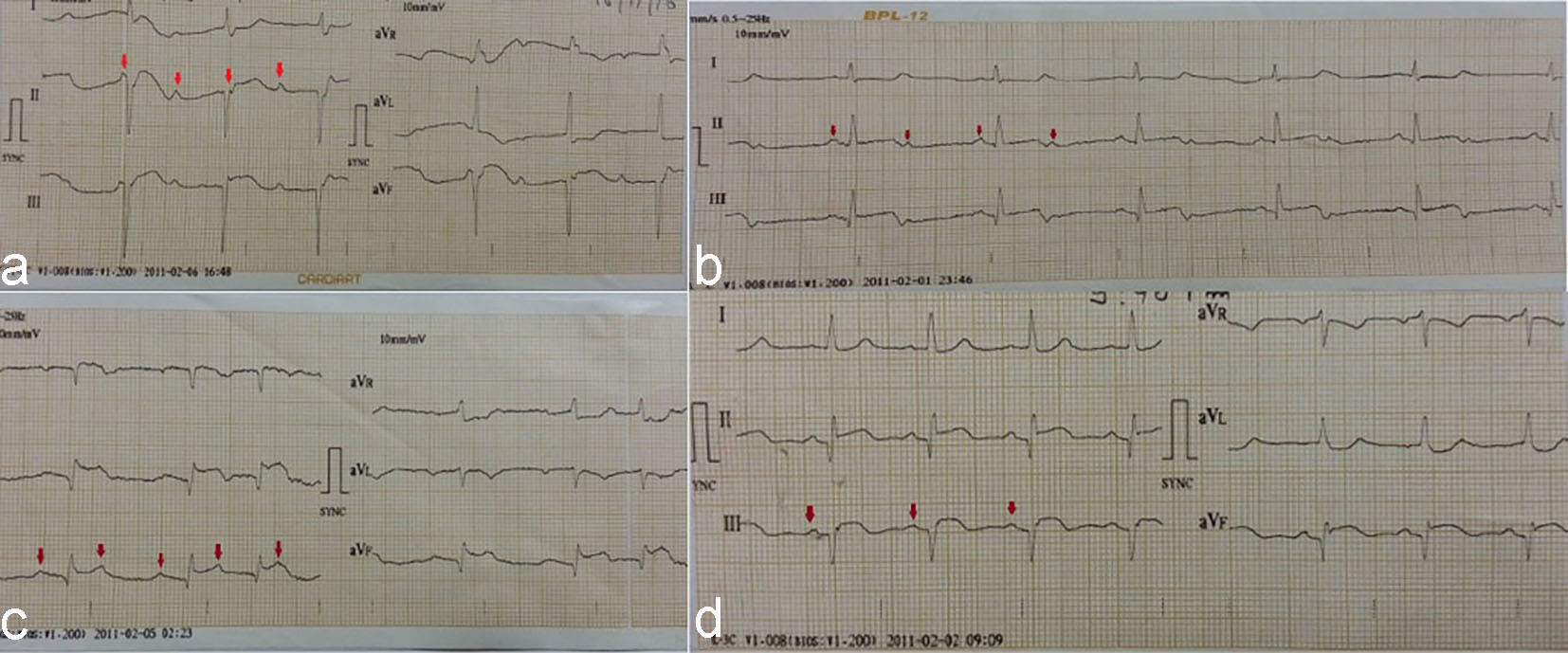 Click for large image | Figure 1. (a) Electrocardiogram showing complete heart block; (b) 2:1 atrioventricular block; (c) Wenckebach phenomenon; (d) Normal sinus rhythm. |
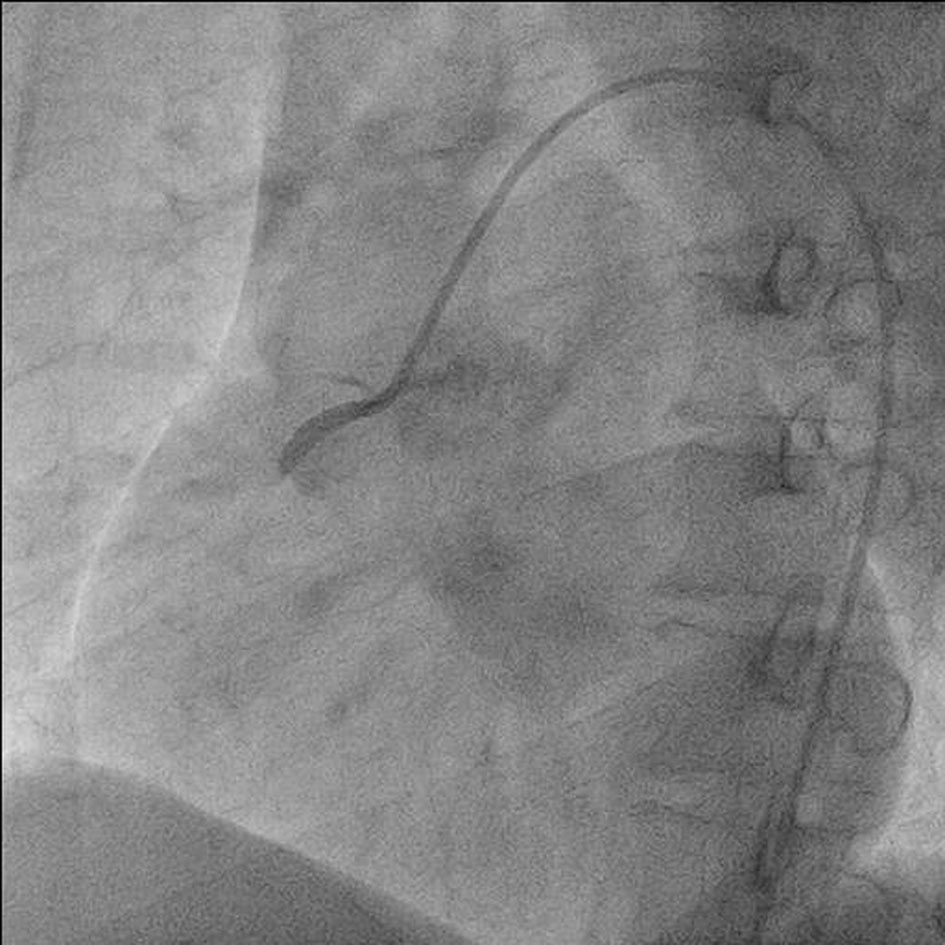 Click for large image | Figure 2. Basal angiogram showing occlusion of proximal RCA. |
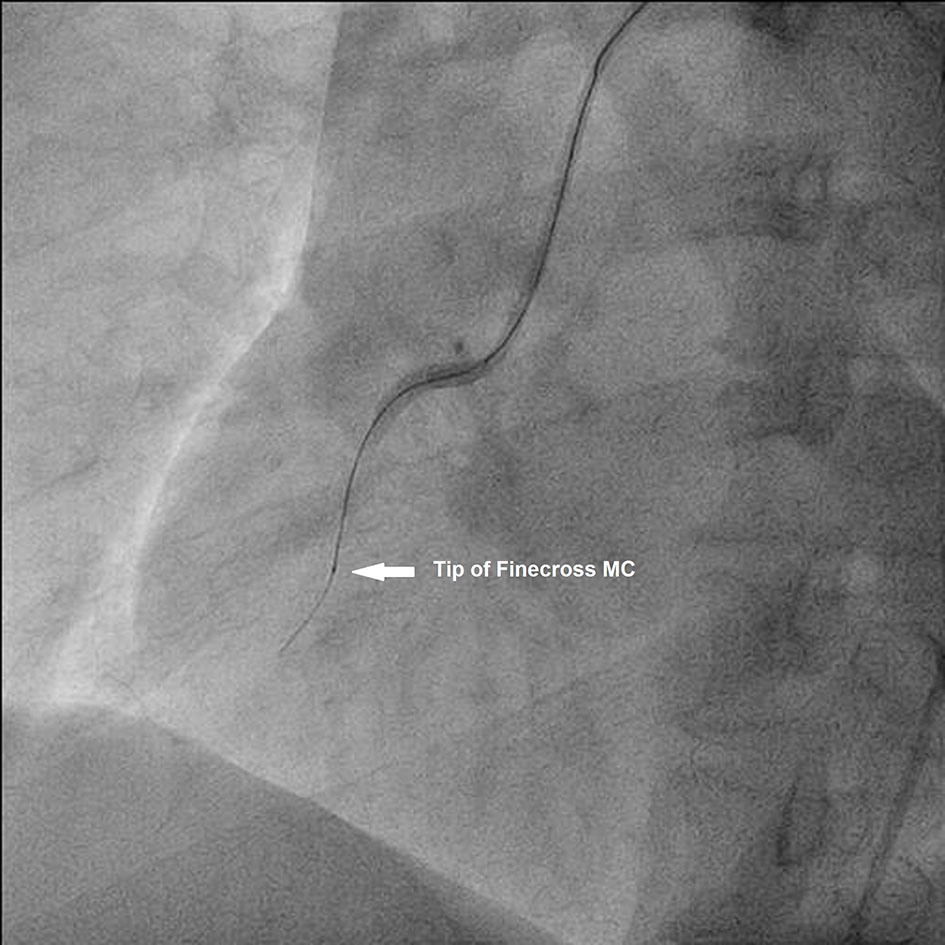 Click for large image | Figure 3. Fielder FC guide wire over finecross microcatheter beyond the lesion. |
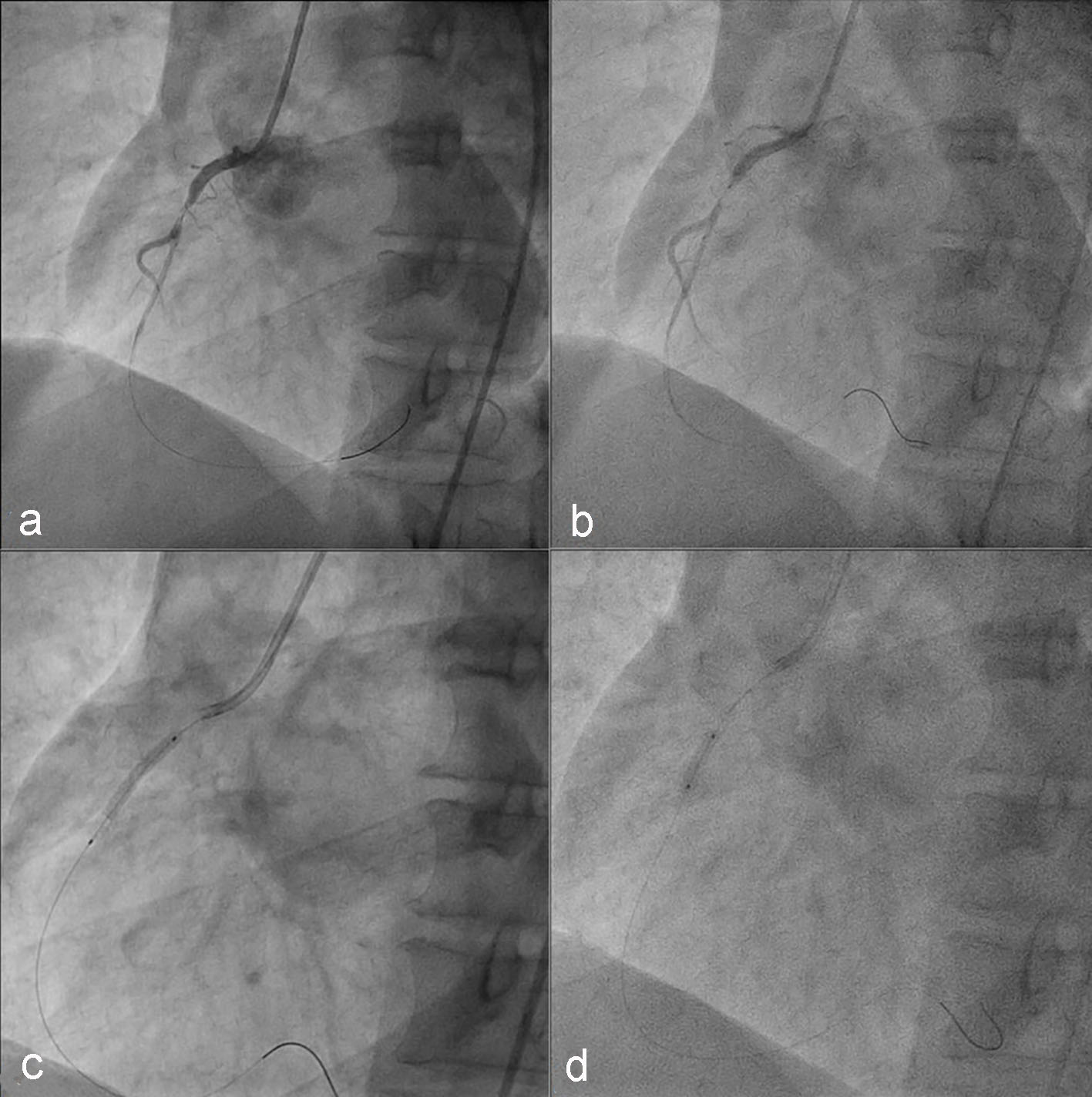 Click for large image | Figure 4. (a) BMW guide wire parked distally after exchange with Feider wire; (b) lesion being predilated with 2 × 10 Minitrak balloon; (c) stent being deployed across the lesion; (d) stent being post-dilated with non-compliant balloon. |
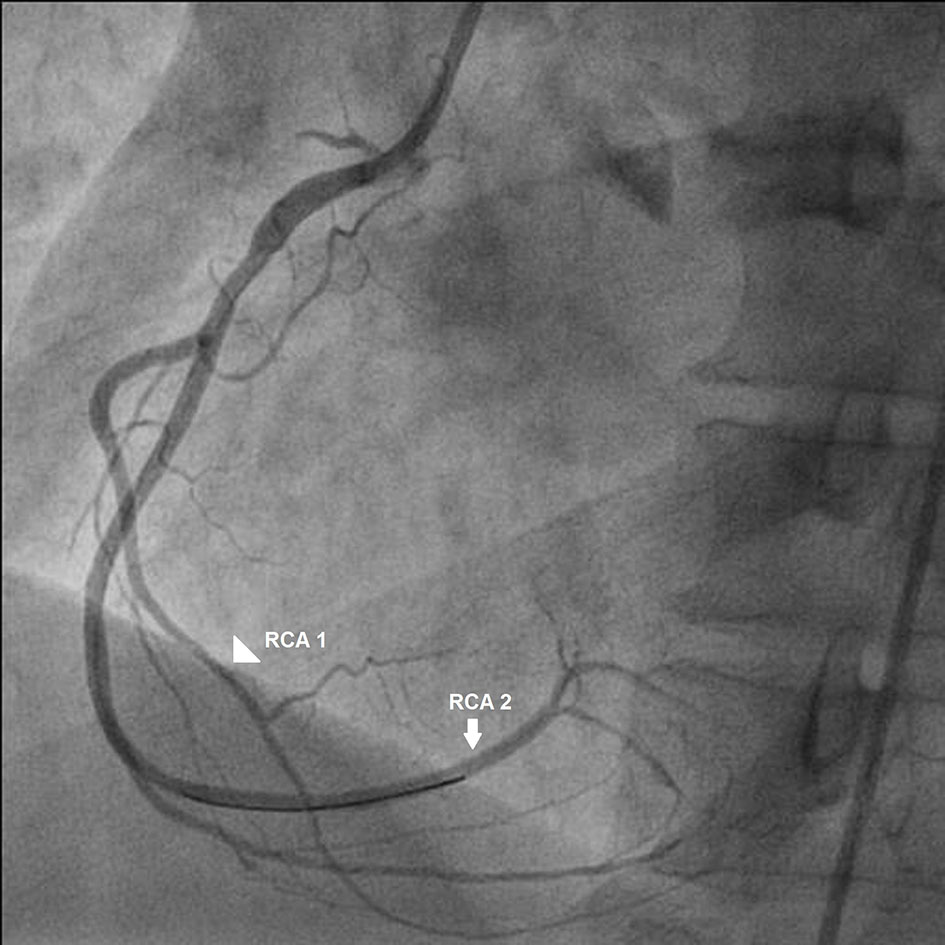 Click for large image | Figure 5. Atypical right coronary artery after stent deployment. |
| Discussion | ▴Top |
Double RCA is a very rare coronary anomaly, whose true definition and correct diagnosis remain controversial [2, 3]. Sometimes, it is very difficult to distinguish double RCA with single orifice from RCA which has a high take-off of a large right ventricular artery. Right anterior oblique (RAO) view may be helpful in differentiating double RCA from a large right ventricular branch as it provides better demonstration of artery courses in such circumstances [4]. Sato et al have proposed that double RCAs are defined when they supply the blood to the inferior left myocardium, thus both of the RCAs should course downwardly to reach the interventricular sulcus whether or not they cross the crux [5]. The first report about double RCA anomaly in the literature was by Barthe et al [6]. They observed double RCA originated from one ostium. The vessels were within the right atrioventricular groove. After the origin of a conus artery and a ventricular branch, the most anterior RCA descended toward the acute margin of the heart and terminated in a small posterior descending artery. The second RCA terminated in a small posterior descending and posterolateral branches. In our cases, both RCAs were almost identical in size and both gave rise to a PDA. By using this reasonable classification, we diagnosed our case as atypical double RCA. Since the first report, this rare anomaly has been accepted as a benign entity. However, its involvement with atherosclerosis has also been reported, where revascularisation had been performed either by coronary artery by-pass surgery or elective percutaneous coronary intervention (PCI) [7, 8]. It may be associated with tachyarrhythmia as reported by Ozeren et al [9]. Rohit et al have reported primary PCI of double RCA presenting with acute inferior wall infarction but there was no rhythm disturbance in their case [10]. To the best of our knowledge and after extensive search in medical literature, we are reporting for the first time, double RCA presenting with complete heart block with cardiogenic shock where primary PCI was performed. After complete revascularization, the rhythm was restored to normal. RCA maintains a course in the atrioventricular groove and forms the uppermost portion of the posterior descending branch. The length of each of the two posterior descending branches varies from patient to patient: in our patient, both the branches were large; therefore, their occlusion was responsible for the symptoms.
Conflicts of Interest
None.
| References | ▴Top |
- Angelini P, Villason S, Chan AV Jr, Diez JG. Normal and anomalous coronary arteries in humans. In: Angelini P, editor. Coronary artery anomalies: a comprehensive approach. Baltimore: Lippincott Williams & Wilkins; 1999. p. 27-79.
- Tuncer C, Batyraliev T, Yilmaz R, Gokce M, Eryonucu B, Koroglu S. Origin and distribution anomalies of the left anterior descending artery in 70,850 adult patients: multicenter data collection. Catheter Cardiovasc Interv. 2006;68(4):574-585.
doi pubmed - Sari I, Kizilkan N, Sucu M, Davutoglu V, Ozer O, Soydinc S, Aksoy M. Double right coronary artery: report of two cases and review of the literature. Int J Cardiol. 2008;130(2):e74-77.
doi pubmed - Altun A, Akdemir O, Erdogan O, Ozbay G. An interesting diagnostic dilemma: double right coronary artery or high take off of a large right ventricular branch. Int J Cardiol. 2002;82(1):99-102.
doi - Sato Y, Kunimasa T, Matsumoto N, Saito S, et al. Detection of double right coronary artery by multi-detector row computed tomography: is angiography still gold standard? International Journal of Cardiology. 2008;126(1):134-135.
doi - Barthe JE, Benito M, Sala J, Houbani AJ, Quintana E, Esplugas E, Gausi C. Double right coronary artery. Am J Cardiol. 1994;73(8):622.
doi - Sari I, Uslu N, Gorgulu S, Nurkalem Z, Eren M. Inferior myocardial infarction and extensive atherosclerosis in a patient with double right coronary artery. Int J Cardiol. 2006;111(2):321-323.
doi pubmed - Tatli E, Buyuklu M, Altun A, Yilmaztepe M. A patient with double right coronary artery and acute inferior myocardial infarction due to the critical lesion in one of them. Int J Cardiol. 2007;119(1):e30-31.
doi pubmed - Ozeren A, Aydin M, Bilge M, Dursun A, Onuk T. Atherosclerotic double right coronary artery and ectasia of left coronary arteries in a patient with presented acute coronary syndrome and ventricular tachycardia. Int J Cardiol. 2005;102(2):341-343.
doi pubmed - Rohit M, Bagga S, Talwar KK. Double right coronary artery with acute inferior wall myocardial infarction. J Invasive Cardiol. 2008;20(2):E37-40.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


