| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 9, Number 1, January 2017, pages 17-22
Use of a Respiratory Volume Monitor to Assess Respiratory Competence in Cardiac Surgery Patients After Extubation
Stephan Ianchuleva, Diane Laddb, e, C. Marshall MacNabbc, Lizeng Qind, Nathan Marengia, Jenny Freemanc
aTufts Medical Center, Boston, MA, USA
bWest Virginia University, Morgantown, WV, USA
cRespiratory Motion, Inc., Waltham, MA, USA
dHarvard Medical School, Boston, MA, USA
eCorresponding Author: Diane Ladd, West Virginia University, 411 Waverley Oaks Rd., Morgantown, WV, USA
Manuscript accepted for publication August 19, 2016
Short title: Non-Invasive Respiratory Monitor
doi: https://doi.org/10.14740/jocmr2033w
| Abstract | ▴Top |
Background: Patients who have undergone cardiac surgery are generally mechanically ventilated postoperatively. Early postoperative extubation is currently recommended in anesthesia guidelines. No current technology can accurately, non-invasively, measure respiratory competence after extubation. Pulse oximetry has been helpful, but this is a late indicator of respiratory compromise. A novel, non-invasive, respiratory volume monitor (RVM) has been shown to deliver accurate continuous, real-time minute ventilation (MV), tidal volume (TV) and respiratory rate (RR) measurements and provide an objective measure of respiratory competence. The RVM will accurately reflect MV, TV and RR in cardiac surgery patients before and after extubation.
Methods: RVM traces were recorded from patients before and after cardiac surgery. Continuous monitoring began on admission to the unit and was ended at 24 h after extubation. RVM-based MV, TV and RR were calculated from 30-s segments. MV, TV and RR were also continuously recorded from the ventilator prior to extubation. The RVM was calibrated to each patient using the readings from the ventilator.
Results: During mechanical ventilation, the RVM measured TVs strongly correlated with the ventilator TVs (r = 0.97). Following extubation, the patient’s breathing became more erratic and TVs and MVs decreased. Within 1 h, all patients studied showed a marked recovery of MV and TV.
Conclusions: RVM-based MV, TV and RR correlated well with similar data collected from ventilators. After extubation, RVM shows promise as a means to monitor respiratory competence of non-intubated patients, and has implications for use in other settings and improving patient safety.
Keywords: Non-invasive; Respiratory volume monitor; Ventilation; Postoperative
| Introduction | ▴Top |
The most recent National Hospital Discharge Survey reported over 400,000 patients underwent cardiac surgery in the United States in 2010 [1]. In cardiac patients, respiratory problems following extubation are the most significant cause of postoperative comorbidity, despite considerable improvement in postoperative care and monitoring [2]. In a recent study of 7,105 cardiac patients, 216 were readmitted to the intensive care unit (ICU) due to respiratory complications [3]. This represented 39% of all ICU readmissions in that study. In recent study of the 7.8% of patients readmitted to the ICU following cardiac surgery, respiratory failure was reported to be the cause for 39% of them [2, 4]. Current trends in cardiac anesthesia recommend early extubation, but that is not always feasible and prolonged endotracheal intubation and mechanical ventilation place cardiac patients at an increased risk of respiratory complications. Previous data show that the airway can constrict immediately after extubation as a result of mechanical irritation to the upper airway and prolonged supine position [2]. Cardiopulmonary bypass patients are at an even greater risk since they can develop temporary pulmonary ischemia that decreases the production of surfactant and stiffens respiratory tissue [2]. Timely detection and prevention of respiratory compromise in this population has become a priority [5]. Despite the inherent dangers caused by respiratory complications, current in-hospital monitoring is still lacking.
A non-invasive technology that could reliably measure respiratory function after extubation and give early warning signs of respiratory compromise before harmful events occurred could markedly improve patient care and safety. Subjective clinical assessment and respiratory rate (RR) monitoring are both inconsistent and unreliable indicators of respiratory sufficiency, and current clinical practice relies heavily on continuous pulse oximetry or capnography.
Though used in almost every clinical setting, pulse oximetry can be unreliable and studies have shown nearly two-thirds of alarms triggered by the oximeter to be false [6, 7]. Furthermore, oxygen saturation is a lagging indicator, as it decreases only after a significant drop in ventilatory adequacy and readings are often confounded by the use of supplemental oxygen leading to possible delay in interventions and risk to patient safety.
Capnography, while useful in intubated patients, is limited after extubation. It is a qualitative indicator with limited utility in non-intubated patients. One of the difficulties with capnography in the non-intubated patients is patient compliance and maintaining proper placement of the sampling cannula [8]. Both oximetry and capnography are indirect measurements of respiratory performance, as they do not directly monitor the adequacy of respiration, but are rather surrogate measures of respiratory status.
Direct measurement of respiratory performance in non-intubated patients has been a challenge. While a skilled clinician may measure a patient’s RR by counting chest wall movements, an obstructed airway or chest muscle contraction could result in this same movement rather than true respiratory effort. In the obese population, observing a chest rise and fall is increasingly challenging and even if one can accurately count the RR, one would not be able to easily distinguish between adequate and inadequate breathing. The currently available measures are limited and often do not provide enough clinically relevant information to trigger healthcare provider response and early intervention to prevent respiratory compromise [9].
Recent development of a non-invasive respiratory volume monitor (RVM) that provides quantitative, continuous, real-time measurements of MV, TV and RR in non-intubated patients has addressed a number of these challenges. With the recommended electrode placement and calibration algorithms, strong correlations (0.96 ± 0.16, mean ± 95% CI for regular and erratic breathing) between RVM and spirometric measurements have been previously demonstrated [10]. The RVM can quantify ventilation in non-intubated patients and help identify patients at risk for respiratory complications following cardiac surgery and in other clinical settings [11-15]. However, RVM had been evaluated in post-sternotomy patients. The goal of this study was to demonstrate that an alternate electrode placement, to accommodate the sternal dressing, would not affect the RVM correlations to the ventilator and to show the utility of using RVM to monitor MV, TV, and RR in cardiac surgery patients after median sternotomy. It was hypothesized RVM would provide accurate, continuous measurements of MV, TV, and RR in this cohort before and after extubation.
| Methods | ▴Top |
Fourteen cardiothoracic patients (four females and 10 males, average age 69 ± 11.8 years, average BMI 29 ± 6.0 kg/m2, eight coronary artery bypasses, four valve replacements, and two myomectomies, Table 1) were enrolled in an IRB approved protocol for monitoring respiratory status in the Tufts cardiothoracic unit (CTU). Respiratory traces were recorded from thoracic electrodes using an impedance-based RVM system (ExSpiron, Respiratory Motion, Inc., Waltham, MA) throughout the postoperative stay in the CTU. All cardiothoracic procedures were performed under general anesthesia and all patients arrived in the CTU intubated and sedated. Upon arrival in the CTU, the ExSpiron electrode PadSet was positioned to the right of the sternal dressing, approximately at the right mid-clavicular line, instead of the standard midsternal placement. The device was calibrated while the patient was on the ventilator (Puritan-Bennett 840, Covidien, Mansfield, MA) during synchronous intermittent mandatory ventilation mode (SimV) with setting at 6 - 8 mL/kg IBW as determined by the anesthesiologist. Respiratory data (MV, TV and RR) were acquired only every 15 s from the ventilator, as the ventilator did not support continuous respiratory trace streaming. RVM-based MV, TV, and RR were calculated from continuous 30-s segments. Simultaneous recordings were collected from the ventilator prior to extubation. RVM data were recorded continuously from CTU arrival until 24 h after extubation or CTU discharge, whichever occurred first. Arterial blood gases were collected before extubation and again approximately 1 - 2 h after extubation in a subset of patients (n = 12) as deemed necessary by the surgical care team.
 Click to view | Table 1. Subject Demographics |
| Results | ▴Top |
RVM traces were continuously recorded in the CTU for 27 ± 3.7 h (6 - 49 h). After extubation, patients remained in the CTU and were monitored by the RVM for another 18 ± 2.5 h (2 - 29 h). Twelve of 14 of the patients had ventilator reading for analysis. During mechanical ventilation, TVs measured by the RVM strongly correlated with TVs reported by the ventilator (r = 0.97). This correlation was maintained during both mandatory ventilation (SIMV) and during spontaneous breathing with pressure support (PS) modes. Patient average error in TV measurements between RVM and the ventilator was -2.6%, the average precision was 23.9% and average accuracy was 26.2%. An example of simultaneous RVM and ventilator recordings for 30 min is shown in Figure 1. During this time, the ventilator measured an average MV of 6.3 L/min, a TV of 520 mL, and a rate of 12 breaths/min, while RVM measured an average MV of 5.9 L/min (7% error), an average TV of 490 mL (6% error), and an average RR of 12.2 breaths/min (3% error).
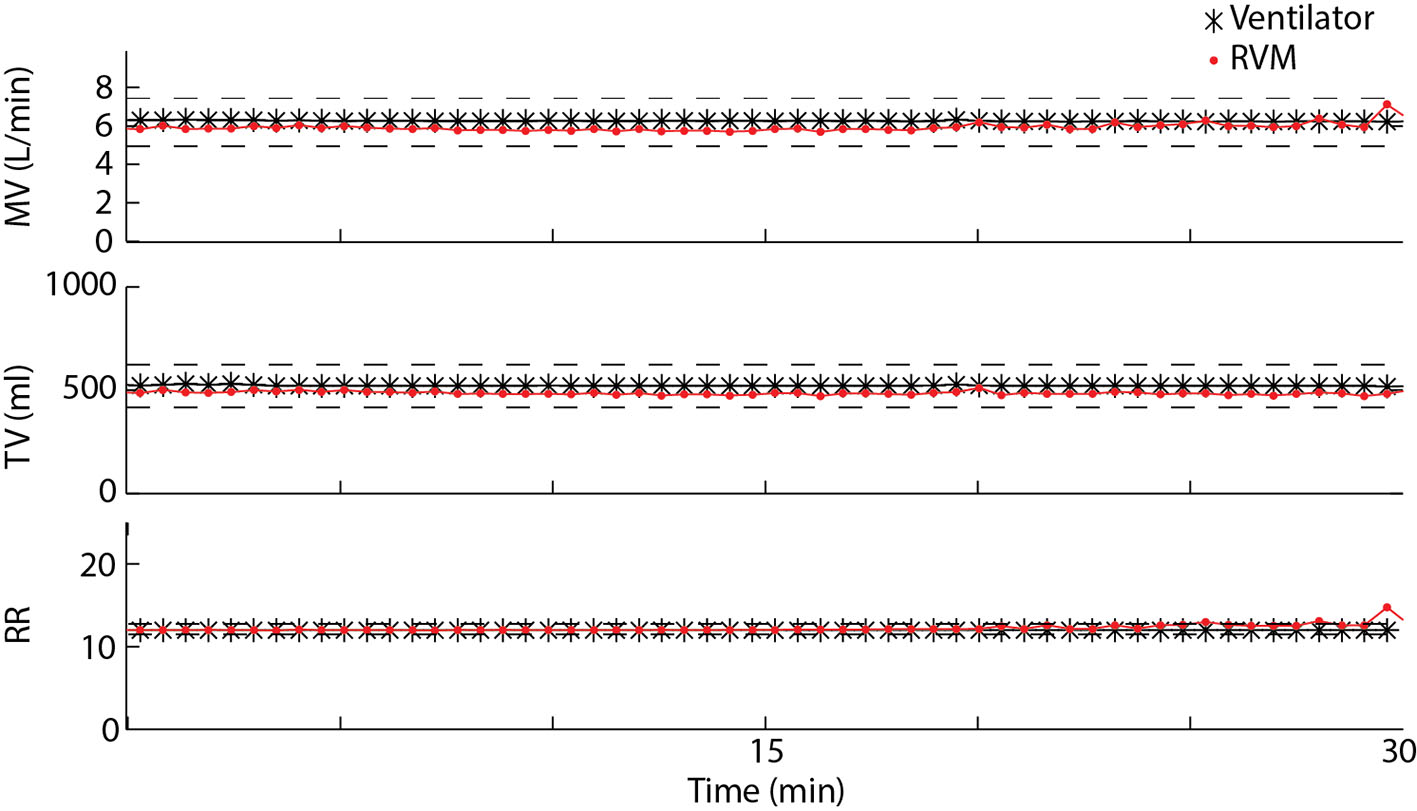 Click for large image | Figure 1. Measured MV, TV, and RR over a 30-min period using RVM (red) and the Puritan Bennett ventilator in SimV mode (black) for one example patient. Average errors between RVM and the ventilator for MV, TV, and RR are less than 10%. |
Before and after extubation, the RVM recorded respiratory traces continuously, in real-time, and captured a distinct pattern of post-extubation respiratory variation. Based on body surface area, the average predicted MV was calculated to be 7.6 ± 0.6 L/min for the 14 patients. During 2 min of breathing on SimV mode on the ventilator, the average baseline ventilation was slightly above the predicted at 8.2 ± 0.4 L/min (109±5% of predicted). Analysis of the ExSpiron data from the 14 studied patients showed MV was significantly reduced 30 min after extubation to 77±9% of baseline (8.2 ± 0.4 to 6.4 ± 0.9 L/min, P < 0.05) and TV was significantly reduced to 71±9% of baseline (520 ± 40 to 370 ± 40 mL, P < 0.01) relative to the pre-extubation baseline MV (Table 2, Fig. 2a, b). After 30 min, MV began to increase and by 60 min after extubation, average MV and TV had returned to baseline levels (MV: 118±16% of baseline (9.6 ± 1.2 L/min); TV: 105±16% of baseline (490 ± 50 mL); P > 0.4). Importantly, RR remained practically unchanged after extubation, displaying no systematic variation. Thirty minutes after extubation, RR was 113±8% of baseline (17.1 ± 1.5 to 17.5 ± 1.0 breaths/min, P = 0.4). It is important to note that RR is the only direct and continuous respiratory parameter currently monitored after extubation. SaO2 monitoring was recorded every hour by the nursing staff and revealed no significant drops in blood oxygen saturation after extubation (Fig. 2c, average 97±1%, 91-100%).
 Click to view | Table 2. Respiratory Metrics Before and After Extubation (N = 14) |
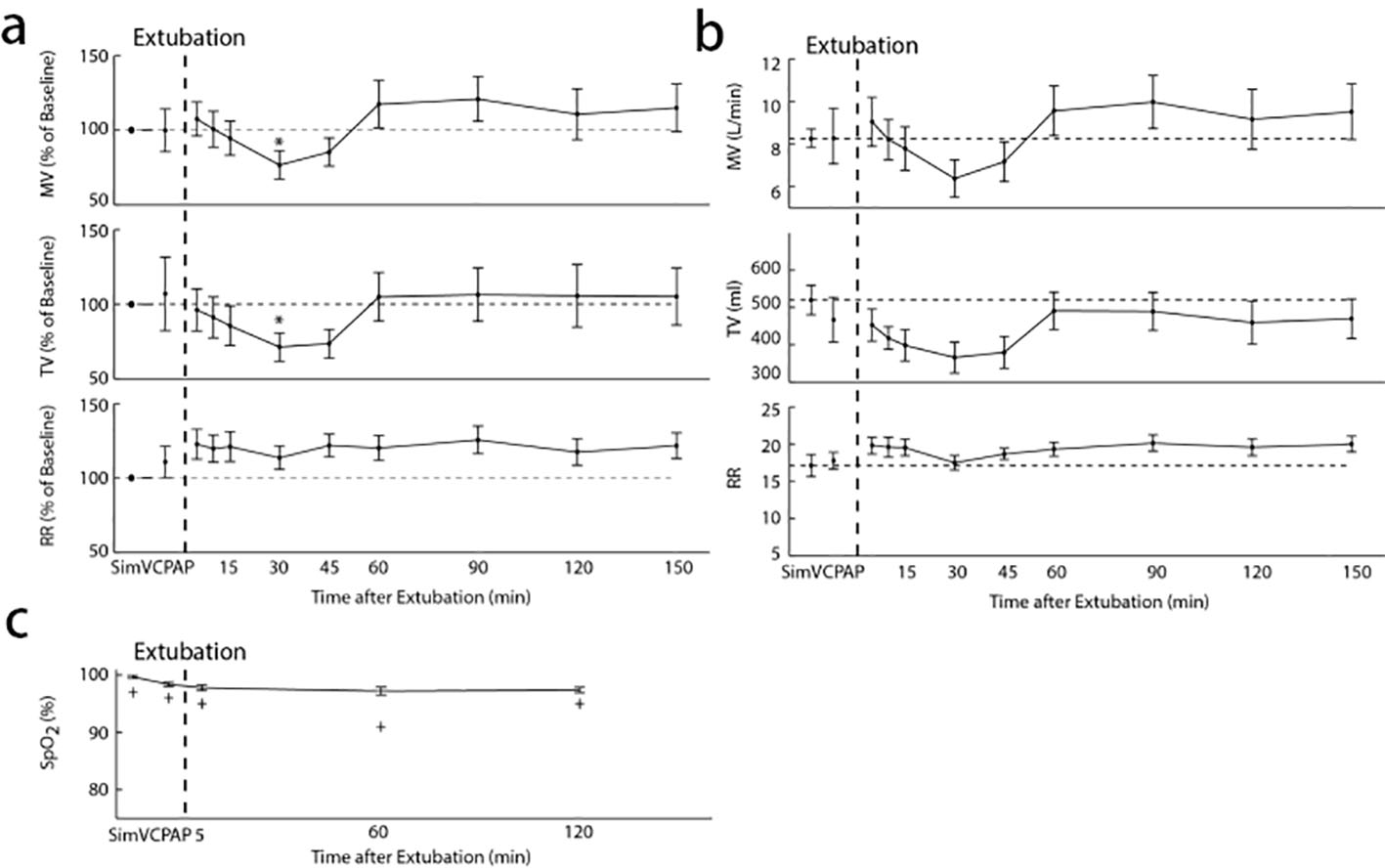 Click for large image | Figure 2. (a) MV, TV, and RR as percent of baseline before and after extubation. A nadir in ventilation occurs 30 min after extubation with MV significantly reduced to 77±9% of baseline (*P < 0.05) and TV significantly reduced to 71±9% of baseline (*P < 0.01), while RR is not significantly different at 113±8% of baseline. Sixty minutes after extubation, MV has returned to 118±16% of baseline and TV has returned to 105±16% of baseline. (b) Absolute values of MV, TV, and RR measured before and after extubation. MV falls significantly from 8.2 ± 0.4 L/min at baseline to 6.4 ± 0.9 L/min 30 min after extubation and TV was significantly reduced from 520 ± 40 mL at baseline to 370 ± 40 mL after extubation. (c) Average SpO2 values recorded before and after extubation. The minimum SpO2 value recorded at each time point among all subjects is shown as a “+”. |
Blood gas measurements were taken on average 56 ± 25 min before extubation and 106 ± 27 min after extubation. SpO2 remained unchanged from before to after extubation (98 ± 0.4 vs. 98 ± 0.8, P = 0.21, Table 3). PCO2, PaCO2 and pH also showed no significant differences (Table 3). There was a slight significant increase in bicarbonate from before to after extubation, but was of no clinical importance (21.3 ± 0.5 vs. 22.3 ± 0.4, P = 0.04). Figure 3 shows RVM traces from a representative post-extubation course.
 Click to view | Table 3. Blood Gases Before and After Extubation |
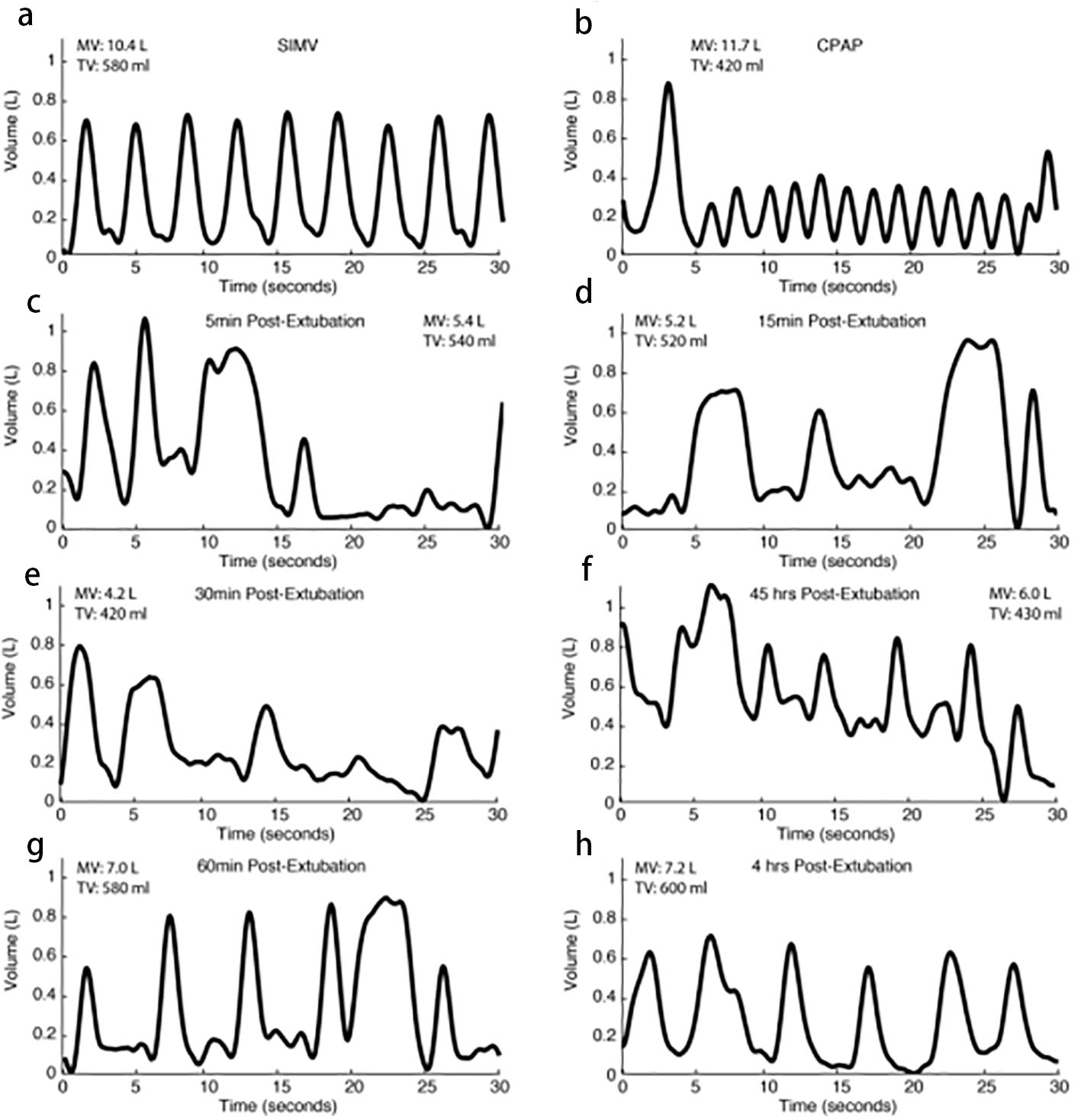 Click for large image | Figure 3. Example respiratory traces from a representative patient (60-year-old male, BMI 29). Initial traces reflect ventilator breaths only with no spontaneous ventilation (a). As the patient awakes from anesthesia and progresses toward extubation, faster and shallower spontaneous breaths predominate with an occasional ventilator breath (b). Just after extubation, the patient’s breathing pattern is more irregular (c, d) and TVs and MVs decrease (d, e). TV and MV measurements increase over time after successful extubation (f, g, h). |
Conclusions
While intubated, RVM-based MV, TV and RR correlated well with CTU ventilator measurements in patients after median sternotomy. After extubation, RVM continuously reported MV, TV and RR, providing a continuous, non-invasive, quantitative assessment of respiratory competence. A pattern of MV and TV decrease during the first 30 min after extubation was noted in all patients. Subsequent recovery to pre-extubation levels within 1 h as confirmed by PaCO2 from arterial blood gas was noted in all patients. RVM showed distinct changes in MV and TV after extubation, while RR showed no significant variations. Although no patients in this study required reintubation, based on data from other studies collected after extubation in premature infants, we propose that patients who continue to have a decrease in MV with no rise to baseline within 1 h after extubation will require intervention such as non-invasive ventilation or reintubation. Further studies to evaluate the use of RVM in postoperative cardiac surgical patients for early detection of respiratory failure for development of reintubation protocols are ongoing.
This study demonstrated that, while intubated, RVM-based MV, TV and RR correlated well with ventilator measurements (r = 0.97). In addition, the change in the PadSet placement to accommodate the sternal wound and dressing did not affect the device measurements. This confirms that the RVM can provide accurate measurements of MV, TV and RR in patient’s post-median sternotomy using the modified positioning of the electrode PadSet. After extubation, RVM continuously reported MV, TV and RR, providing a real-time, non-invasive, quantitative assessment of respiratory competence. A pattern of MV and TV decrease during the first 30 min after extubation was noted. Subsequent recovery to pre-extubation levels within 1 h as confirmed by PaCO2 from arterial blood gas was noted in all patients. This shows that RVM is capable of providing patterns and trends in ventilation status not available to healthcare providers with other technology.
Respiratory complications are one of the leading causes of readmission to the ICU for cardiac surgery patients [16]. This study shows the benefits of this new technology and its application in the CTU and possibly other locations. Pulse oximetry is the leading technology used to assess respiratory status in non-intubated patients; however, SpO2 levels do not begin to decline until well after respiratory decompensation has begun and is known for being prone to inaccuracies [13, 17]. Intermittent blood gas measurements were taken intermittently and on average over 1 h after extubation, well after RVM confirmed a recovery in MV. RVM showed distinct changes in MV and TV after extubation, while RR, generally measured with cardiac monitoring, showed no significant variations.
The time it takes a patient to return to baseline MV is inversely proportional to successful extubation, therefore demonstrating the importance of obtaining MV measurements [18]. Additionally, determination of MV after extubation using RVM could potentially aid in quicker assessment of the necessity and timing of reintubation, or provide an early indication of when institute non-invasive ventilation (NIV), in the form of continuous positive airway pressure or biphasic positive airway pressure. Although no patients in this study required reintubation, based on data from other studies collected after extubation in premature infants, it is hypothesized that patients who continue to have a decrease in MV with no rise to baseline within 1 h after extubation will require intervention such as non-invasive ventilation or reintubation.
Recently, the American Society of Anesthesiology has voiced the opinion that quantitative monitoring of respiratory status is superior over qualitative methods [19]. Qualitative clinical signs such as chest excursion and auscultation of breath sounds are useful, but they can only be obtained periodically and are often inaccurate. Carbon dioxide monitoring is also a qualitative sign of respiration in non-intubated patients and its accuracy is dependent on many factors. However, non-invasive MV and TV have been previously unavailable in non-intubated patients. The RVM fills this gap. By providing MV and TV, the RVM permits a more comprehensive, quantitative assessment of respiratory status. With this functionality, RVM-derived respiratory data can bring forth reproducible and comparable data across patients over a wide range of breathing patterns. This can promote better evaluation of respiratory status in the CTU and other healthcare settings.
Funding
The study was supported by Respiratory Motion, Inc.
Conflicts of Interest
Dr. Ianchulev, Dr. Qin, Dr. Marengi and Dr. Qin report no conflict of interest. Dr. Ladd and C. Marshall MacNabb are employed by Respiratory Motion, Inc.
| References | ▴Top |
- CDC/NCHS National Hospital Discharge Survey. 2010.
- Albu G, Babik B, Kesmarky K, Balazs M, Hantos Z, Petak F. Changes in airway and respiratory tissue mechanics after cardiac surgery. Ann Thorac Surg. 2010;89(4):1218-1226.
doi pubmed - Joskowiak D, Wilbring M, Szlapka M, Georgi C, Kappert U, Matschke K, Tugtekin SM. Readmission to the intensive care unit after cardiac surgery: a single-center experience with 7105 patients. J Cardiovasc Surg (Torino). 2012;53(5):671-676.
- Taenzer AH, Pyke JB, McGrath SP, Blike GT. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010;112(2):282-287.
doi pubmed - Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006;81(3):880-885.
doi pubmed - Wiklund L, Hok B, Stahl K, Jordeby-Jonsson A. Postanesthesia monitoring revisited: frequency of true and false alarms from different monitoring devices. J Clin Anesth. 1994;6(3):182-188.
doi - van Loon K, van Rheineck Leyssius AT, van Zaane B, Denteneer M, Kalkman CJ. Capnography during deep sedation with propofol by nonanesthesiologists: a randomized controlled trial. Anesth Analg. 2014;119(1):49-55.
doi pubmed - Practice guidelines for postanesthetic care: a report by the American Society of Anesthesiologists Task Force on Postanesthetic Care. Anesthesiology. 2002;96(3):742-752.
doi - Gaucher A, Frasca D, Mimoz O, Debaene B. Accuracy of respiratory rate monitoring by capnometry using the Capnomask(R) in extubated patients receiving supplemental oxygen after surgery. Br J Anaesth. 2012;108(2):316-320.
doi pubmed - Panaysuk A, Lalli M, Yocum N, Panasyuk S, Lew R, Logan G, Freeman J. Assessment of a Continuous Monitoring Technique to Measure Adequacy of Respiration. Circulation. 2011;124:A11398.
- Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011;365(2):139-146.
doi pubmed - Taenzer AH, Pyke JB, McGrath SP. A review of current and emerging approaches to address failure-to-rescue. Anesthesiology. 2011;115(2):421-431.
doi pubmed - Lynn LA, Curry JP. Patterns of unexpected in-hospital deaths: a root cause analysis. Patient Saf Surg. 2011;5(1):3.
doi pubmed - Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008;188(11):657-659.
pubmed - Leuvan CH, Mitchell I. Missed opportunities? An observational study of vital sign measurements. Crit Care Resusc. 2008;10(2):111-115.
pubmed - Fouzas S, Politis P, Skylogianni E, Syriopoulou T, Priftis KN, Chatzimichael A, Anthracopoulos MB. Knowledge on pulse oximetry among pediatric health care professionals: a multicenter survey. Pediatrics. 2010;126(3):e657-662.
doi pubmed - Jubran A. Pulse oximetry. Crit Care. 1999;3(2):R11-R17.
doi pubmed - Martinez A, Seymour C, Nam M. Minute ventilation recovery time: a predictor of extubation outcome. Chest. 2003;123(4):1214-1221.
doi pubmed - American Society of Anesthesiologists. Committee for Standards and Practice Parameters: standards for basic anesthetic monitoring. October 10, 2010; effective data. July 1, 2011.
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


