| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Case Report
Volume 5, Number 1, February 2013, pages 64-66
Lung Abscess in a Patient With VAP: A Rare Case of Lung Infection Complicated by Two Pathogens
Christina Mystakellia, Stavros Gourgiotisa, b, Paraskevi Aravositaa, Charalampos Seretisa, Efthymia Kannaa, Stavros Aloizosa
aIntensive Care Unit, “Mitera” Obstetric and Gynecological Hospital, Athens, Greece
bCorresponding author: Stavros Gourgiotis, 41 Zakinthinou Street, 15669, Papagou, Athens, Greece
Manuscript accepted for publication September 14, 2012
Short title: Lung Abscess
doi: https://doi.org/10.4021/jocmr1132w
| Abstract | ▴Top |
Ventilator-associated pneumonia (VAP) is defined as pneumonia occurring in a patient after intubation with an endotracheal tube or tracheostomy tube lasting for 48 hours or more. We describe a case of 75-year-old male who initially presented with pneumonia of the right basis with accompanying plevritis. The patient was intubated and his condition was complicated with a VAP infection while he developed a lung abscess. The antibiotic therapy was based on susceptibility bronchial secretions isolated acinetobacter baumannii and klebsiella pneumoniae; these pathogens were also isolated from the drained abscess. The patient was discharged in good health. The interest of this case is recommended in the existence of two responsible pathogens, the paucity of the development of lung abscess in a patient with VAP, and the successful treatment of the patient with the combination of controlled drainage of the abscess and appropriate antibiotic therapy.
Keywords: Ventilator-associated pneumonia; Acinetobacter baumannii; Klebsiella pneumoniae; Lung; Abscess
| Introduction | ▴Top |
Ventilator-associated pneumonia (VAP) is a common, possibly life-threatening complication in intensive care unit (ICU) patients with a reported relative risk of 9-27% and mortality of 25-50% [1].
The pathogenesis of VAP is supported to initiate from the aspiration of oropharyngeal secretions past the endotracheal tube cuff or from inoculation directly into the airway, resulting finally in the development of severe inflammation of the respiratory system [2].
VAP should be distinguished from the community-acquired pneumonia, which is related to acute respiratory failure, and from nosocomial pneumonia occurring among hospitalized patients, who, on the contrary, do not receive mechanical ventilation. According to CDC guidelines, the diagnosis of VAP in a patient receiving ventilation support are the presence of new and/or progressive pulmonary infiltrates on a chest radiograph plus two or more of the following criteria: fever (≥ 38.5 °C) or hypothermia (< 36 °C), leukocytosis (≥ 12 × 109/L), purulent tracheobronchial secretions, or a reduction in PaO2/FIO2 of at least 15% in the previous 48 hours [3].
We present an extremely rare case of a patient with VAP who developed lung abscess, due to acinetobacter baumanii infection and who was treated with administration of mereponem and colistin combined with computed tomography (CT)-guided drainage. The presence of two main pathogens, the rarity of the development of a lung abscess in a patient with VAP, and the successful management with the combination of CT-guided drainage and cultures-based antibiotic therapy underline the diagnostic and educational value of this case.
| Case Report | ▴Top |
A 75-year-old male with a history of diabetes, heart failure and chronic obstructive pulmonary disease was admitted to hospital with a 2 days history of cough, fever (> 38 °C) and shortness of breath. Chest x-ray and chest CT revealed pneumonia of the right basis (Fig. 1). Under the diagnosis of community-acquired pneumonia, the administration of piperacillin-tazobactam (i.v. and nebulizer) was initially started. Nevertheless, the patient was intubated a few hours later due to hemodynamic instability and insufficient gas exchange. The antibiotic therapy was continued with no patient’s clinical improvement. Acinetobacter baumannii and klebsiella pneumoniae were isolated from the bronchial secretions and a new antibiotic i.v. scheme included meropenem and colistin was administrated; the scheme was based on his bronchial cultures susceptibility while the diagnosis of VAP was established.
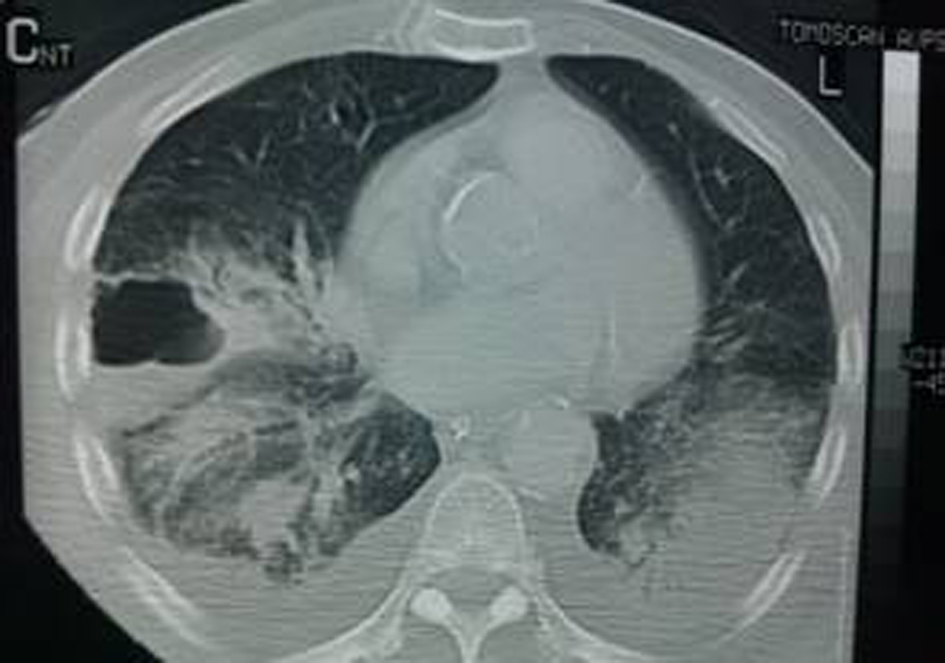 Click for large image | Figure 1. Chest X-ray (a) and CT (b) reveal pneumonia of the right basis with accompanying plevritis. |
| Discussion | ▴Top |
VAP is considered to have become a life-threatening situation in ICU patients. The main reasons are the increased resistance of nosocomeal pathogens in antibiotics administration and the impaired immune response of the critically ill patients.
The most common pathogens that are related to the development of VAP are pseudomonas aeruginosa (about 24%), staphylococcus aureus (about 20%), haemophilus species (about 10%), acinetobacter species (about 8%), streptococcus pneumoniae (about 4%) and klebsiella species (about 2%) [4]. The therapeutic approach of VAP remains a matter of debate; nevertheless, in the daily practice, the main targets are to prevent or confront the migration of the pathogens to the lower respiratory structures and eradicate the developing respiratory infection with the use of appropriate antibiotics. From this point of view, it is evident that the detection of the specific pathogen(s) that cause(s) VAP has a crucial role concerning the type of antibiotics that should be administered, both in order to confront the infection and not violate the principles of evidence-based use of antibiotics.
The most important factors towards this direction are the thorough clinical examination and the close monitoring of the patients, the avoidance of using antibiotics without evidence from antibiogrammes and the capability of multidisciplinary approach of the patients in complicated cases.
In the case presented, VAP was complicated by the formation of a lung abscess, induced by acinetobacter baumanii co-infection. The development of lung abscesses in VAP are rare complications, particularly coming to the presence of acinetobacter baumanii, with almost complete lack of similar case reports, whose rarity could be attributed to the extensive use of broad-spectrum antibiotics in these patients [5].
The therapeutical approach was very challenging. The antibiotics administrated, meropenem and colistin, were proven to be an efficient treatment strategy, managing to intercept the progress of a severe respiratory infection in a critically ill patient, in accordance to the literature [5, 6]. In addition, CT-guided drainage of the lung abscess, which followed in sequence, appeared to be an effective method to treat a lung abscess that was refractory to conventional therapy.
In conclusion, the successful management of this severe infection, along with its rare complication by the particular species, lied upon the combination of aggressive -but not excessive- antibiotics treatment in combination with interventional radiology applications, underlining the significance of multidisciplinary approach in rising up to the task of coping with complex and life-threatening infections in the ICU environment.
| References | ▴Top |
- Torres A, Ewig S, Lode H, Carlet J. Defining, treating and preventing hospital acquired pneumonia: European perspective. Intensive Care Med. 2009;35(1):9-29.
pubmed - Safdar N, Crnich CJ, Maki DG. The pathogenesis of ventilator-associated pneumonia: its relevance to developing effective strategies for prevention. Respir Care. 2005;50(6):725-739, discussion 739-741.
pubmed - Rosenthal VD, Bijie H, Maki DG, Mehta Y, Apisarnthanarak A, Medeiros EA, Leblebicioglu H,
et al . International Nosocomial Infection Control Consortium (INICC) report, data summary of 36 countries, for 2004-2009. Am J Infect Control. 2012;40(5):396-407.
pubmed - Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165(7):867-903.
pubmed - Mukhopadhyay C, Krishna S, Vandana KE, Shenoy A, Bairy I. Ventilator-associated pneumonia with Col-S strains: a successful comeback of colistin!. Braz J Infect Dis. 2008;12(5):444-446.
pubmed - Pachon-Ibanez ME, Docobo-Perez F, Lopez-Rojas R, Dominguez-Herrera J, Jimenez-Mejias ME, Garcia-Curiel A, Pichardo C,
et al . Efficacy of rifampin and its combinations with imipenem, sulbactam, and colistin in experimental models of infection caused by imipenem-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54(3):1165-1172.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


