| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 4, Number 5, October 2012, pages 338-345
Emergency Department Pneumonia Patients Who do not Meet the Six-Hour Criteria for Antibiotic Administration: Do They Have a Different Clinical Presentation?
Susan H. Wattsa, b, E. David Bryana
aTexas Tech University Health Sciences Center, Paul L Foster School of Medicine, Department of Emergency Medicine, USA
bCorresponding author: Susan H.Watts, TTUHSC Dept of Emergency Medicine, 4800 Alberta Ave, El Paso TX, 79905, USA
Manuscript accepted for publication August 14, 2012
Short title: ED Pneumonia Patients
doi: https://doi.org/10.4021/jocmr1092w
| Abstract | ▴Top |
Background: The Joint Commission (JC) has set a quality of care standard for emergency department (ED) patients diagnosed with community acquired pneumonia (CAP) that states that they are to receive antibiotics within six hours of presentation to the ED. Hospitals have been able to demonstrate that the majority of patients meet these criteria, yet there are still many who do not. Previously published studies have reported that there are several issues that contribute to prolonged times to antibiotic administration including ED crowding and atypical clinical presentations. This study was undertaken to identify factors existing early in the patient encounter that may be associated with failure to meet the Joint Commission’s six-hour standard for antibiotic administration.
Methods: This was an IRB-approved, retrospective observational study covering 36 months in an academic emergency department. All adults with an admission diagnosis of CAP were eligible but were excluded if their discharge diagnosis was not CAP, if hospitalized within the previous 14 days, or if HIV positive. Univariate analysis and multiple logistic regression with stepwise variable selection were performed comparing patients who met and did not meet JC standards. The analysis included demographics (age, sex), chief complaint at triage and to doctor (fever, dyspnea, cough, chest pain, weakness/fatigue, abdominal pain), presence of altered mental status, triage vital signs, co-morbidities, day of week and time of day of presentation.
Results: A total of 736 cases were eligible; 199 cases met exclusion criteria; 43 charts were unavailable; 494 were included in the study group (363 with complete antibiotic time records; 131 were incomplete). From the univariate analysis, respiratory rate (RR) and oxygen saturation were the only factors that met Bonferroni criteria for statistical significance when comparing those who met and did not meet the JC six-hour criteria (RR 25 ± 9 vs 22 ± 6 breaths/minute, respectively, P = 0.002; oxygen saturation 87 ± 10% vs 92 ± 5%, respectively, P < 0.001). Multiple logistic regression identified triage pulse rate, oxygen saturation, presence of altered mental status, hour of day, and day of week as variables associated with time to antibiotic administration. Chances for meeting the standard were increased by 10% for each 5-beat increase in pulse rate or 1% decrease in oxygen saturation. If the person exhibited altered mental status, they were > 3.5 times more likely to meet the 6-hour criteria. If they presented to ED between 3 PM and 10 PM chances of meeting criteria were reduced by about 65%. If they presented on a Thursday, chances improved 2.8 times.
Conclusions: Compared to patients who did meet Joint Commission criteria, those who did not receive antibiotics within 6 hours were likely to have triage pulse rates and O2 saturation levels closer to normal, thus contributing to diagnostic uncertainty. They were also likely to present to the ED at the most crowded time of day. Likelihood to meet JC criteria was improved if O2 saturation was below normal, pulse rate was elevated, if they exhibited mental confusion, or if they presented to the ED very early or very late in the day, or on a lower census day.
Keywords: Community acquired pneumonia; CAP; Joint Commission
| Introduction | ▴Top |
The length of time that elapses before patients diagnosed with community acquired pneumonia (CAP) receive antibiotics in the Emergency Department (ED) is thought to have an impact on patient outcome [1, 2]. Consequently, the Infectious Disease Society of America and the American Thoracic Society set time guidelines for the administration of the first dose of antibiotics to patients diagnosed with CAP in the ED [3]. Although there is little evidence to support a specific time recommendation for antibiotic administration, the Joint Commission on Accreditation of Healthcare Organizations (Joint Commission or JC) has instituted quality of care standards (namely core measures) for hospitals that evaluate whether pneumonia patients receive their first dose of antibiotics within six hours of hospital arrival (PN-5c) [3, 4]. This has been modified from an earlier standard (PN-5b) for which the time limit had been set at four hours.
Joint Commission criteria are met for the majority of ED patients diagnosed with CAP, but the treatment of many patients still fails to meet the six-hour standard. Previously published studies have reported that prolonged time to first dose of antibiotics is associated with many issues including atypical clinical presentations [5] and ED crowding [6, 7]. In our own ED, we have observed that the sickest patients appear to be treated in the shortest length of time, namely their clinical presentation is definitive and treatment can be initiated quickly. We hypothesized that those who have prolonged times for antibiotic administration were more likely to have clinical presentations that are more ambiguous, and therefore treatment is delayed.
The objective of this study was to identify factors existing early in the patient encounter that may be associated with the failure to meet the Joint Commission’s six-hour standard for antibiotic administration.
| Methods | ▴Top |
Study design, setting, and population
This retrospective observational study covering a 36-month period (2002 - 2004) was approved by the El Paso IRB of the Texas Tech University Health Sciences Center with waiver of consent. It was conducted in an academic emergency department with about 60,000 patient visits per year.
Study protocol
All adult patients (≥18 years old) with a hospital admission diagnosis of CAP were eligible for inclusion. A list of potentially eligible patients was generated using the ED information system (Logicare Corporation, Eau Claire, WI) employing search terms for all pneumonia types including bacterial, viral, aspiration, and anaerobic pneumonias. This allowed for the inclusion of CAP patients who might have been miscoded due to clerical errors. One of the investigators (SHW) performed the chart reviews and recorded the information on an electronic data abstraction form (Microsoft Access, Microsoft Corporation, Redmond WA). Patient cases were excluded if the final hospital discharge diagnosis was not CAP, if they had been hospitalized within the 14 days prior to this admission, or if they were human immunodeficiency virus (HIV) positive. These criteria reduced the probability of including patients with hospital-acquired or atypical pneumonias and are consistent with previous CAP studies [8, 9].
Data abstracted from the charts included elements necessary to calculate Pneumonia Severity Index (PSI) [10],including demographics (age, sex, nursing home resident); co-morbidities (history of neoplasia, liver disease, congestive heart failure, cerebrovascular disease, or renal disease); triage vital signs (respiratory rate, systolic blood pressure, temperature, pulse, oxygen saturation), presence of mental confusion; worst vital signs (respiratory rate, systolic blood pressure, temperature, pulse, oxygen saturation); and results of some laboratory and imaging studies (arterial pH less than 7.35, PO2 less than 60 mmHg, sodium if less than 130 mEq/L, BUN if greater than 30 mg/dL, glucose if greater than 250 mg/dL, hematocrit if less than 30%, and presence of pleural effusion). In addition we recorded the patient’s chief complaint at triage and to the doctor (fever, dyspnea, cough, chest pain, weakness/fatigue, abdominal pain), times of blood culture orders and draws, times of antibiotic orders and administration, hospital unit admitted to, ED triage date and time, hospital discharge date and time, and final diagnosis. Time to antibiotic administration was calculated as the time between the electronic triage time stamp and time of antibiotic administration recorded in the chart. Presence of mental confusion was considered positive if the patient’s chief complaint or history of present illness included references to altered mental status (AMS), somnolence, or behavior changes. History of dementia or Alzheimer’s disease was not considered positive for mental confusion unless there was a change from their usual condition.
Measurements
We limited our statistical analysis to data that would be available early in the patient encounter, namely before the results of lab and imaging studies would be available for most patients. This decision was based on the assumption that in many EDs there may be a significant delay between triage and physician examination and a further delay when awaiting laboratory and imaging results [11, 12]. Once the decision to give antibiotics has been made, orders must be written and transmitted and the drugs must be obtained and administered. Therefore, we reasoned that if the six-hour criteria are to be met, the decision to give antibiotics is often made soon after the initial patient encounter.
Data analysis
Univariate statistical analysis was performed for each of the risk factors described below using T-tests for continuous variables and Fisher’s exact test for categorical variables (Stata, v.10.1; College Station, TX). Due to the large number of variables (n = 28), Bonferroni criteria were applied, making statistical significance P < or = 0.002 (namely 0.05/28). Multiple logistic regression was performed using stepwise variable selection to compare characteristics of those who met the six-hour standard to those who did not (Stata, v.10.1; College Station, TX). Included in the logistic regression analysis were patient age and sex, presence of mental confusion (Y/N), chief complaint at triage and to doctor, triage vital signs, and co-morbidities. In addition, because previous studies have shown that ED crowding can affect antibiotic administration times [6, 7], we included day of week and time of day. Time of day was categorized as early (7 AM - 2:59 PM), midday (3 PM to 10:59 PM), and night (11 PM to 6:59 AM). Statistical significance was set at P < or = 0.05.
| Results | ▴Top |
A total of 736 cases met the inclusion criteria; 199 cases met exclusion criteria; 43 charts were unavailable, leaving 494 cases as the study group. Among the included cases, 363 cases had complete antibiotic time records while 131 cases had incomplete records (Fig. 1).
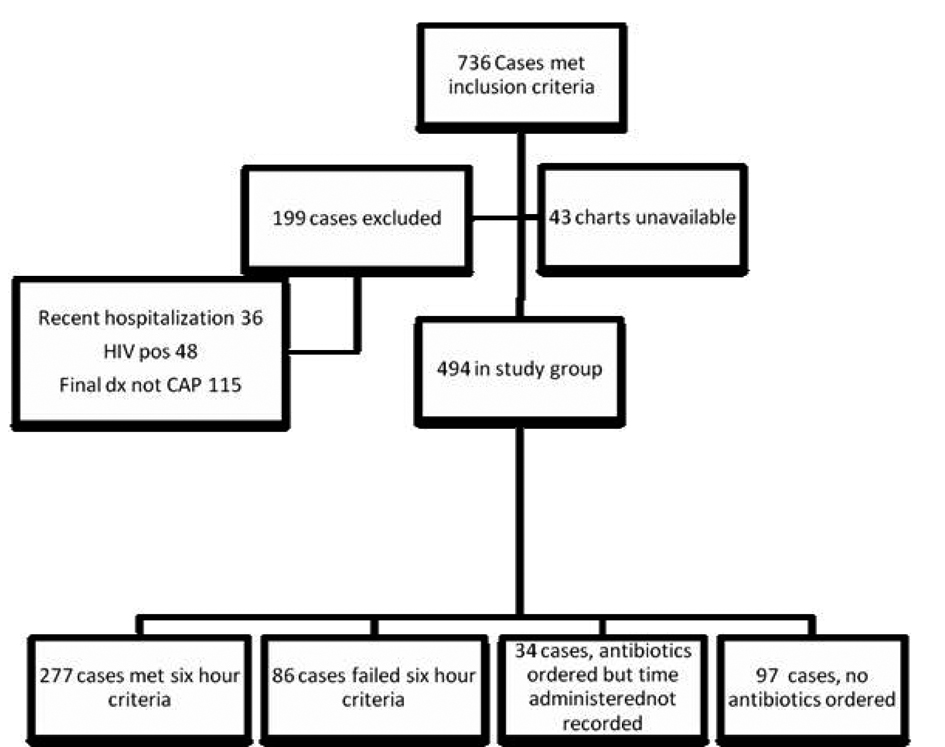 Click for large image | Figure 1. Included and excluded cases. |
From univariate analysis of patients with complete antibiotic data, the only characteristics meeting Bonferroni criteria for statistical significance were respiratory rate and average oxygen saturation (P = 0.002 and P < 0.001, respectively) (Table 1). Mean pulse rate approached statistical significance (P = 0.007) and there were no statistically significant differences for any other vital signs, co-morbidities, chief complaints, day-of-week or hour of day of presentation.
 Click to view | Table 1. Univariate Analysis Comparing Characteristics of Cases That Met and Failed to Meet the Joint Commission Six-Hour Standard for Antibiotic Administration |
Multiple logistic regression identified five variables associated with time to antibiotic administration: triage pulse rate, oxygen saturation, presence of altered mental status, hour of day, and day of week (Table 2). Chances for meeting the six-hour standard were increased if the person exhibited altered mental status, if their oxygen saturation was decreased, or if their pulse rate was elevated. If the person had altered mental status they were > 3.5 times more likely to meet the six-hour criteria. A 1% decrease in O2 saturation and 5 beat increases in pulse rate were each associated with a 10% increase in chances to meet criteria. Patients who presented to the ED between 3 PM and 11 PM were only one-third as likely to meet the JC criteria as those who presented early in the day or late at night. If they presented on a Thursday, they were 2.8 times more likely to meet the six-hour criteria.
 Click to view | Table 2. Results of Multiple Logistic Regression Using Stepwise Variable Selection to Identify Patient Risk Factors Associated With Likelihood to Meet Joint Commission Criteria for Administration of Antibiotics Within Six Hours if Diagnosed With CAP in the ED |
Because 27% of the included cases had incomplete antibiotic data and so were not included in the logistic regression, we compared the characteristics of the complete-data versus incomplete-data groups to rule out the possibility that those with incomplete data might constitute a distinct group. From univariate analysis, the only characteristic meeting Bonferroni criteria for statistical significance was average oxygen saturation which was lower in the complete data group (88 ± 9% vs 91 ± 7%, P = 0.002) (Table 3). Average temperature and pulse rate approached statistic al significance but the differences were not clinically significant (Table 3). A larger percentage of the patients with complete antibiotic data reported a fever to the doctor (44% vs 31%, P = 0.007) (Table 3). Otherwise, the cases with incomplete antibiotic data appear to be similar to those included in the logistic regression analysis.
 Click to view | Table 3. Characteristics of Cases Included in Multiple Logistic Regression Compared to Cases not Included due to Incomplete Antibiotic Data |
| Discussion | ▴Top |
Our results indicate that triage pulse rate, triage oxygen saturation level, presence of altered mental status, hour of day and day of week of presentation are each associated with the likelihood of receiving antibiotics within 6 hours of presentation for patients diagnosed with CAP in our ED. Patients who demonstrated altered mental status, lower oxygen saturation or an increased heart rate early in their patient encounter are more likely to receive antibiotics within six hours than those with vital signs closer to normal. Patients who present during the late afternoon and evening (3 - 11 PM) have reduced chances of meeting the six-hour criteria while those who present on Thursdays have increased chances.
It stands to reason that patients with elevated pulse rates, reduced oxygen saturation, and altered mental status are more likely to meet the six-hour standard because there is little doubt that they are sick and the decision to give antibiotics does not necessarily require laboratory or imaging tests. Our results are in agreement with previously published studies that have also identified associations between ‘markers of severe illness’ and increased odds of meeting antibiotic administration guidelines, including reduced oxygen saturation [7, 13, 14], elevated pulse rate [7, 14], elevated respiratory rate [7, 14], and fever [14]. There is disagreement however on the role of altered mental status. The results of the present study appear to group altered mental status with other signs of sepsis thereby contributing to reduced time to antibiotic administration. This conflicts with the findings of Waterer et al who found that altered mental status was associated with delays in antibiotic administration [5]. This incongruity is likely to be due to the somewhat different definitions of altered mental status in the two studies and the differences in inclusion criteria for the two studies (patients with clinical evidence of pneumonia vs patients with ED diagnosis of pneumonia).
In the absence of obvious signs of pneumonia such as fever and hypoxia, the time to antibiotic administration trends toward times in excess of four hours [5, 15]. When diagnostic uncertainty arises, such as when patients with CAP lack rales or hypoxia, laboratory and imaging studies must be completed before a definitive diagnosis can be made. Up to 22% of Medicare patients in one study presented in a manner likely to result in delayed diagnosis of CAP [15].
ED crowding has been shown to negatively impact the timely administration of antibiotics to CAP patients [6, 7]. In the present study, the association between time of day of presentation and time to antibiotic administration is likely due to ED crowding because peak ED patient census generally occurs between 3 PM and 11 PM in our facility. Significant factors influencing ED crowding are the number of people in the waiting room and the average length of stay for admitted paitents [7]. In our facility, the number of people in the waiting room increases steadily from about 10 AM and the number of available ED beds decreases as admitted patients wait to be moved to the floor. Although these previous studies examined compliance with the older 4-hr standard, we believe the general trends regarding the effects of ED crowding and timing of antibiotic administration are applicable to the current study. The association of Thursdays with reduced time to antibiotic administration is also likely to be due ED crowding as Thursdays are generally our lowest census days.
Limitations
This study relied on retrospective chart review for data and consequently was limited solely to what was recorded. For this study, if the time for drug administration was not recorded, we assumed it was not given. In addition, it was conducted at a single institution which is a county hospital and the results of the study may or may not be generalizable to different hospital settings. Similarly, our patient population may be unusual in that few have third party insurance and a significant proportion has limited access to primary care. Consequently many of our patients present to the ED in advanced stages of illness and require hospital admission. This could increase the proportion of patients seen who have abnormal vital signs.
It is concerning that the final analysis of data for this study included just 45% of the cases that met inclusion criteria, but this is not out of line with previously published papers. In this realm of investigation, the inclusion criteria are often very broad and then the exclusion criteria are applied to pare down the number of cases that apply to the question of interest. It is not unusual to find that the study population remaining after the application of all exclusion criteria can range from 46 to 64% of the original number of included cases [1, 2, 6, 12, 16].
Conclusions
Compared to patients who were given antibiotics within six hours of presentation, those who have prolonged times for antibiotic administration are likely to have pulse rates and oxygen saturation levels at presentation that are closer to normal, thus contributing to diagnostic uncertainty for CAP. They are also likely to present to the ED during the time of day when it is most crowded. The likelihood to meet JC criteria was improved if a patient’s oxygen saturation was below normal, if pulse rate was elevated, if mental confusion was evident, or if ED presentation was very early or very late the day, or on a lower census day.
Acknowledgments
Many thanks to Adir Doliner, MD who assisted with chart review, Stephen Borron MD who provided very insightful manuscript review, and Patrick Tarwater PhD and Melchor Ortiz PhD who provided guidance in statistical analysis and interpretation.
Declaration
Presented at the Western Regional SAEM meeting, February 2011, Keystone CO; Paul L Foster School of Medicine Research Colloquium, May 2011, El Paso TX; SAEM Annual Meeting, June 2011, Boston MA.
Financial Support
There was no financial support for the investigation or manuscript development other than regular salary.
Conflict of Interest
Neither author has any financial arrangement or conflict of interest to disclose.
| References | ▴Top |
- Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med. 2004;164(6):637-644.
pubmed - Meehan TP, Fine MJ, Krumholz HM, Scinto JD, Galusha DH, Mockalis JT, Weber GF,
et al . Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA. 1997;278(23):2080-2084.
pubmed - Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF,
et al . Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27-72.
pubmed - Specifications Manual for National Hospital Inpatient Quality Measures: Centers for Medicare & Medicaid Services and the Joint Commission. http://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx.
- Waterer GW, Kessler LA, Wunderink RG. Delayed administration of antibiotics and atypical presentation in community-acquired pneumonia. Chest. 2006;130(1):11-15.
pubmed - Fee C, Weber EJ, Maak CA, Bacchetti P. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):501-509.
pubmed - Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, Metlay JP. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007;50(5):510-516.
pubmed - Ramanujam P, Rathlev NK. Blood cultures do not change management in hospitalized patients with community-acquired pneumonia. Acad Emerg Med. 2006;13(7):740-745.
pubmed - Benenson RS, Kepner AM, Pyle DN, 2nd, Cavanaugh S. Selective use of blood cultures in emergency department pneumonia patients. J Emerg Med. 2007;33(1):1-8.
pubmed - Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, Coley CM,
et al . A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243-250.
pubmed - Rodriguez KL, Burkitt KH, Sevick MA, Obrosky DS, Aspinall SL, Switzer G, Mor MK,
et al . Assessing processes of care to promote timely initiation of antibiotic therapy for emergency department patients hospitalized for pneumonia. Jt Comm J Qual Patient Saf. 2009;35(10):509-518.
pubmed - Fee C, Weber EJ. Identification of 90% of patients ultimately diagnosed with community-acquired pneumonia within four hours of emergency department arrival may not be feasible. Ann Emerg Med. 2007;49(5):553-559.
pubmed - Schouten JA, Hulscher ME, Kullberg BJ, Cox A, Gyssens IC, van der Meer JW, Grol RP. Understanding variation in quality of antibiotic use for community-acquired pneumonia: effect of patient, professional and hospital factors. J Antimicrob Chemother. 2005;56(3):575-582.
pubmed - Fee C, Metlay JP, Camargo CA, Jr., Maselli JH, Gonzales R. ED antibiotic use for acute respiratory illnesses since pneumonia performance measure inception. Am J Emerg Med. 2010;28(1):23-31.
pubmed - Metersky ML, Sweeney TA, Getzow MB, Siddiqui F, Nsa W, Bratzler DW. Antibiotic timing and diagnostic uncertainty in Medicare patients with pneumonia: is it reasonable to expect all patients to receive antibiotics within 4 hours? Chest. 2006;130(1):16-21.
pubmed - Caterino JM, Hiestand BC, Martin DR. Quality of care in elder emergency department patients with pneumonia: a prospective cohort study. BMC Emerg Med. 2008;8:6.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.


