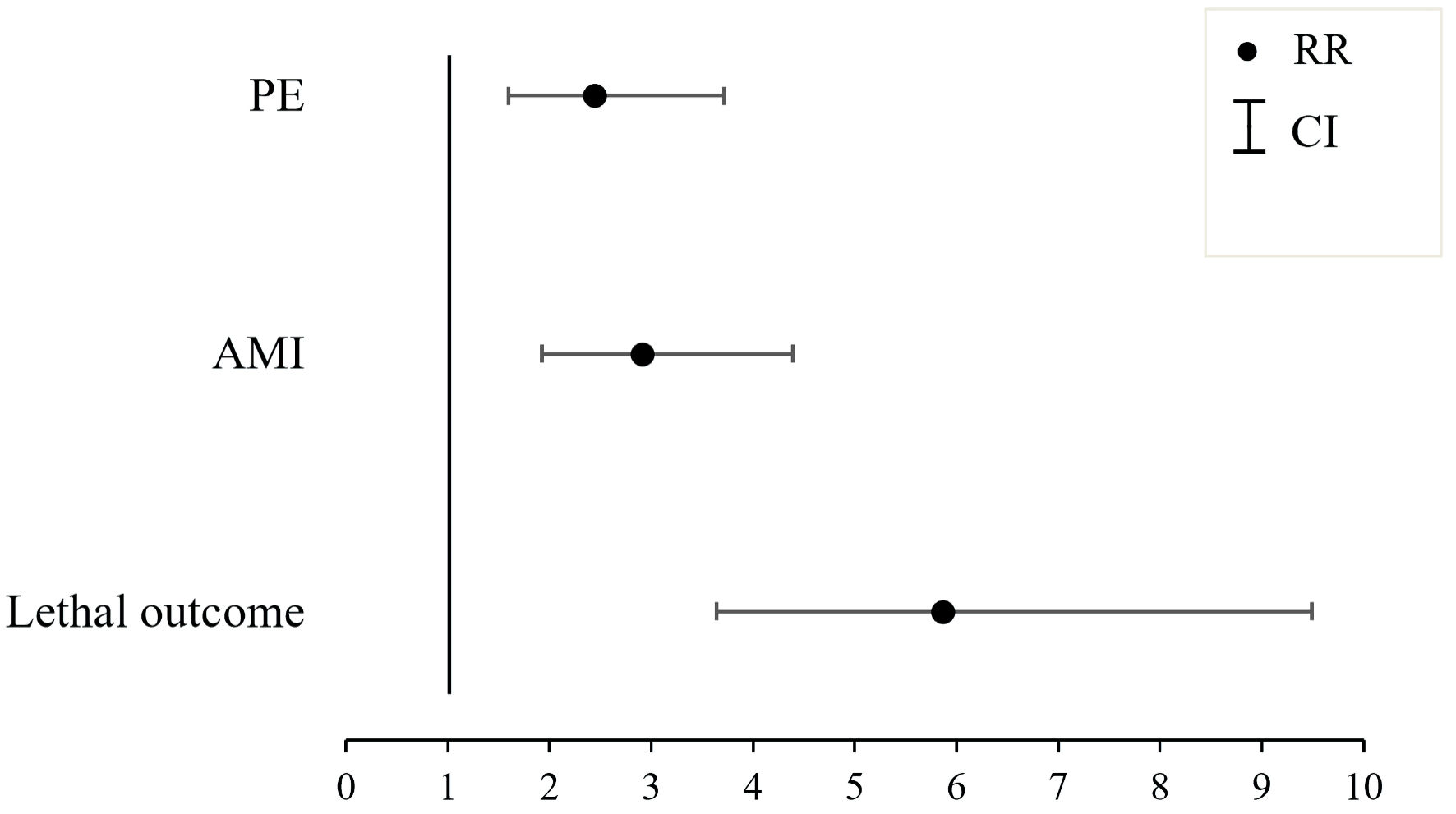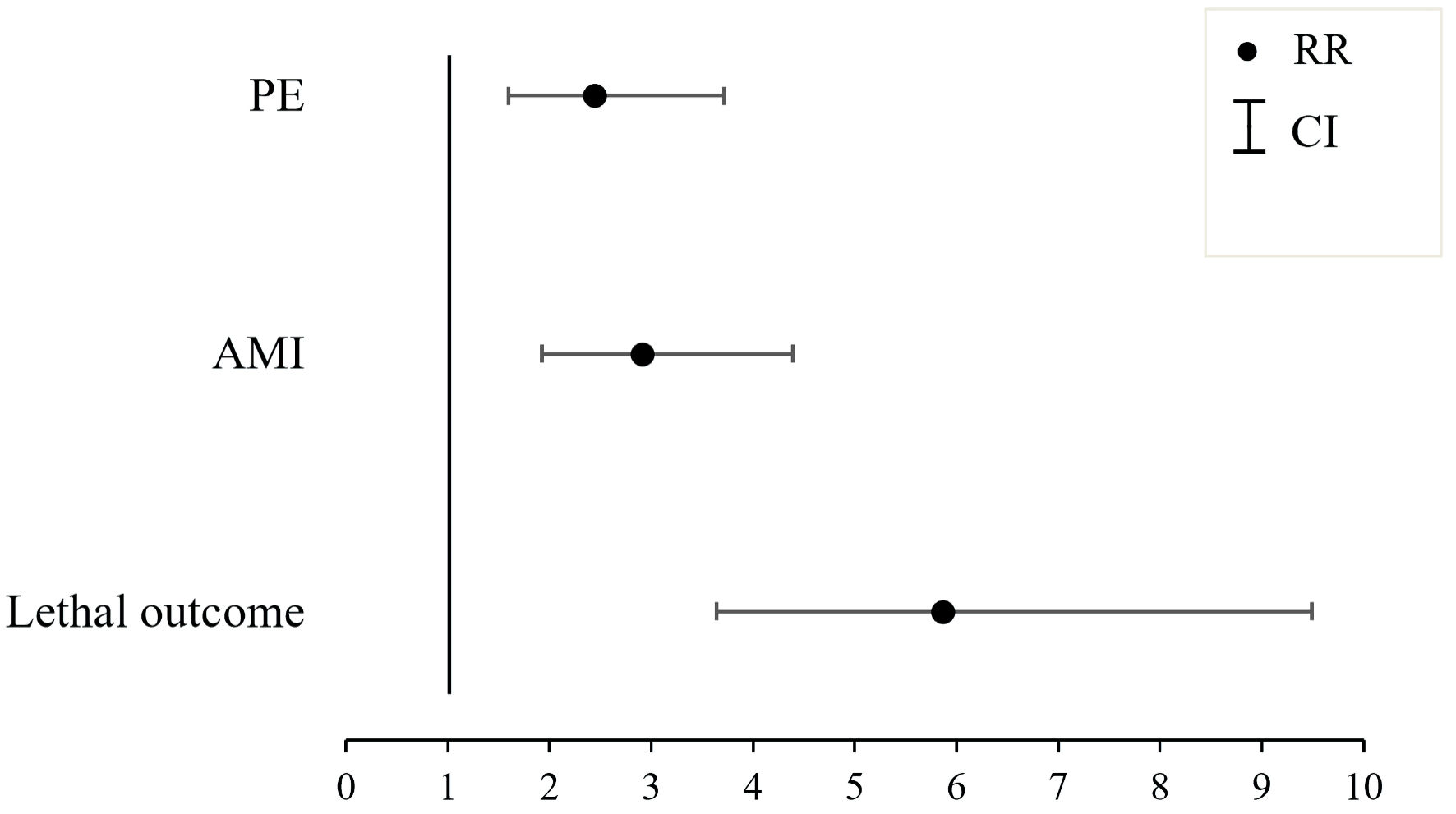
Figure 1. The influence of the presence of premature ventricular contractions (PVCs) on the onset of cardiovascular complications within the studied cohort. AMI: acute myocardial infarction, PE: pulmonary embolism; RR: risk ratio; CI: confidence interval.
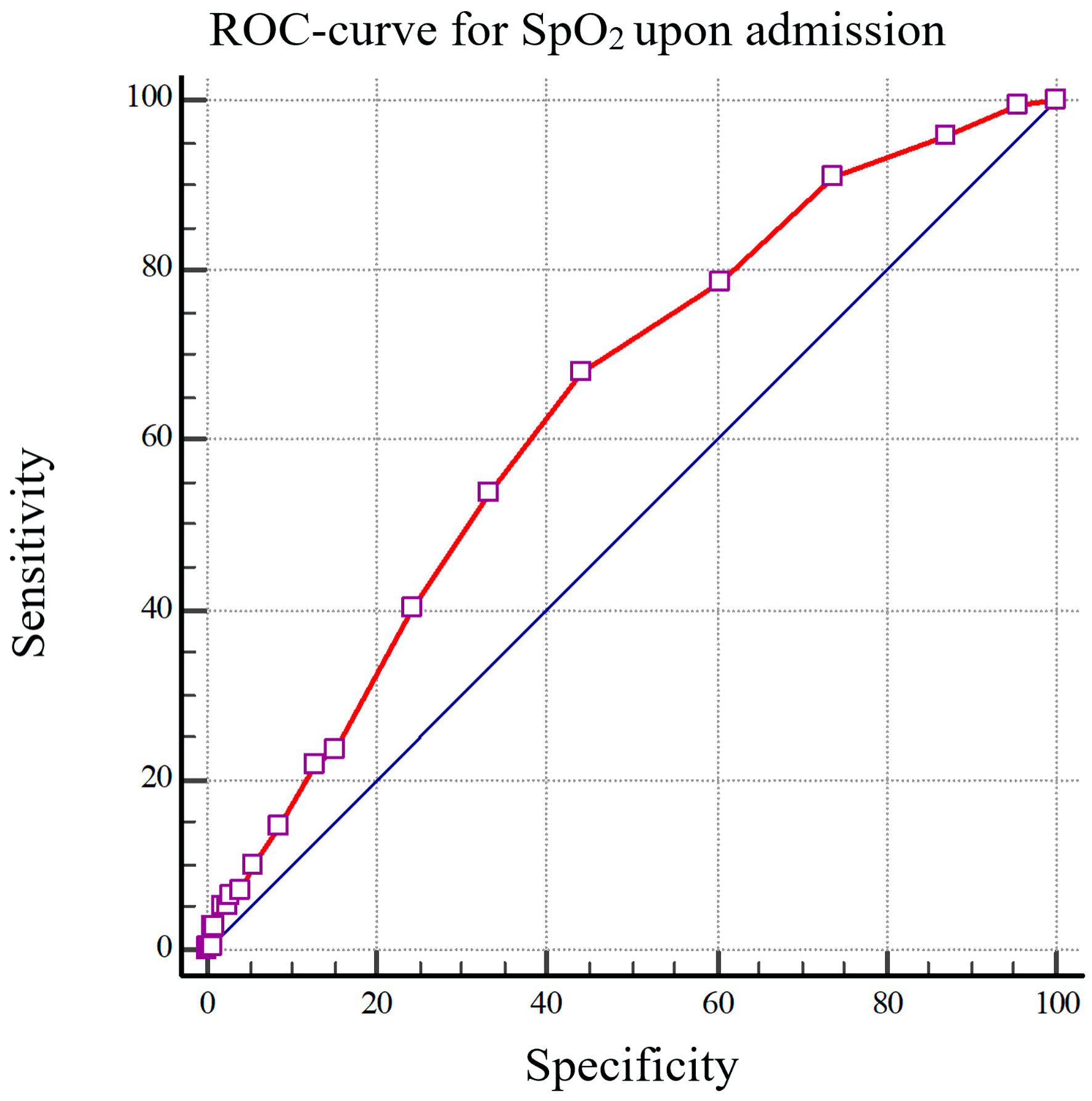
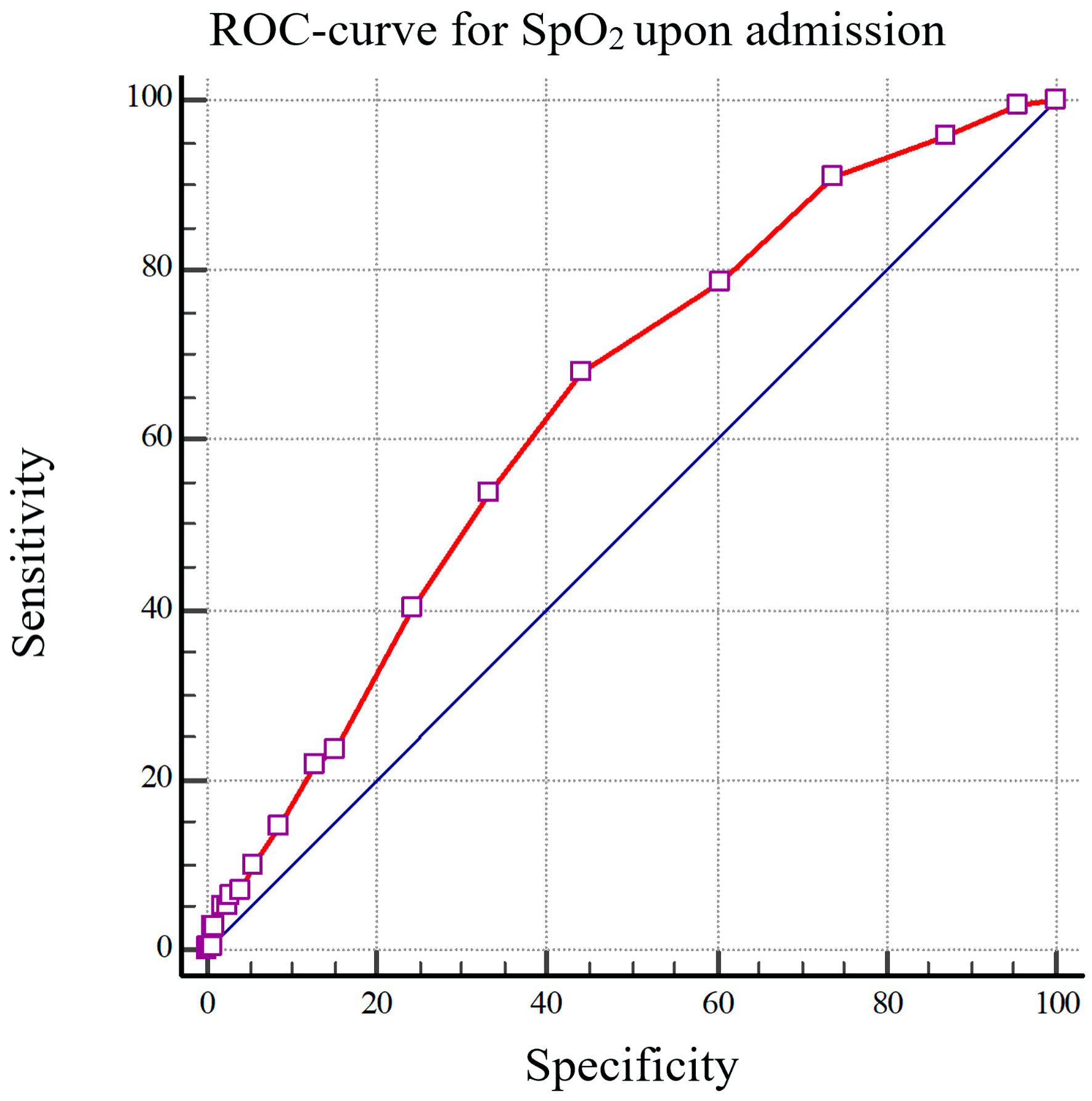
Figure 2. The ROC curve depicting the reduction in peripheral capillary oxygen saturation (SpO2) upon admission, specifically less than 95%, as a predictive measure for the onset of premature ventricular contractions (PVCs) in individuals afflicted with COVID-19 (AUC: 0.641). SpO2: the average value of oxygen saturation measured by a pulse oximeter; ROC: receiver operating characteristic; COVID-19: coronavirus disease 2019; AUC: area under the curve.