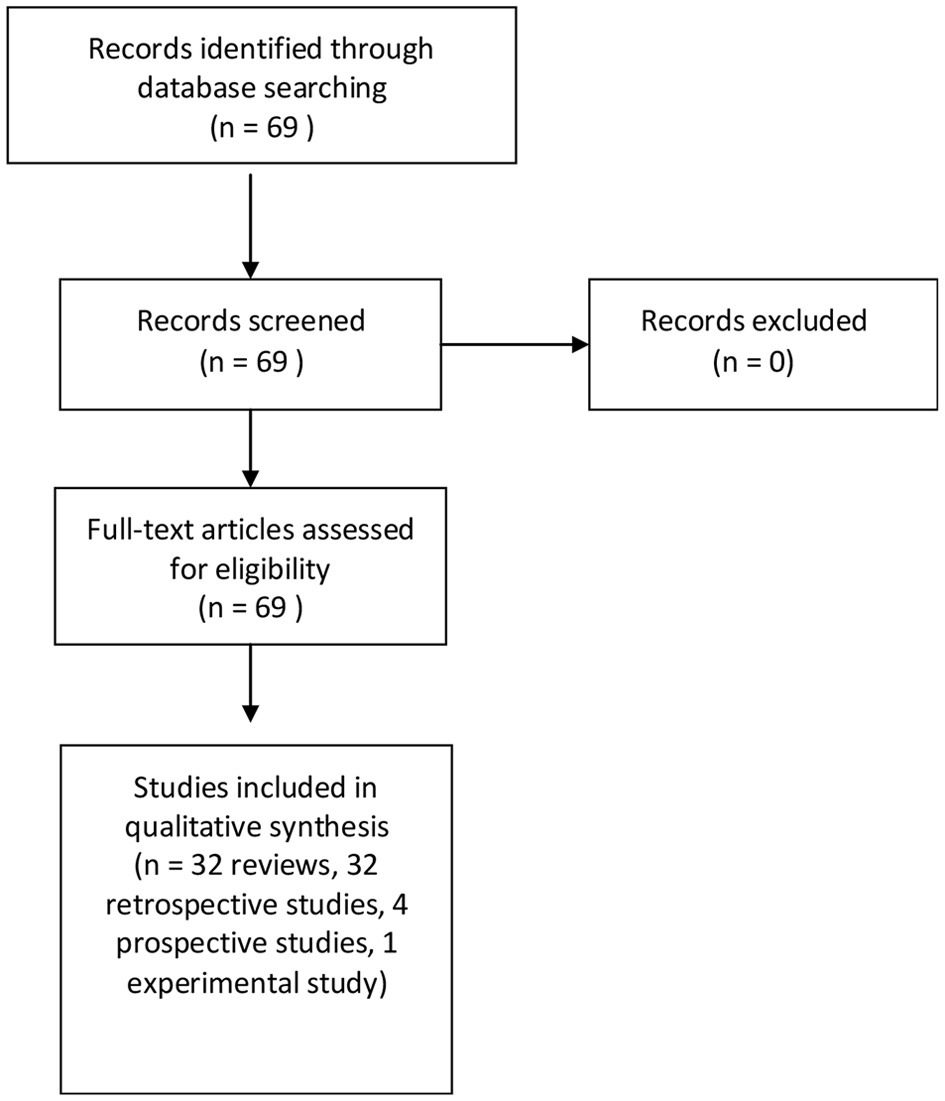
Figure 1. Diagram of the search strategy.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 14, Number 4, April 2022, pages 147-157
State of the Art, Current Perspectives, and Controversies of Budd-Chiari Syndrome: A Review
Figures
Tables
| Type | Level of obstruction |
|---|---|
| Reprinted with permission from Reference 3. BCS: Budd-Chiari syndrome; IVC: inferior vena cava. | |
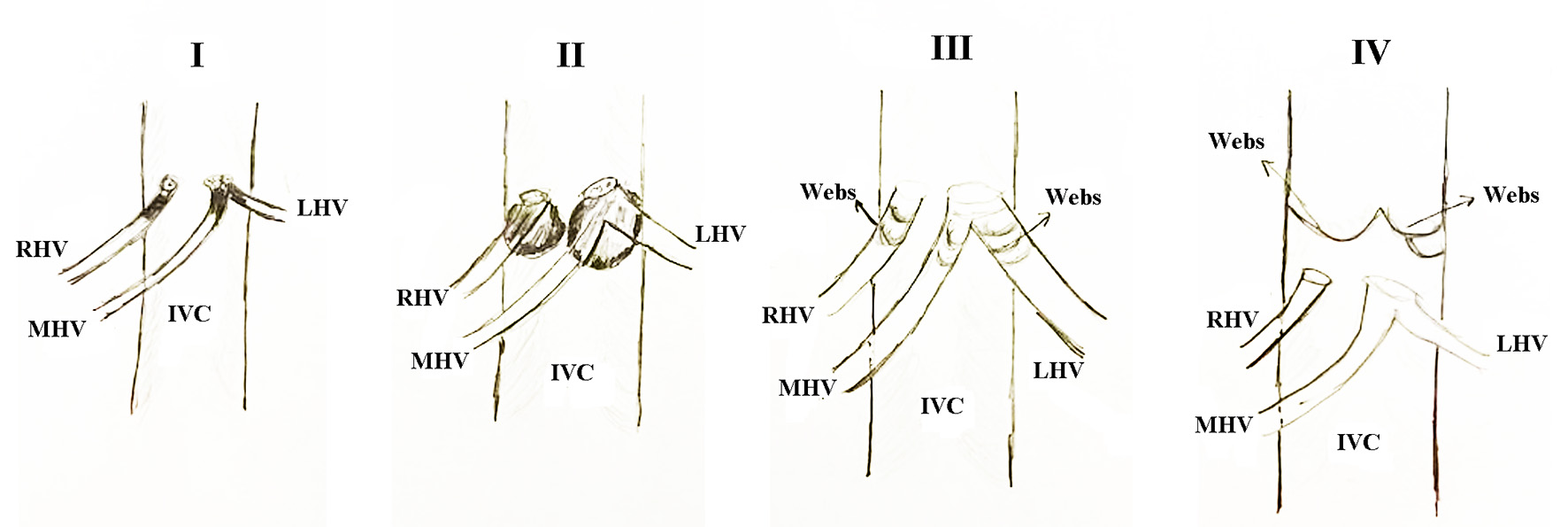
| I | Obstruction of IVC with or without secondary hepatic vein occlusion |
| II | Obstruction of major hepatic veins |
| III | Obstruction of the small centrilobular venules (considered by some as veno-occlusive disease) |
| Type | Level of obstruction |
|---|---|
| Reprinted with permission from Reference 3. BCS: Budd-Chiari syndrome; IVC: inferior vena cava. | |
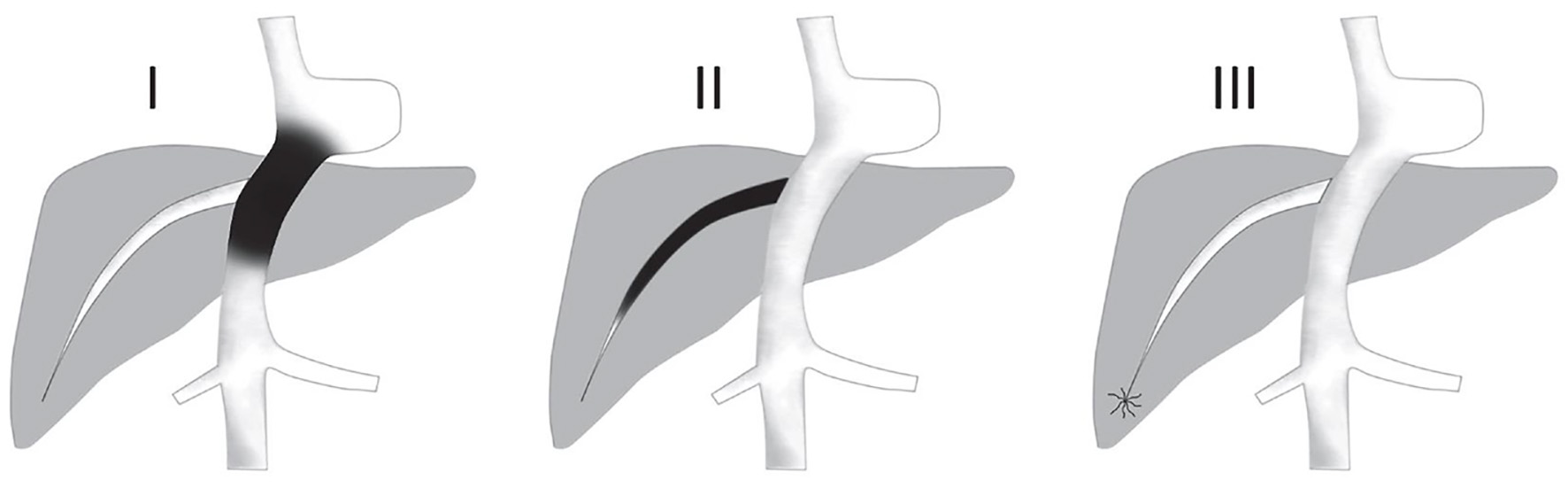
| I | Hepatic vein obstruction or thrombosis without IVC obstruction or compression |
| II | Hepatic vein obstruction or thrombosis with IVC obstruction or thrombosis |
| III | Isolated hepatic venous webs |
| IV | Isolated IVC webs |
| Type | Duration of disease |
|---|---|
| Reprinted with permission from Reference 3. BCS: Budd-Chiari syndrome. | |
| Fulminant | Present with hepatic encephalopathy within 8 weeks of development of jaundice |
| Acute | Short duration (< 1 month), ascites, hepatic necrosis without formation of venous collaterals |
| Subacute | Insidious onset (1 - 6 months), ascites, minimal hepatic necrosis, and portal and hepatic venous collaterals |
| Chronic | (> 6 months) Complications of cirrhosis in addition to findings in the subacute form |
| Type | Pathology | Management |
|---|---|---|
| Reprinted with permission from Reference 11. ACLF: acute-on-chronic liver failure; BCS: Budd-Chiari syndrome; HV: hepatic vein; TIPSS: transjugular intrahepatic portosystemic shunt. | ||
| A | Acute hepatic vein thrombosis or stent block precipitates ACLF in a BCS | Urgent recanalization as per anatomy operations: 1. Thrombectomy or thrombosis with stenting; 2. HV stenting; 3. TIPSS |
| B | Non-thrombotic acute insult precipitates ACLF in a chronic BCS | B1: BCS treated successfully previously, treat like any other ACLF B2: BCS untreated previously: 1. Treatment of BCS after recovery from acute insult; 2. Liver transplant |
| C | Acute hepatic vein thrombosis precipitates ACLF in a non-vascular chronic liver disease | Operations: 1. Thrombectomy or thrombosis with stenting; 2. HV stenting; 3. Liver transplant |
| Prognostic index | Parameters | Formula | Interpretation |
|---|---|---|---|
| Reprinted with permission from Reference 11. AIIMS-HVOTO: All India Institute of Medical Sciences Hepatic Venous Outflow Tract Obstruction; BCS: Budd-Chiari syndrome; INR: international normalized ratio; OLT: orthotopic liver transplantation; TIPSS: transjugular intrahepatic portosystemic shunt. | |||
| Clichy | Ascites, Child-Pugh score, age, creatinine | (Ascites score × 0.75) + (Pugh score × 0.28) + (Age × 0.037) + (Creatinine × 0.0036) | 5-year survival < 5.4: 95% > 5.4: 62% |
| New Clichy score | Ascites, Child-Pugh score, age, creatinine, pathological form (acute, chronic, or both) | 0.95 × Ascites score + 0.35 × Pugh score + 0.047 × Age + 0.0045 × Serum creatinine + (2.2 × form III) | 5-year survival < 5.1: 100% > 5.4: 65% |
| Rotterdam score | Encephalopathy, ascites, prothrombin time, bilirubin | (1.27 × Encephalopathy) + (1.04 × Ascites) + (0.72 × Prothrombin time) + (0.004 × Bilirubin) | 5-year survival Class I (0 - 1.1): 89% Class II (1.1 - 1.5): 74% Class III (> 1.5): 42% |
| BCS-TIPSS score | Bilirubin, age, INR | Age (years) × 0.08 + Bilirubin (mg/dL) × 0.16 + INR × 0.63 | 1-year OLT-free survival < 7: 95% > 7: 12% |
| AIIMS-HOVTO score | Response to therapy and Child-Pugh score | 1.2 × Response to therapy + 0.8 × Child class | 5-year survival < 3: 92% 3.1 - 4: 79% > 4: 39% |
| Category | Residual stenosis | PG | Ascites | Liver function tests |
|---|---|---|---|---|
| Reprinted with permission from Reference 63. BCS: Budd-Chiari syndrome; PG: pressure gradient. | ||||
| Excellent | 0 - 25 | Hemodynamically comparable reduction of PG | Complete reduction (if present) | Improved |
| Good | 25 - 30 | Comparable residual PG | Stable (not requiring paracentesis or diuretics) | Stable |
| Fair | 30 - 50 | Improved PG | Controlled with paracentesis or diuretics | Mildly deteriorated |
| Poor | > 50 | Minimal or no improvement | Increasing | Cross derangement |