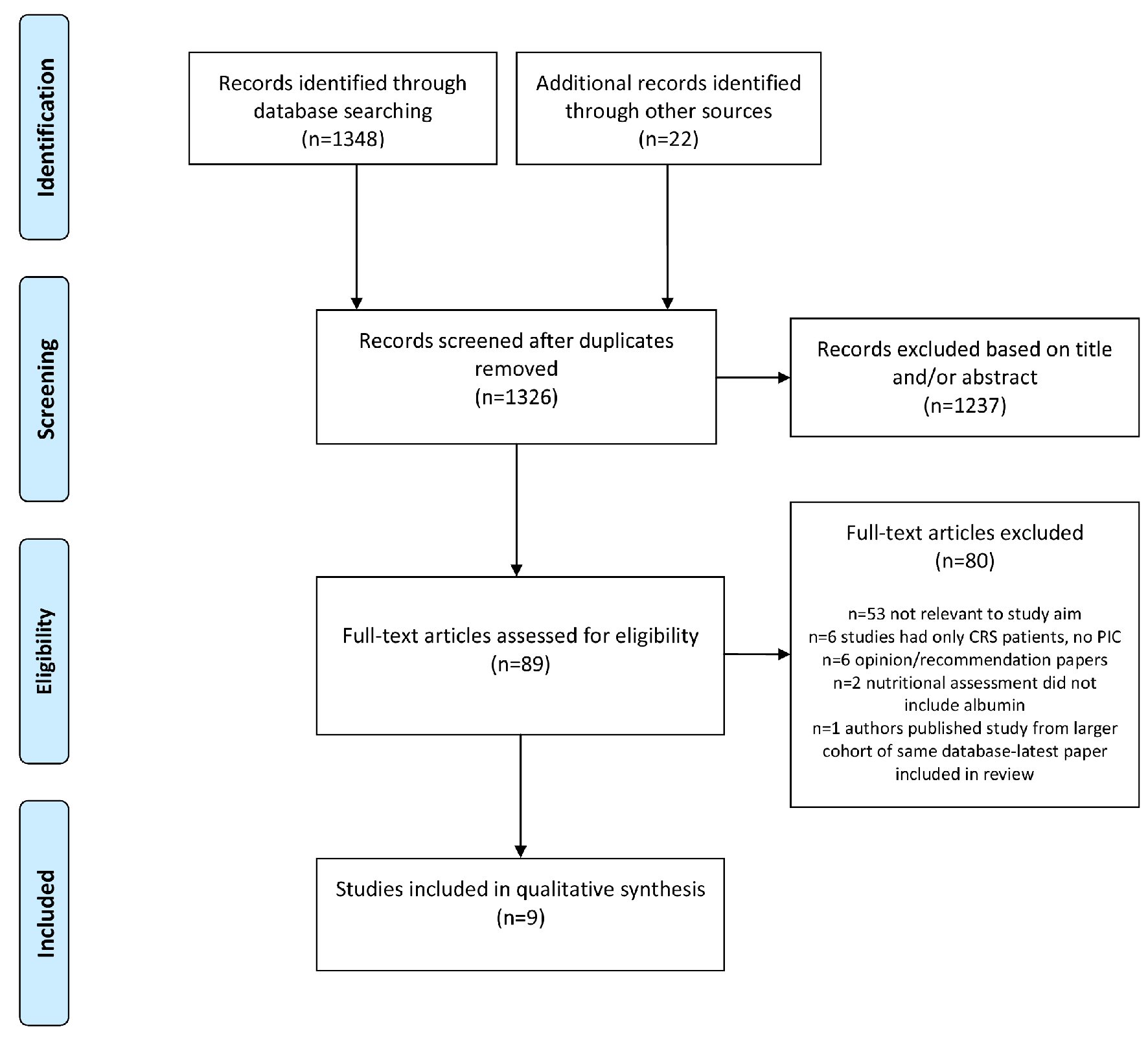
Figure 1. Flowchart of the systematic review.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://www.jocmr.org |
Review
Volume 12, Number 12, December 2020, pages 773-779
Low Preoperative Serum Albumin Levels Are Associated With Impaired Outcome After Cytoreductive Surgery and Perioperative Intraperitoneal Chemotherapy for Peritoneal Surface Malignancies
Figure
Table
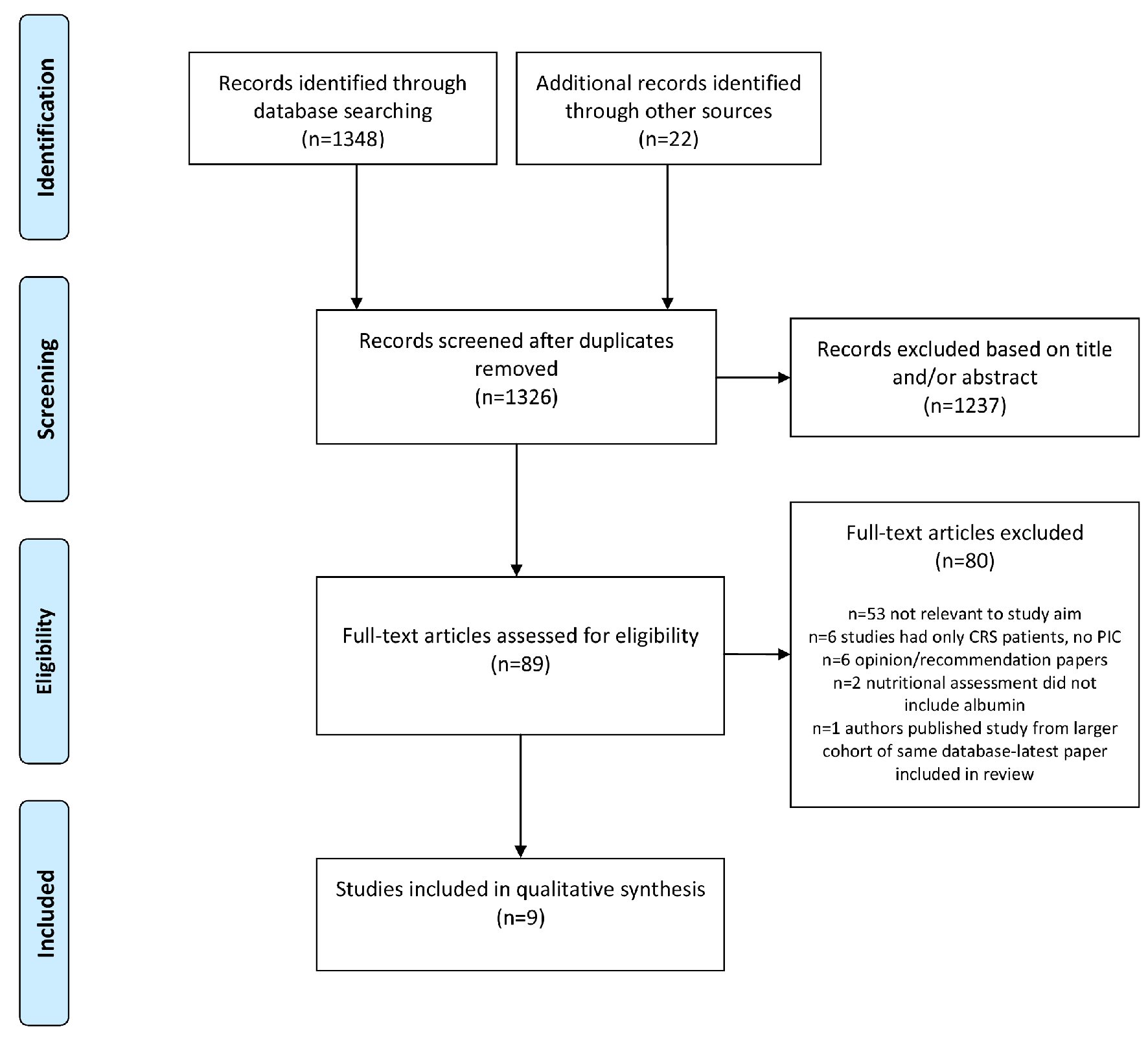
| Authors | PSM origin and study sample | Postoperative morbidity and mortality (entire cohort) | Survival (entire cohort) | Significance of hypoalbuminemia |
|---|---|---|---|---|
| OS: overall survival; PFS: progression-free survival; DFS: disease-free survival; DSM: death and serious morbidity; PM: peritoneal metastases; PSM: peritoneal surface malignancies; PMP: pseudomyxoma peritonei; LOS: length of stay; ICU: intensive care unit; HDU: high dependency unit; N.S.: non-significant; pts: patients. | ||||
| Graziosi et al, 2016 [19] | N = 64 pts with PM of various primary origins (34.4% colorectal, 32.8% gastric, 14.1% ovarian and 10.9% other origin) | 5.1% major postoperative morbidity (grades III/IV) | Median follow-up was 26.5 months (range 4 - 120 months) | With 3.8 g/dL as preoperative albumin cut-off value, 5-year OS of 70% vs. a 5- year OS of 38% in the high vs. low albumin group. |
| 5.1% postoperative mortality | 5-year OS was 55 % for entire cohort | Preoperative albumin level was identified as an independent prognostic factor for OS in multivariate analysis. | ||
| No data regarding albumin as predictor of postoperative morbidity/mortality. | ||||
| Cascales-Campos et al, 2016 [20] | N = 85 pts (> 75 years) with PM of various primary origins (42% colorectal, 31% ovarian, 20% appendiceal-PMP, 7% other origin) | 43.5% overall morbidity (grades I - IV) | No survival data | Preoperative albumin level < 3 g/dL was associated with overall morbidity (grades I - IV) in univariate analysis. |
| 23.5% and 14.4% minor (grades I/II) and major (grades III/IV) morbidity | ||||
| 5.1% 90-day mortality (2/5 of the deceased died of complications not related to CRS and PIC) | Preoperative albumin level < 3.5 g/dL was associated with major morbidity (grades III/IV) in multivariate analysis. | |||
| No survival data. | ||||
| Huang et al, 2016 [21] | N = 591 pts with PM of various primary origins (31.3% appendiceal 23.4% colorectal, 29.3% PMP, 11.5% mesothelioma, ovarian 4.7%) | 41.8% overall major morbidity (grades III/IV) | 62.2 months median OS | Preoperative albumin was 3.7 ± 0.55 g/dL for entire cohort; albumin value of 3.5 g/dL used as cut-off of hypoalbuminemia. |
| Hypoalbuminemic group had statistically significant higher PCI than the normoalbuminemic one. | ||||
| 0.8% post-operative mortality | N.S. differences in mortality between normo- and hypoalbuminemic groups (2 vs. 3 pts). | |||
| Hypoalbuminemic group had statistically significant higher rates of major morbidity (grades III/IV), as well as LOS, ICU and HDU hospitalization duration (twice median stay). | ||||
| In multivariate analysis, preoperative serum albumin < 3.5 g/dL was an independent prognostic factor for a poor perioperative outcome (grades III - V - 1.5-fold risk of a poor perioperative outcome when preoperative serum albumin < 3.5g/dL)). | ||||
| Hypoalbuminemic group had statistically significant poorer OS (49.3 months (32.0 - 66.6) vs. 65.8 months (48.5 - 83.1)). | ||||
| Peters et al, 2015 [22] | N = 1,085 pts with PM of various primary origins | 44% and 37% overall and major morbidity | No survival data | Preoperative albumin < 3 g/dL and weight loss were the only preoperative factors significantly associated with DSM in the multivariate model. |
| 1.8% postoperative mortality | ||||
| overall 30-day DSM rate of 37.4% | No survival data. | |||
| Winer et al, 2013 [23] | N = 67 pts with PM of appendiceal (AP, n = 37) or colorectal origin (CRC, n = 30) with signet cell histology | 22% vs. 29% major morbidity (grade III/IV) in the CRC vs. AP group | Median follow-up of CRC and AP groups was 4.4 and 4.1 years, respectively | In univariate analysis, preoperative albumin level < 3.5 g/dL was significant predictor of poor survival in the CRC group and marginally in the AP group. |
| 5.4% vs. 6.7% 60-day mortality for AP vs. CRC group | Preoperative albumin was not independent survival predictor in multivariate analysis in any of the groups. | |||
| PFS and OS were 9 and 12 months in CRC and 12 and 21 months in AP pts | No data regarding albumin as predictor of postoperative morbidity/mortality. | |||
| Votanopoulos et al, 2013 [24] | N =13 pts with PM from rectal primary; N = 204 pts with PM from colonic primary | 30-day mortality for colon and rectal group was 5.7% and 0%, respectively | Median follow-up was 40.1 and 88.1 months for rectal and colonic group, respectively | In univariate analysis, preoperative albumin level was not statistically significant in predicting survival in the pts groups. |
| Overall morbidity for the colon and rectal groups was 51% and 46 %, respectively | Median survival was 14.6 months for the rectal group and 17.3 months for the colon group | |||
| 3-year survival was 28.2% and 25.1 % for the rectal and colon groups, respectively | Albumin was not independent survival predictor in multivariate analysis in any of the groups. | |||
| No data regarding albumin as predictor of postoperative morbidity/mortality. | ||||
| Votanopoulos et al, 2013 [25] | N = 81 patients (> 70 years) with PM of various primary origins (39.5% appendiceal, 24.7% colorectal, 12.3% mesothelioma, 9.9% ovarian, 7.4% gastric, 6.2% other primaries) | Minor morbidity (grade I/II) was 28 %, while major morbidity (grade III/IV) was 38 % | Median follow-up was 48.1 months | Average albumin level of the entire cohort was 3.6 g/dL, while for patients with complications was 3.7 g/dL; average albumin level of those patients who suffered mortality was 3.2 g/dL. |
| 13.6% 30-day mortality for the entire cohort | Median survival stratified by primary cancer: 31.8 months for appendiceal, 41.5 months for mesothelioma, 54 months for ovarian, 13.2 months for colonic, and 7.6 months for gastric | Preoperative albumin was a significant predictor of survival in both univariate and multivariate analysis in absence of complications. | ||
| 27.4% 90-day mortality for the entire cohort | Mortality risk was reduced by 40% for each additional gram of albumin. | |||
| Deraco et al, 2012 [26] | N = 56 pts with PM from recurrent ovarian cancer | 5.3% procedure-related mortality | 23.1 months median follow-up time | Preoperative serum albumin (cut-off for hypoalbuminemia was 3.5 g/dL) was identified as independent prognostic factor of PFS and OS in multivariate analysis. |
| Overall DSM rate of 26.3% | Median OS and PFS were 25.7 and 10.8 months, respectively | |||
| 5-year OS and PFS were 23% and 7%, respectively | No data regarding albumin as predictor of postoperative morbidity/mortality. | |||
| Banaste et al, 2018 [27] | N = 214 patients with PM from colorectal primary | 50% major postoperative complication rate | Median follow-up was 24 months (range 0 - 82 months) | Preoperative serum albumin (cut-off for hypoalbuminemia was 3.5 g/dL) was identified as independent prognostic factor of PFS and OS in multivariate analysis. |
| No mortality data | Median OS and PFS were 58.9 and 13 months, respectively | Hypoalbuminemia was not a predictor of postoperative morbidity. | ||
| 3- and 5-year OS were 63% and 46%, respectively | ||||
| 3- and 5-year PFS survival were 17% and14%, respectively | ||||