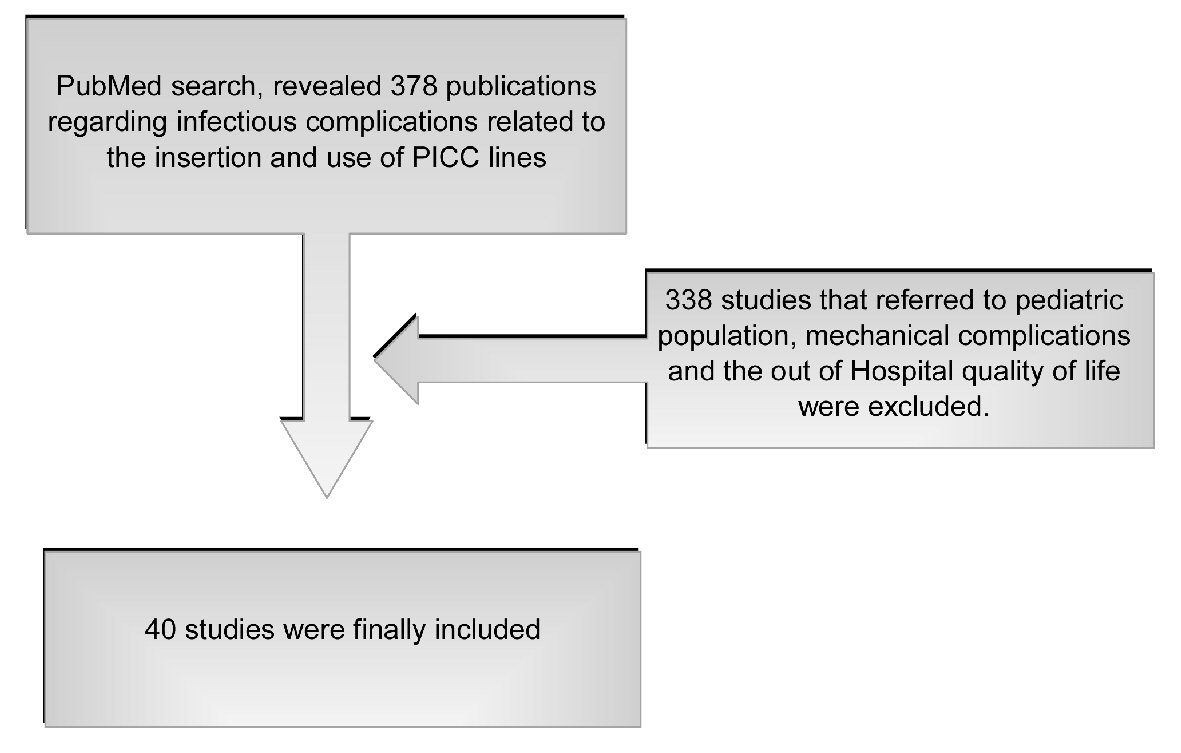
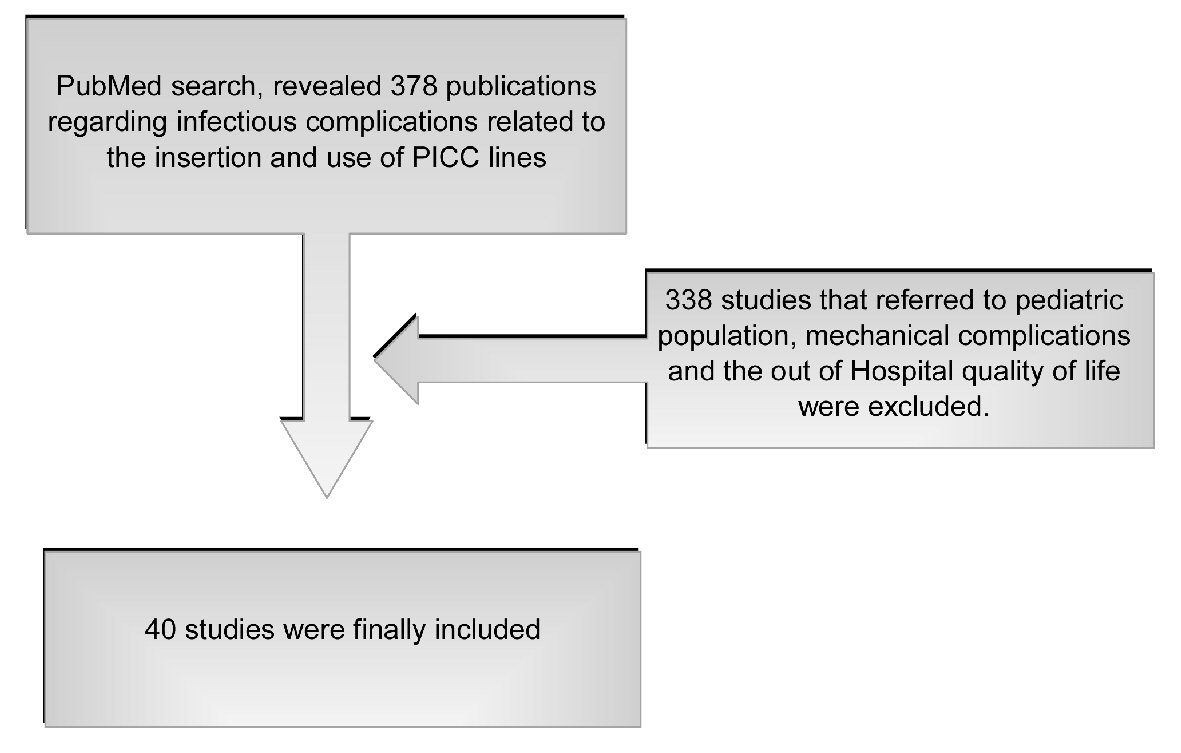
Figure 1. Literature search method.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Review
Volume 11, Number 4, April 2019, pages 237-246
Peripheral Inserted Central Catheter Use and Related Infections in Clinical Practice: A Literature Update
Figure
Table
| Study and year | Study design | Type of patients/database | Major findings |
|---|---|---|---|
| Santolim et al, 2018, [4] | Retrospective study from a single-center | Patients from Orthopedics and Traumatology Department | After insertion of 720 PICCs, no cases of PICC line infections were documented after culture of samples from catheter tips and peripheral blood. |
| Kim et al, 2018, [5] | Multi-center retrospective study | Adult patients with tunneled or conventional PICCs | Reduction rate of CLABSI related to subcutaneous tunneling approach for PICC placement |
| Kagan et al, 2018, [6] | Retrospective study | Adult ill population | PICC CLABSIs were highest among patients receiving non-antimicrobial-impregnated (NAIP) catheters. |
| Stewart et al, 2018, [7] | Retrospective study | Patients with Staphylococcus aureus bacteremia | Early PICC line insertion in Staphylococcus aureus bacteremia appears to be safe. |
| Herc et al, 2017, [8] | Study based on data from the Michigan Hospital Medicine Safety consortium | Adult patients | The Michigan PICC-CLABSI (MPC) offers a novel way to inform decisions regarding PICC use, surveillance of high-risk cohorts, and utility of blood cultures when PICC-CLABSI is suspected. |
| Martyak et al, 2017, [9] | Retrospective review | Patients with PICCs inserted by the bedside in the ICU and PICCs placed by interventional radiology in non-ICU | PICC lines placed at the bedside in the ICU setting were associated with higher complication rates, in particular infectious complications. |
| Lo Priore et al, 2017, [10] | Retrospectively collected data | Mainly oncology patients | Decreased infectious rate after implementing a systematic surveillance program |
| Chaftari et al, 2017, [11] | Prospective single institution study | Patients with hematologic malignancies | Non-antibiotic catheter lock solution with nitroglycerin, ethanol and sodium citrate reduced CLABSI. |
| Jacques et al, 2018, [12] | Retrospective case series | Pregnant and postpartum patients | No differences in infectious rate compared to non-pregnant |
| Kang et al, 2017, [13] | Prospective, multi-center, cohort study | Cancer patients | CLABSI rate 1.3%. Increased MBI was related to more complications. |
| Chen et al, 2017, [14] | Retrospective study | Acute myeloid leukemia patients | Bacteremia in patients with PICCs was comparable to that of other IV lines. |
| Xu et al, 2016, [15] | Retrospective study | Patients from a large academic medical center | PICCs complications were less but more serious (including bacteremia) when compared to midline peripheral catheters |
| Kim-Saechao, et al, 2016, [16] | Historical cohort study | Patients in an academic tertiary medical center | Application of a mandatory electronic communication tool (MECT) based on clinical practice guidelines decreased CLABSI. |
| Storey et al, 2016, [17] | Randomly assignment of patients | Patients in three high-risk units | No differences in CLABSI development in patients with chlorhexidine (CHG)-impregnated or non-CHG PICC line |
| Pernar et al, 2016, [18] | Retrospective review of prospectively collected data | Patients’ requests for PICCs maintained in database (2000-13) | Implementation of a surgeon-led PICC team had among other, significant impact on the avoidance of complications of PICC lines. |
| Bertoglio et al, 2016, [19] | Prospective study | Oncology patients | PICC is a safe venous device for chemotherapy delivery with CLABSI incidence 1.7%. |
| Nolan et al, 2016, [20] | Retrospective cohort study | Adult ITU patients | PICCs (dual/triple lumen) and centrally inserted central catheter CICCs (triple/quadruple lumen) were compared for complications of both groups. Infections were uncommon following PICC and CICC insertion, with no significant difference in complication rates. |
| Sriskandarajah et al, 2015, [21] | Retrospective single center | Oncology patients | Comparison of the incidence of thrombosis and infections in two groups who had either PICCs or long-term skin tunneled catheters (LTSTCs). In regards to infection, incidence rate was higher in the PICC group. |
| Rhee et al, 2015, [22] | Retrospective observational study | Non-ICU patients | In non-ICU patients with CLABSIs, underlying hematologic malignancy, neutropenia, and PICC lines were highly prevalent in this population. |
| Seckold et al, 2015, [23] | Systematic review of prospective and retrospective studies in the English language referring to January 2000 until October 2013 | general population groups as well as oncology and non-oncology patients | Both silicone and polyurethane PICC lines exhibit nearly identical overall average post-insertion compilation rates. Oncology patients experience higher levels of post-insertion complications. |
| Austin et al, 2015, [24] | Single institution retrospective cohort review | Patients in both critical care and burn settings | PICC line-associated complication rates are similar to those published in the critical care literature. Although higher than those published in the burn literature, they are similar to central venous catheter-associated complication rates. While PICC lines can be a useful resource in the treatment of burn patients, they are associated with significant and potentially fatal risks. |
| Coady et al, 2015, [25] | Observational study | Oncology patients with solid tumors | Central venous ports and PICC lines in patients on chemotherapy had lower line infection rates than tunneled catheters. |
| Barsun et al, 2014, [26] | Retrospective review | Burn patients | Severe burn injury patients, long hospital admissions, and later hospital day of PICC insertions are at higher risk of developing PICC infections. |
| O’Brien et al, 2013, [27] | Data collected for the period from May 2011 until January 2012 | Patients in a university center in Canada | Insertion of PICCs with minimum number of lumens reduces complications. |
| Chopra et al, 2013, [28] | Meta-analysis | Adult patients | No differences in development of CLABSI in hospitalized patients with PICCs or CVCs. Consideration of risks and benefits before PICC use in inpatient settings is necessary. |
| Leroyer et al, 2013, [29] | Prospective study | Patients with PICC under interventional radiology | Higher infection rate for PICCs compared to CVCs |
| Baxi et al, 2013, [30] | Retrospective cohort study | University of Michigan Health System | High risk of CLABSI was related to immunosuppression, three PICC lumens and power-injectable PICC. |
| Armstrong et al, 2013, [31] | Comparison between studied patients and a retrospective group | Burn patients | Bacteremia rates were decreased in the burn patients who received antibiotic impregnated PICC lines. |
| Ugas et al, 2012, [32] | Review | Critically ill surgical patients | For the period 1999 - 2011, there is a paucity of studies investigating the incidence of CVC- and PICC-related CLABSI in critically ill surgical populations. |
| Petree et al, 2012, [33] | Review | Patients eligible for PICC insertion | Specific strategies for skin decontamination, sterile barriers, needleless connectors and positive-pressure valves and proper securement with self-adhesive anchoring devices were more effective to reduce CLABSIs. |
| Al-Tawfig et al, 2012, [34] | Prospective study | All patients with PICCs hospitalized in a center in Saudi Arabia | An overall BSI rate 4.5/1000 PICC-days was reported. The development of BSI was related to the underlying conditions and indications for the PICC line use. |
| Mollee et al, 2011, [35] | Prospective, observational study | Oncology patients in a single medical center in Australia | There is a need for standardized surveillance strategy in oncology adult patients, the use of PICC lines in such patients is supported, also the side of line insertion may influence risk of ClABSI. |
| Butler et al, 2011, [36] | Retrospective review | Patients in a large academic hospital | Previous placement of a PICC may be related to catheter-associated infections in hemodialysis patients. |
| Gunst et al, 2011, [37] | Non-randomized study | Surgical ICU patients | PICCs were associated with fewer CLABSIs in long-stay surgical ICU patient compared to CVCs. |
| Fearonce et al, 2010, [38] | Review | Burn patients in a single center | PICC lines had a lower incidence rate for CLABSI compared to CVCs. |
| Al-Raiy et al, 2010, [39] | Prospective study | Patients with CVCs in the ICUs and patients with PICCs hospital-wide | The median time for infection development was significantly longer in the patients with PICCs compared to CVCs. |
| Yap et al, 2006, [40] | Study based on prospectively collected PICC complication data | Oncology patients with solid tumors | Complication rate for year 2003 was lower compared to that of 2001 probably due to application of related strategies. |
| Griffiths et al, 2002, [41] | Prospective study | Comparison of patients with PICCs, CVCs, and peripheral venous access device | PICCs are considered a safe alternative. |
| Cowl et al, 2000, [42] | Prospective study | Patients who received TPN via a PICC or CVC | Regarding infections, the overall rate was similar for each catheter type. |
| Duerksen et al, 1999, [43] | Study based on prospectively collected data compared over 3 different time periods | Patients who received parenteral nutrition | Regarding infections, PICCs do not result in increased line-related sepsis. |