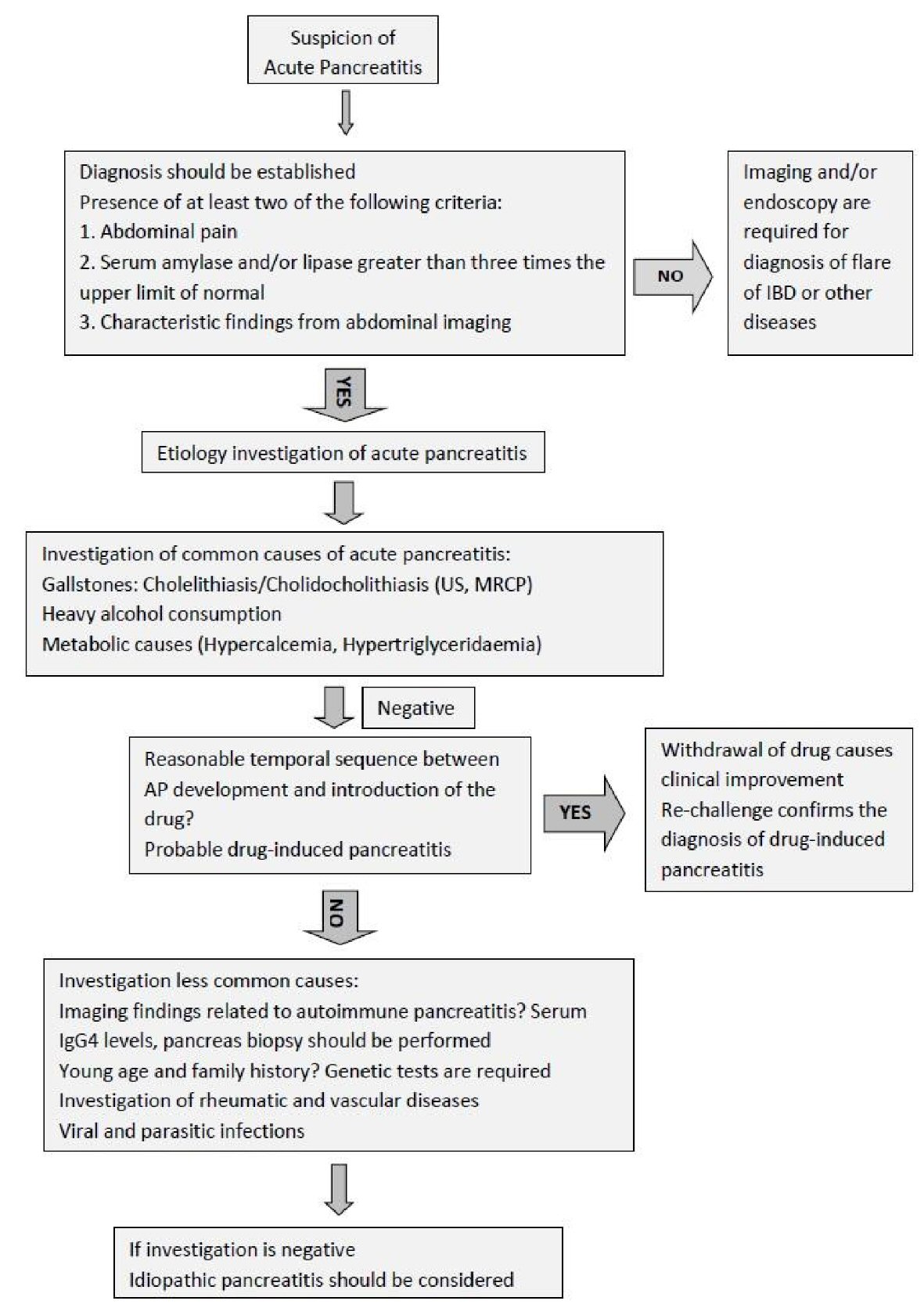
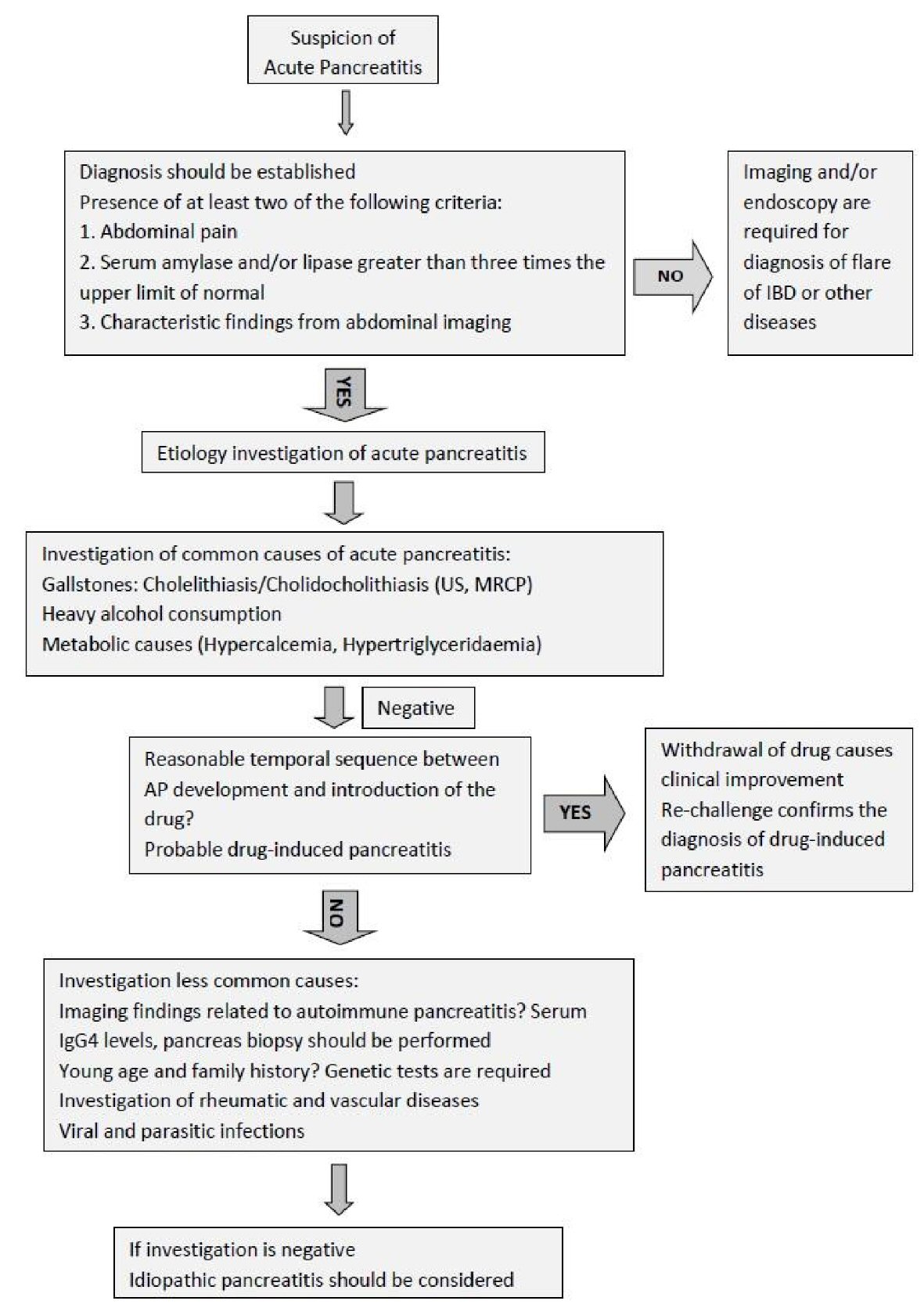
Figure 1. Diagnostic algorithm of causes of acute pancreatitis.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Review
Volume 10, Number 10, October 2018, pages 743-751
Pancreatic Involvement in Inflammatory Bowel Disease: A Review
Figure
Tables
| Crohn’s disease | Ulcerative colitis | |
|---|---|---|
| (+): association; (++): more frequent than other type of IBD | ||
| Acute pancreatitis | ++ | + |
| Autoimmune pancreatitis | + | ++ |
| Chronic pancreatitis | ++ | + |
| Pancreatic insufficiency | + | ++ |
| Pancreatic autoantibodies | ++ | + |
| Benign abnormalities of pancreatic duct | + | + |
| Elevation of serum pancreatic enzymes | ++ | + |
| Study | Bemerjo F. et al [4] | Weber P. et al [5] | Rasmussen H.H. et al [6] | Chen Y.T. et al [7] |
|---|---|---|---|---|
| Methodology | Retrospective multicentric cohort | Retrospective single center | Danish cohort study from 1977 to 1992 | Population-based cohort study from 2000 to 2010 |
| Study of origin | Spain | Germany | Denmark | Taiwan |
| Number of patients | 5,073 IBD patients | 852 CD patients | 15,526 IBD patients, 3,538 CD patients, 11,215 UC patients, 773 indeterminate colitis (IC) patients | 11,909 IBD patients |
| Type of IBD | ||||
| Follow-up period | 14 years | 10 years | 112,824 person-years | 5.33 ± 3.79 years |
| Episodes of acute pancreatitis | 82 | 12 | 86 | 202 |
| Incidence of acute pancreatitis | 1.6% | 1.4% | CD patients: 4.3%, UC patients: 2.1%, IC patients: 7.1% | 31.8 per 100,000 person-years |
| Number of patients with acute pancreatitis (CD/UC) | 67 patients (53 CD/14 UC) | 12 CD patients | 86 (28 CD/50 UC/8 IC) | 202 patients (128 CD/74 UC) |
| Age of patients with acute pancreatitis | 40 ± 12 years (mean ± standard deviation) | Median 23 (10 - 50) | Unknown | Unknown |
| Etiology | 63.4% drug-induced, 20.7% idiopathic, 12.2% cholelithiasis, 3.7% miscellaneous causes | 83% unknown (common causes were excluded), 17% drug-induced | Unknown | Unknown |
| Cholelithiasis |
|---|
| Medications |
| Thiopurines (azathioprine/6-mercaptopourine) |
| Analogues of 5-ASA (mesalamine, sulfasalazine, olsalazine) |
| Metronidazole |
| Corticosteroids |
| Cyclosporine |
| Duodenal involvement of Crohn’s disease |
| Ampullary inflammation |
| Duodenopancreatic fistula |
| Primary sclerosing cholangitis |
| Cholelithiasis |
| Strictures of common bile duct and of pancreatic ducts |
| Hypercoagulation |
| Withdrawal of azathioprine/6-mercaptourine and 5-ASA analogues, if there is suspicion for drug-induced AP and the common causes have been excluded |
| Aggressive intravenous fluid resuscitation |
| 250 - 500 mL per hour during the first 12 - 24 h |
| Lactated Ringer’s should be the preferred isotonic crystalloid fluid; it is contraindicated in hypercalcemia |
| Fluid administration should be titrated according to urine output and comorbidities of patient |
| Electrolyte replacement |
| Analgesia |
| Bowel rest |
| In mild AP, oral feeding can be started immediately, if there is not nausea, vomiting and abdominal pain has resolved |
| In several AP, enteral nutritional is recommended to prevent infectious complications |
| Management of complications of AP |
| If co-existing active IBD, infliximab and corticosteroids may be used |