Figures
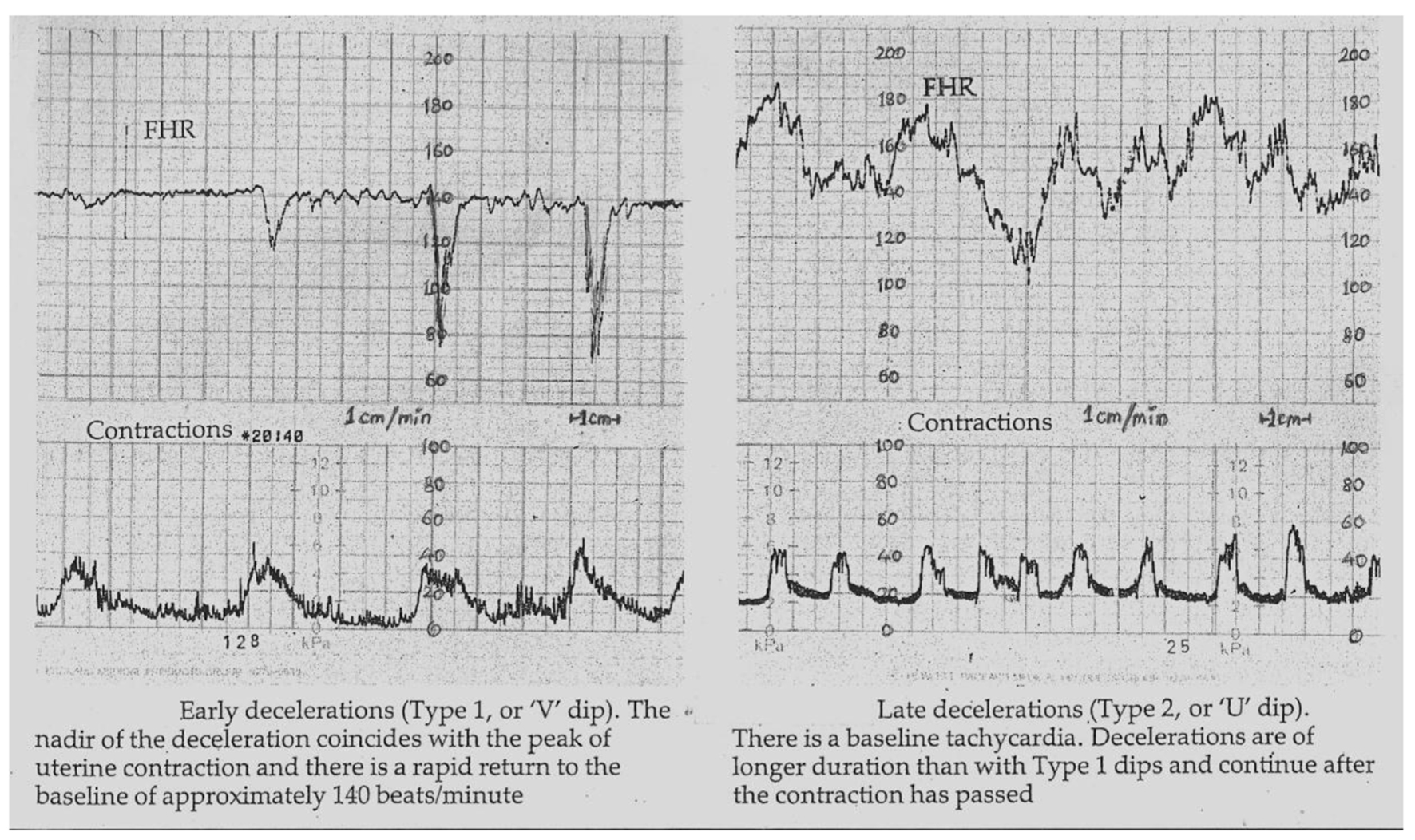
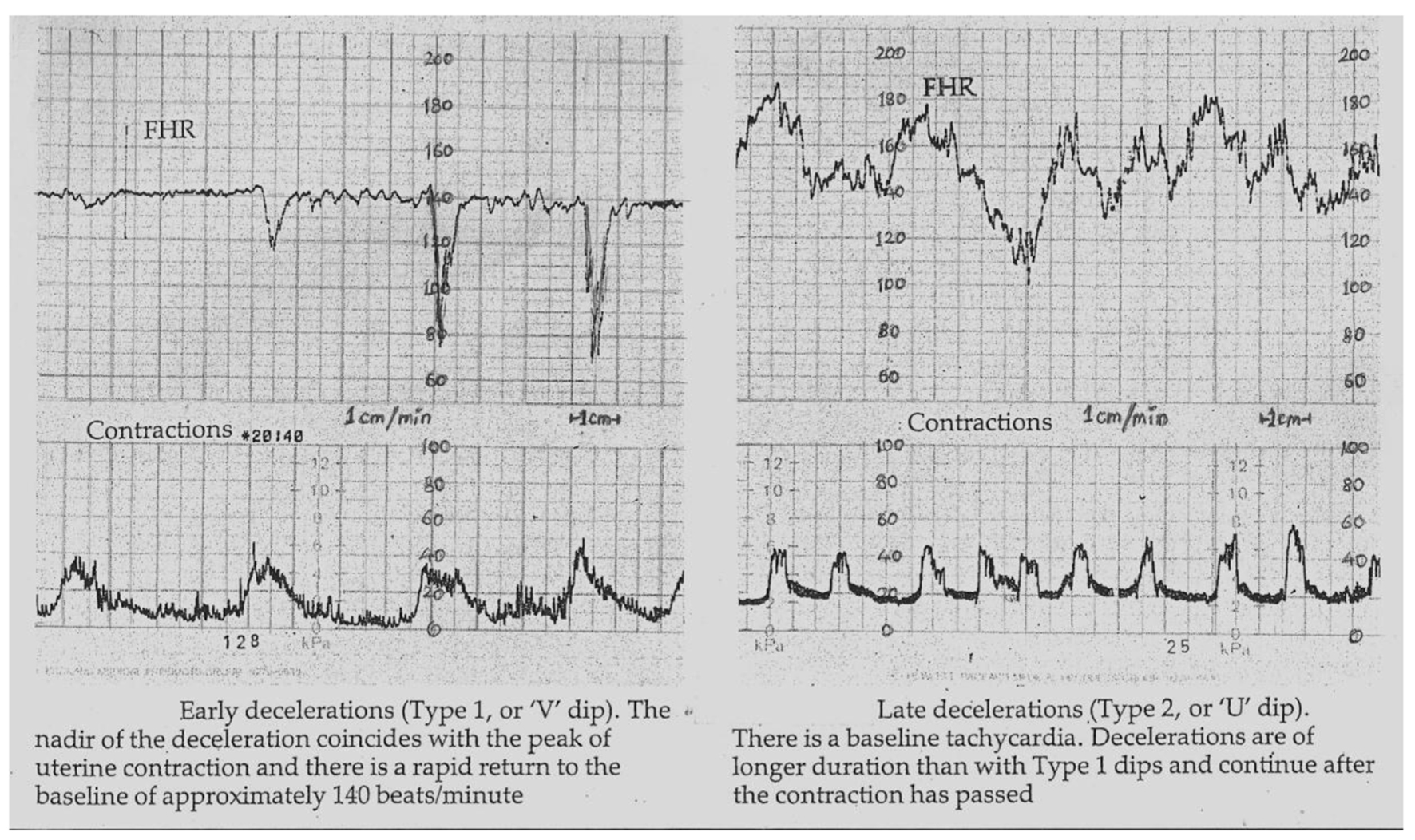
Figure 1. Early and late decelerations in traditional British practice (Reproduced with permission from “Principles of Obstetrics” by Bryan Hibbard, 1988) [17]. Note “rapid rather than gradual descent” of early as well as some of the late FHR decelerations. Illustrations by other British authorities before 2007 were also very similar [14-16]. Many old as well as recent illustrations [25-27] show that late decelerations on British CTG can look more like “V” than “U” especially when they are deep (more serious). Hence there is a danger of miscategorising late decelerations if “gradual” shape is included in the British definition of late decelerations.
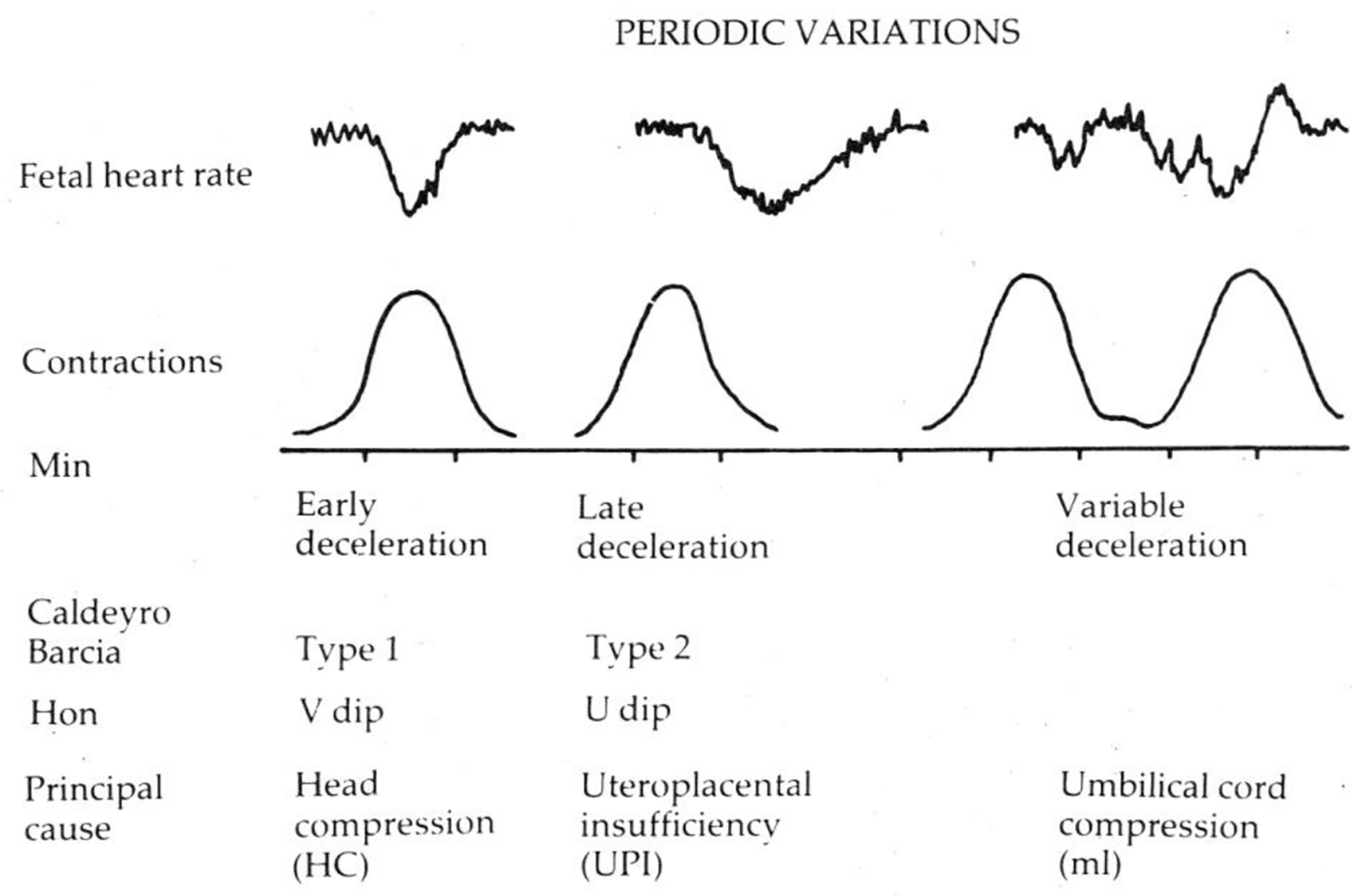
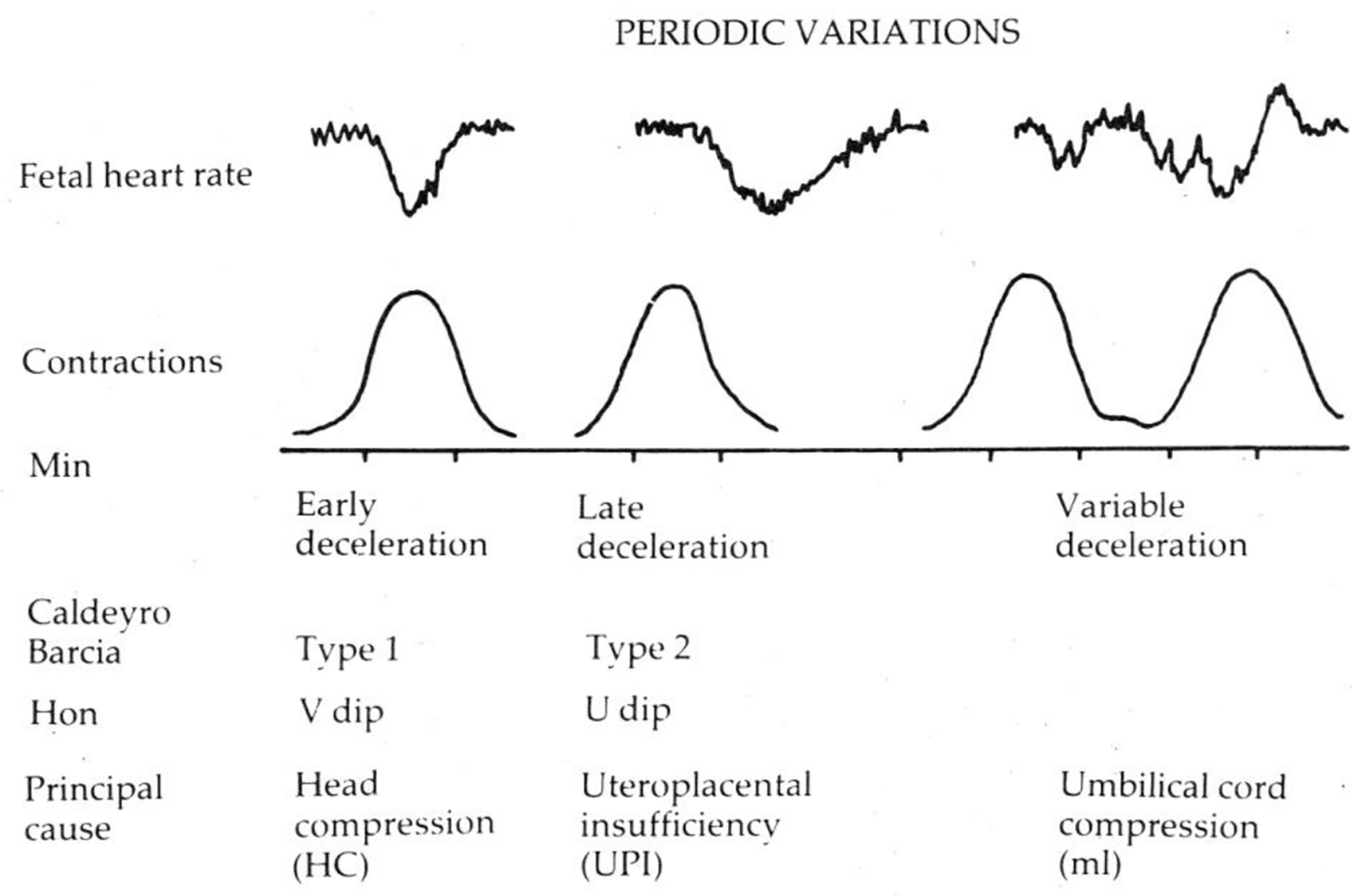
Figure 2. Diagrammatic representation of early, late and variable decelerations as practiced in British Obstetrics before 2007 (Reproduced with permission from “Principles of Obstetrics” by Bryan Hibbard, 1988) [17]. Etiology is not a primary defining feature. Late decelerations are described as “U”-shaped only in contrast with “V”-shaped early decelerations.
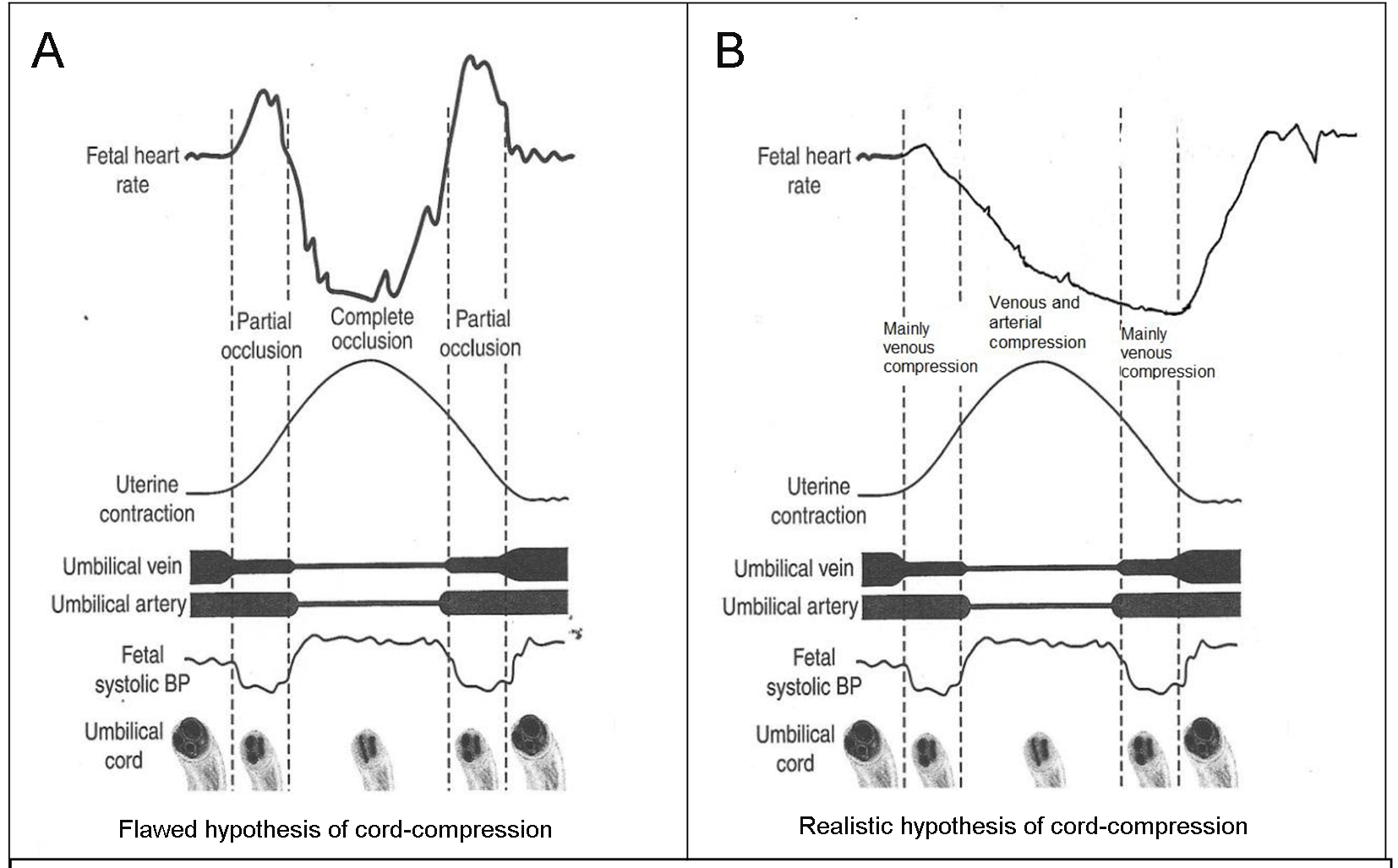
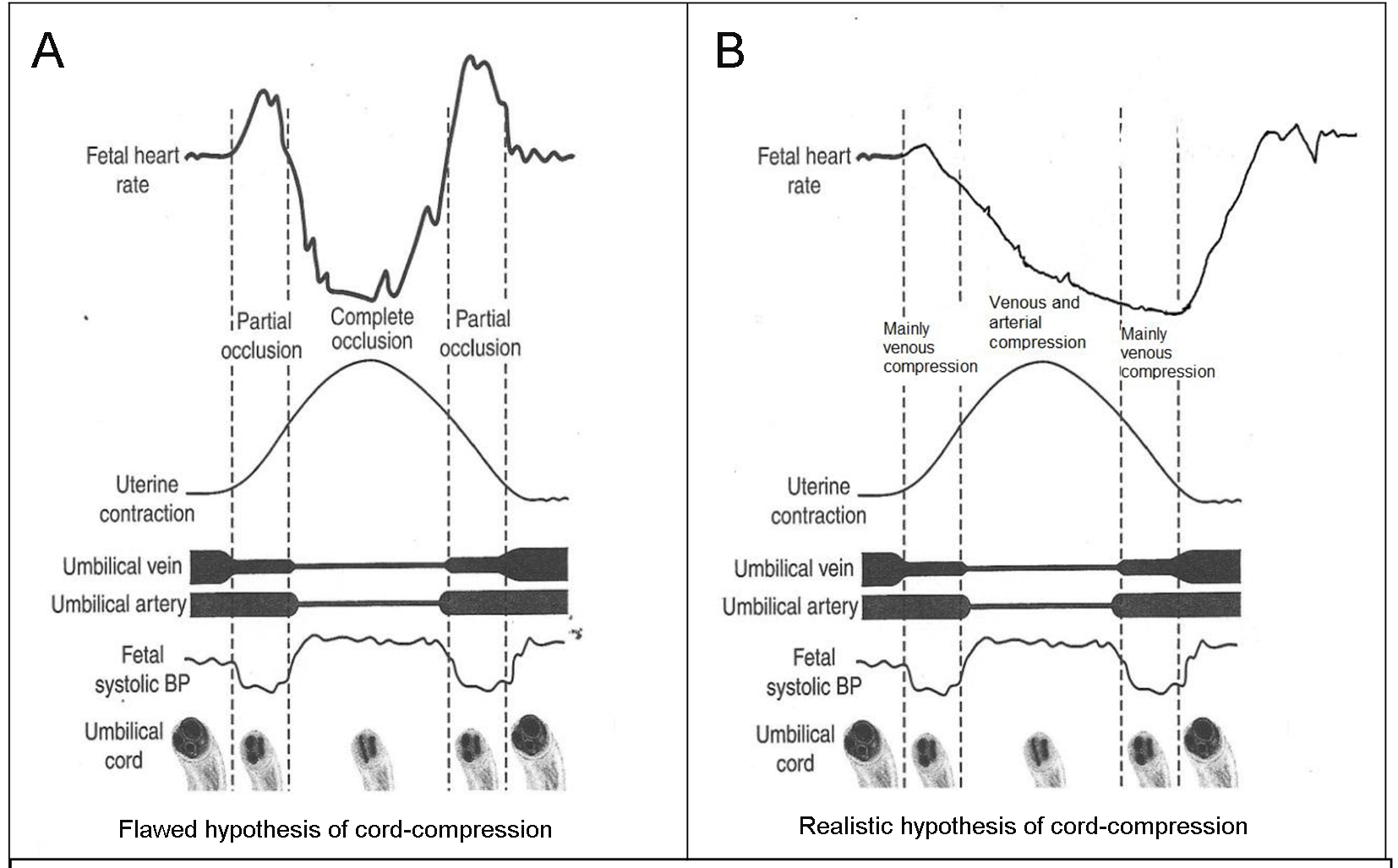
Figure 3. (A) Popular but flawed hypothesis of cord-compression and variable deceleration [25-27, 31, 32]. CTG speed 3 cm/min. Thankfully reproduced from J Clin Med Res. 2015;7:672-80 [13]. This hypothesis has major fallacies. Complete cord-compression has been postulated for these most common decelerations. FHR recovery commencing at the height of contraction (where umbilical arterial and venous occlusion is unrelieved) cannot be explained. Instead the deceleration depicted seems consistent with “non-hypoxic” vagal reflex (e.g. head-compression). (B) Diagrammatic illustration of how “cord-compression” deceleration would actually look like (CTG speed 3 cm/min). Both baro and chemoreceptor mechanisms come into play as shown by many animal studies [12, 33]. The shape will look more rapid (V shaped) on British CTG (speed 1 cm/min). The nadir is reached well after the peak of contraction and recovery would start when umbilical vein compression (i.e. hypoxemia) is being relieved. This is clearly borne out in the Figure 5, where an example of FHR deceleration with known cord compression is given [12].
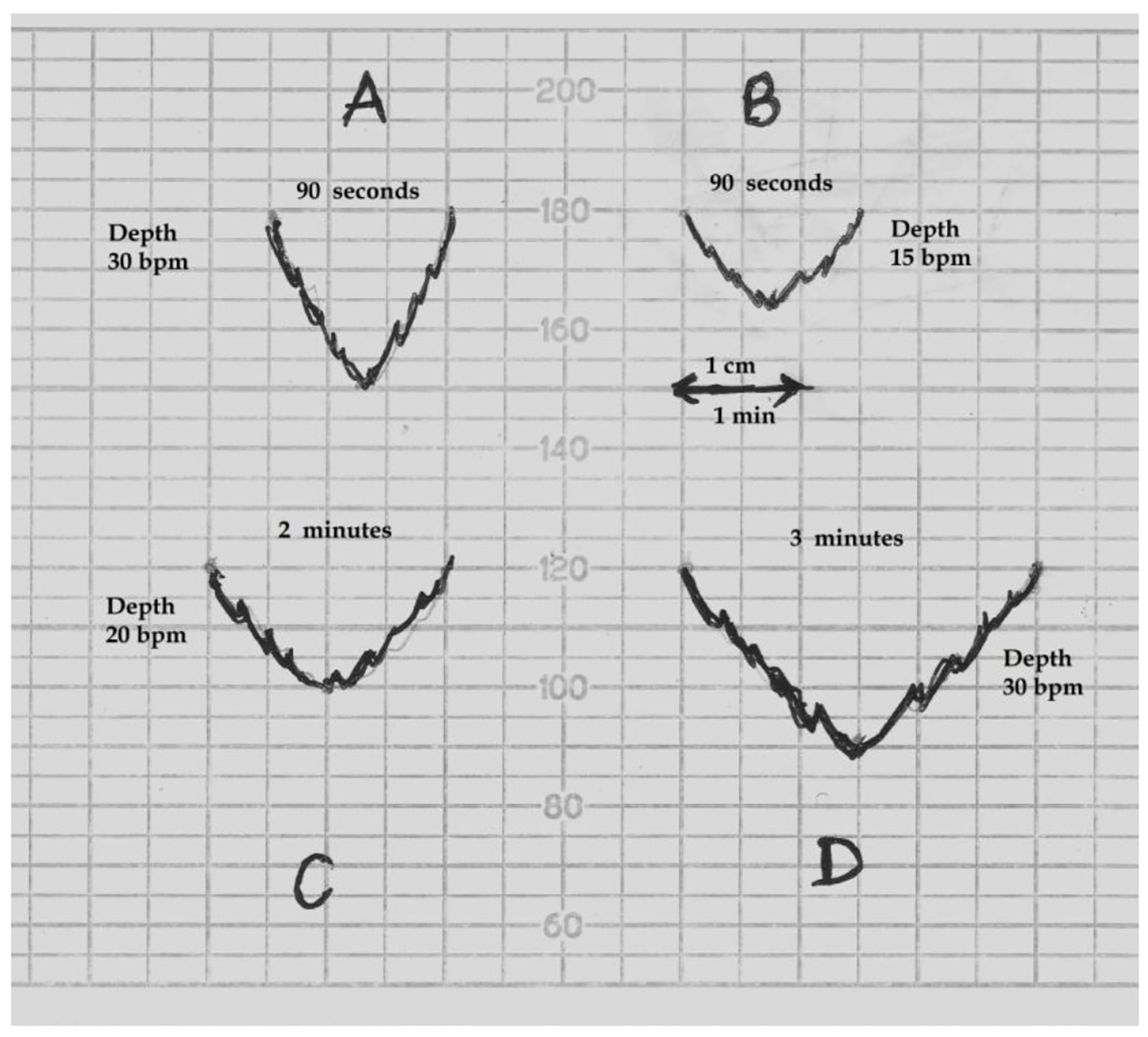
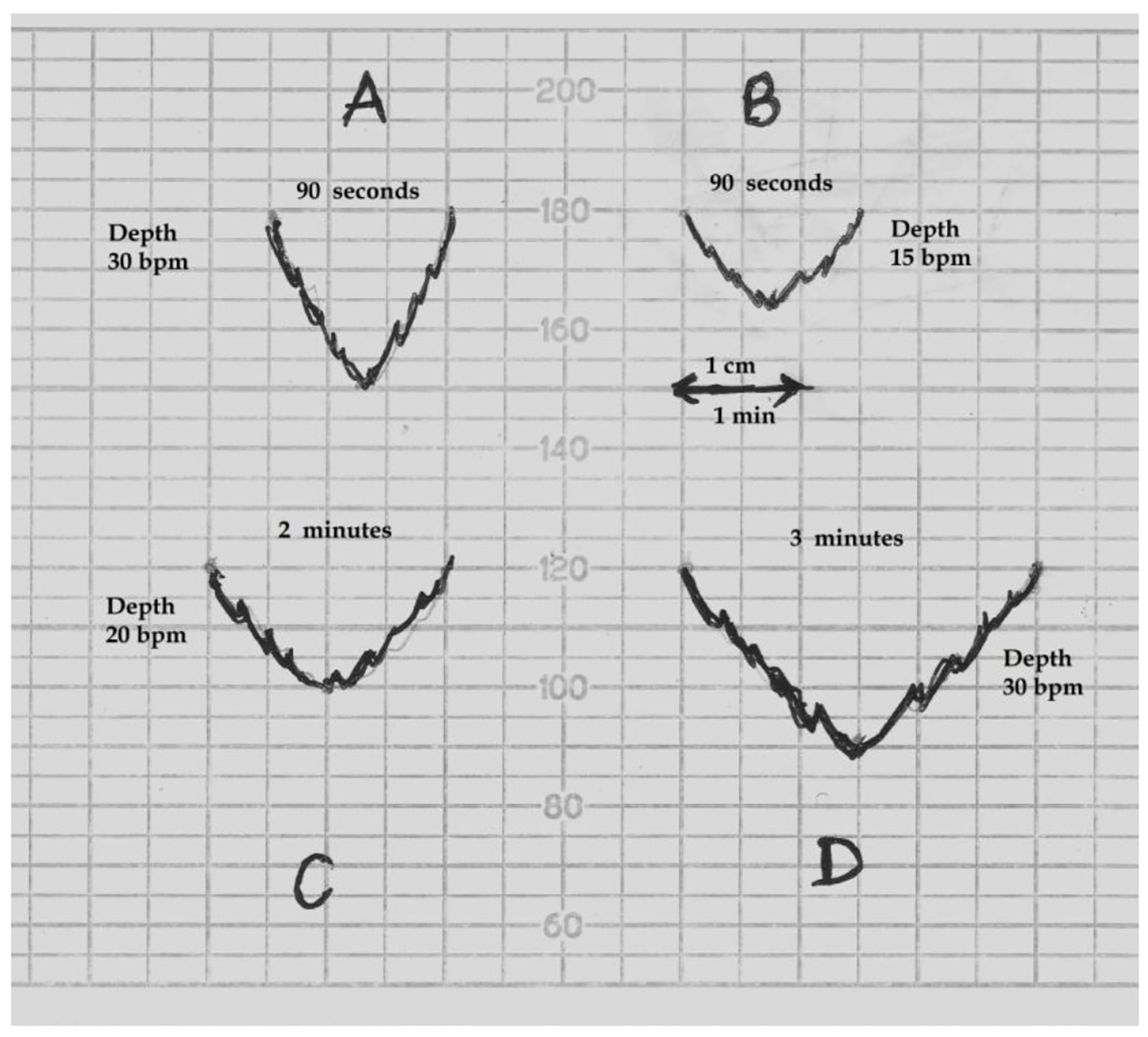
Figure 4. Schematic drawing of FHR decelerations on the British CTG paper (recording speed 1 cm/min). bpm: beats per minute. (A) This deceleration with W/D (width to depth) ratio of 1:1 or less will appear “rapid”. (B) A deceleration will need W/D ratio of about 2:1 or more to appear “shallow/gradual”. Thus a smallest deceleration of depth 15 bpm will need to be about 90 s or more in duration to appear “shallow”. (C, D) Decelerations of depth 20 and 30 bpm will need to be around 2 and 3 min or more in duration respectively to appear “shallow”. Thus “shallow/gradual and short lasting” decelerations coincident with contractions are physically not possible on British CTG.
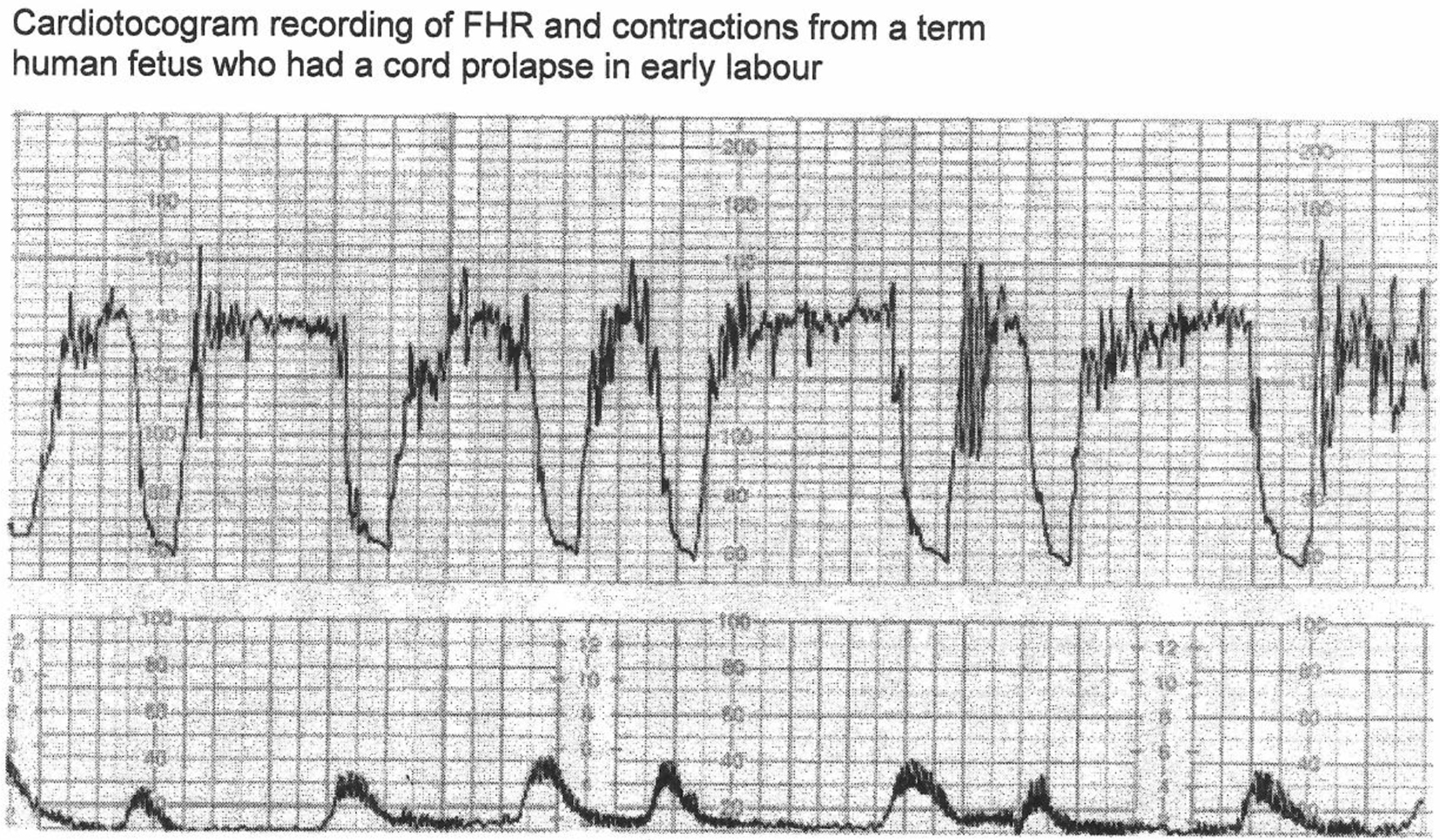
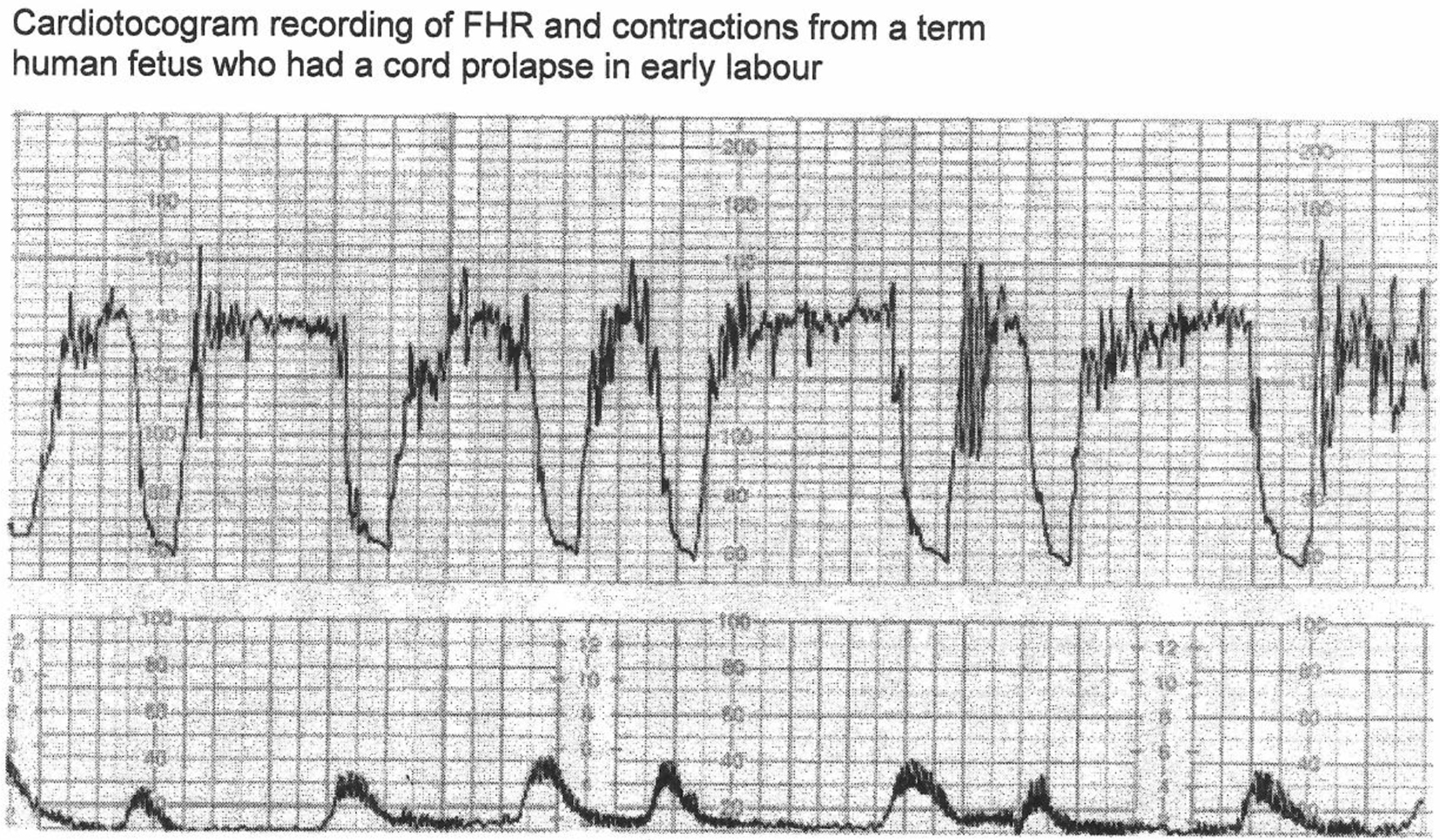
Figure 5. CTG in a case of cord prolapse showing decelerations classed as “variable” by experts [12]. Reproduced with thanks from Westgate et al, Am J Obstet Gynecol. 2007;197:236.e1-11 [12]. Although these decelerations “look” rapid (paper speed 1 cm/min), the “descent-time” is well over 30 s. Moreover, these proven cord-compression decelerations look very different from the vast majority of decelerations coincident with contractions. By FIGO (2015) guidelines these variable decelerations could be mistakenly classed as benign as they are less than three minutes in duration [3].
Table
Table 1. Proposed (British) Definitions of FHR Decelerations
| These definitions are very similar to the traditional British practice between 1970 and 2007 [14-17] and of Edward Hon [21]. |
| Early decelerations | Recurrent/repetitive slowing of FHR (depth > 15 beats/min) with onset early in the contraction and return to baseline at the end of contraction. |
| Late decelerations | Recurrent/repetitive slowing of FHR with onset mid to end of contraction and nadir more than 20 s after peak of contraction and ending after the contraction. If baseline variability is less than 5 beats/min, then the definition would include decelerations less than 15 beats/min. |
| Variable decelerations | Recurrent/repetitive slowing of FHR with varying time relationship to the contraction cycle. They tend to markedly vary in shape. (Variable decelerations could be further classed as abnormal or complicated (the term atypical is now tainted) if more than 50% of them have late components, but this has to be interpreted in the clinical context.) |