| Lung cancer (n = 9) |
| 1/78/F | Non-small cell carcinoma | Mid-trachea stenosis | 4.4 × 3.5 cm mass in superior mediastinum compressing the trachea | Mid-trachea | 16 × 40 mm | Nil |
| 2/63/M | Sarcomatoid cancer | RMB obstruction | RUL mass | RMB | 12 × 40 mm | RT |
| 3/61/M | Squamous cell carcinoma lung | RMB and BI obstruction | 4.5 × 4.7 × 4.6 cm Rt. hilar mass with complete collapse if Rt. lung | RMB and BI | 14 × 40 and 14 × 40 mm | RT and chemotherapy |
| 4/58/M | Adenocarcinoma lung | RMB obstruction | 12.8 × 7.7 × 7.5 cm RUL mass with SVC obstruction | RMB | 16 × 40 mm | Nil |
| 5/74/F | Adenocarcinoma lung | RMB obstruction | RUL mass with collapse of RUL | RMB | 12 × 40 mm | RT (9#) |
| 6/70/M | Squamous cell carcinoma | Mid-tracheal and RMB obstruction | - | Trachea | 16 × 40 mm | Chemotherapy and RT |
| 7/70/M | Squamous cell carcinoma | Distal trachea, proximal Rt. Main and proximal Lt. main obstruction | Infiltrate | Right and LMB | 12 × 40 and 12 × 40 mm | RT (35#) |
| 8/77/M | Squamous cell carcinoma | | - | RMB | 10 × 40 mm | RT |
| 9/67/F | Squamous cell carcinoma | Distal trachea narrowing to 0.4 cm and Rt. Main obstruction | 6.1 × 5.5 × 6.5 cm RUL mass with tracheal compression | Distal trachea | 16 × 40 mm | RT (12#) |
| Esophageal cancer (n = 5) |
| 10/58/M | Squamous cell carcinoma | LMB obstruction | 5.2 × 3.8 × 2.4 cm mass in posterior mediastinum | LMB | 14 × 40 mm | Ivor-lewis surgery with chemotherapy and RT prior to stenting |
| 11/66/M | Squamous cell carcinoma | LMB obstruction | - | LMB | 14 × 40 mm | |
| 12/68/M | Squamous cell carcinoma | LMB obstruction | - | LMB | 14 × 40 mm | Chemotherapy and RT |
| 13/55/M | Squamous cell carcinoma | LMB obstruction | - | LMB | | Chemotherapy |
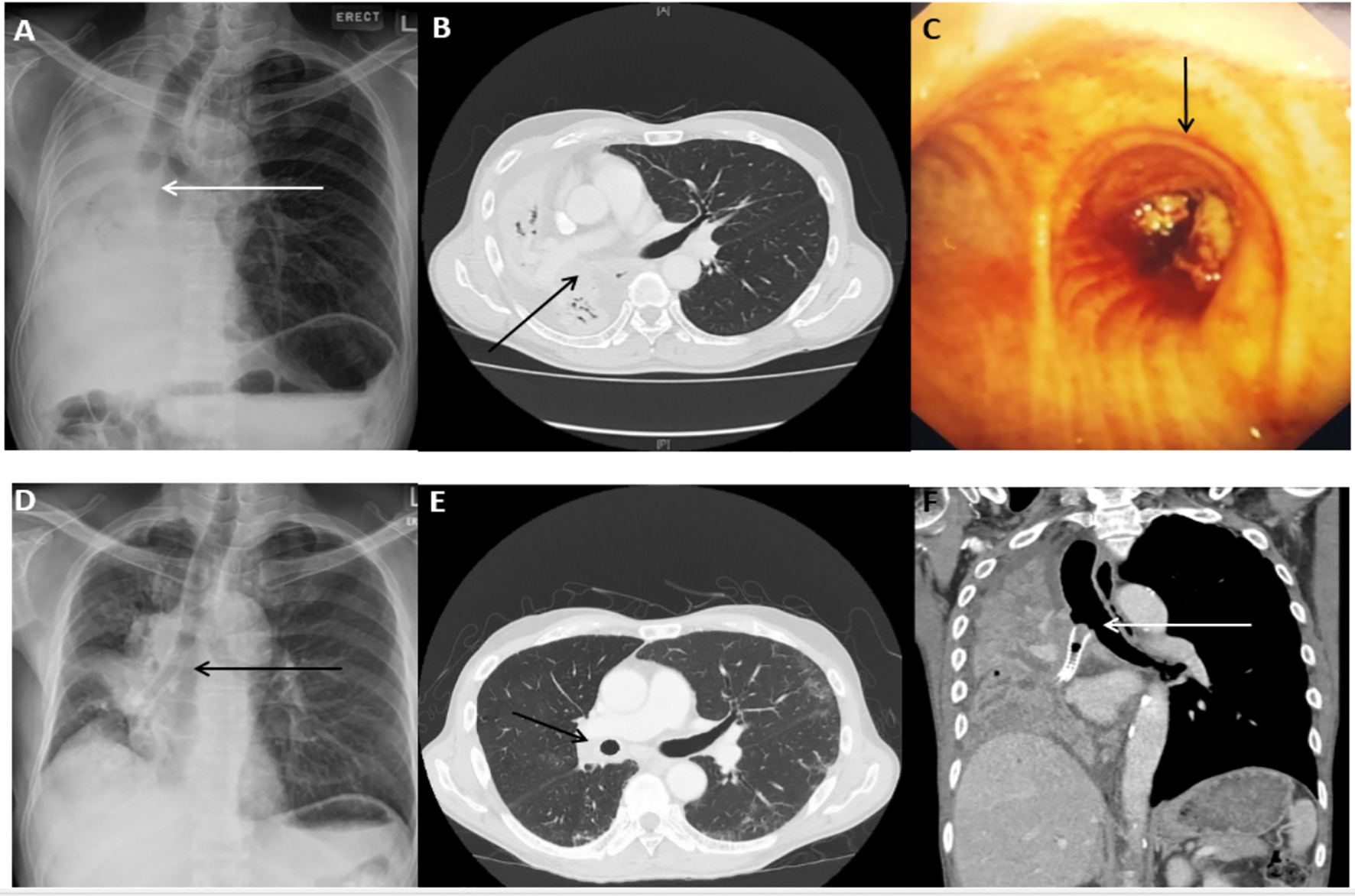
| 14/63/M | Adenocarcinoma | LMB esophageal fistula | Bilateral infiltrates from aspiration pneumonia | LMB | 18 × 40 mm | Ivor-lewis surgery prior to stenting |
| Thyroid cancer (n = 2) |
| 15/54/F | Anaplastic thyroid carcinoma | Upper tracheal narrowing to 0.5 cm | 5.2 × 6.2 × 6.4 cm mass in the thyroid gland | Upper trachea | | Nil |
| 16/76/F | Anaplastic thyroid carcinoma | Sub-glottis and upper tracheal stenosis | 6.6 × 3.3 × 5.6 cm mass in the thyroid gland | Upper trachea | 18 × 60 mm | Nil |