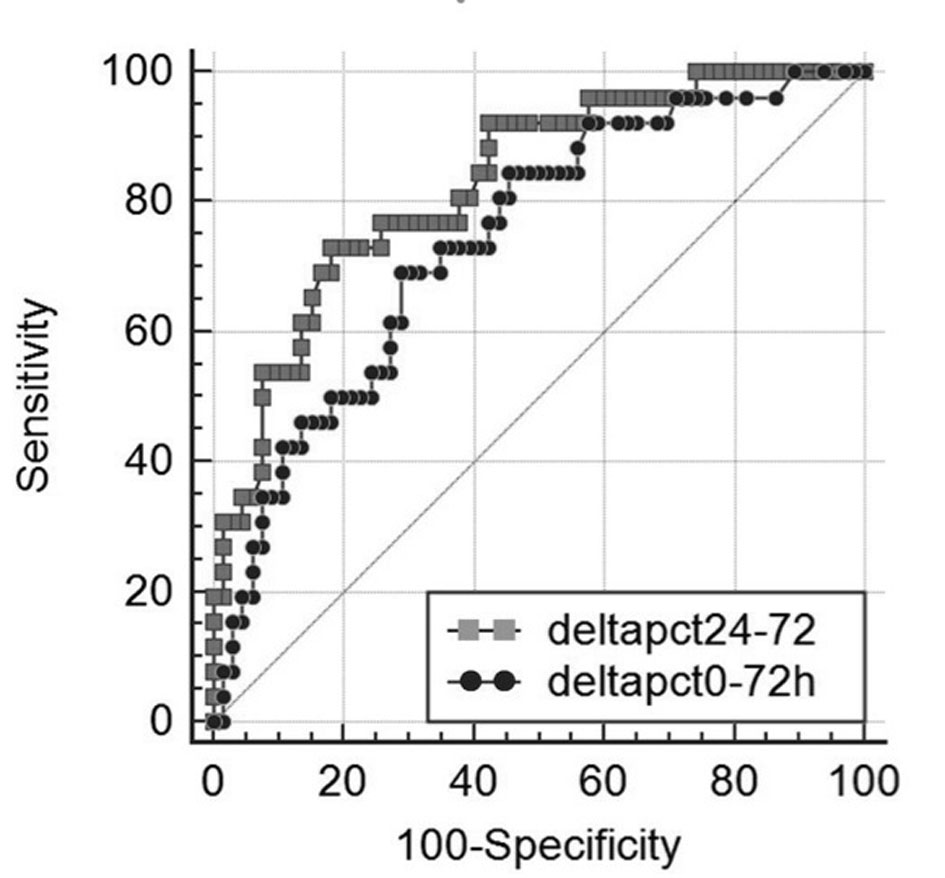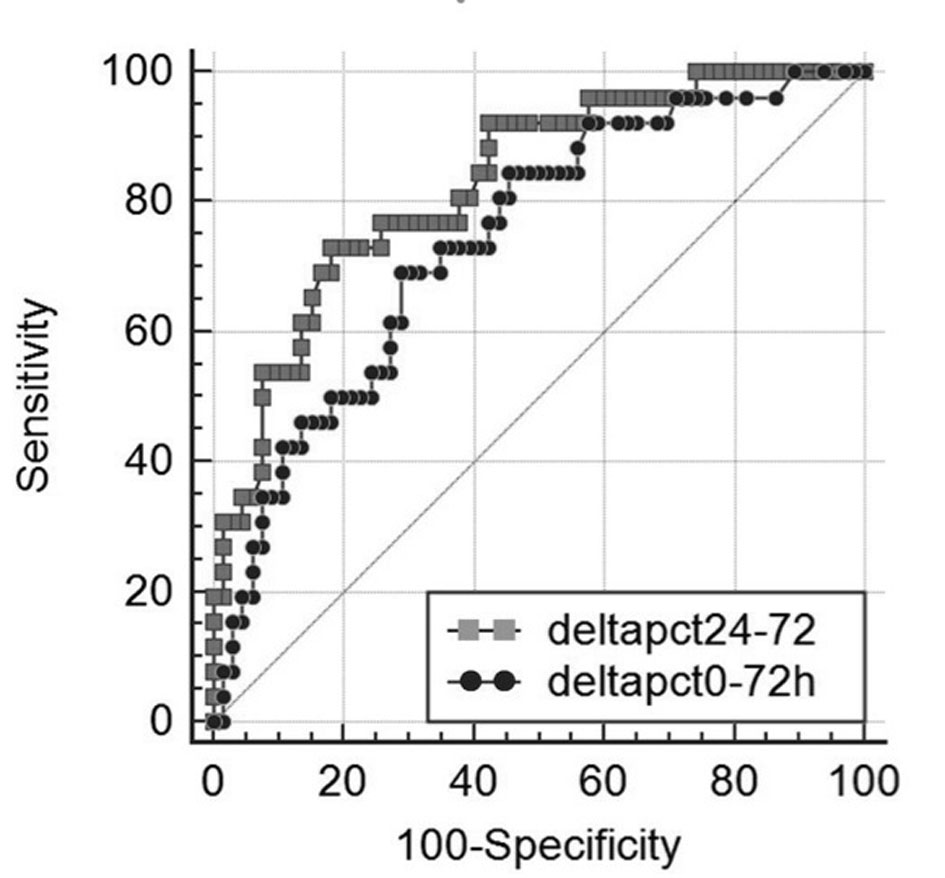
Figure 1. Receiver operating characteristic (ROC) curves of Δ-PCT% variation between day 0 and 72 h (black dotted line) and between 24 and 72 h (grey dotted line) for differentiating between 30-day survivors and non-survivors in 144 patients with severe sepsis syndromes, area under the ROC curve = 0.743 (0.055) for and 0.83 (0.046) (mean (standard deviation)), respectively (P = 0.052).
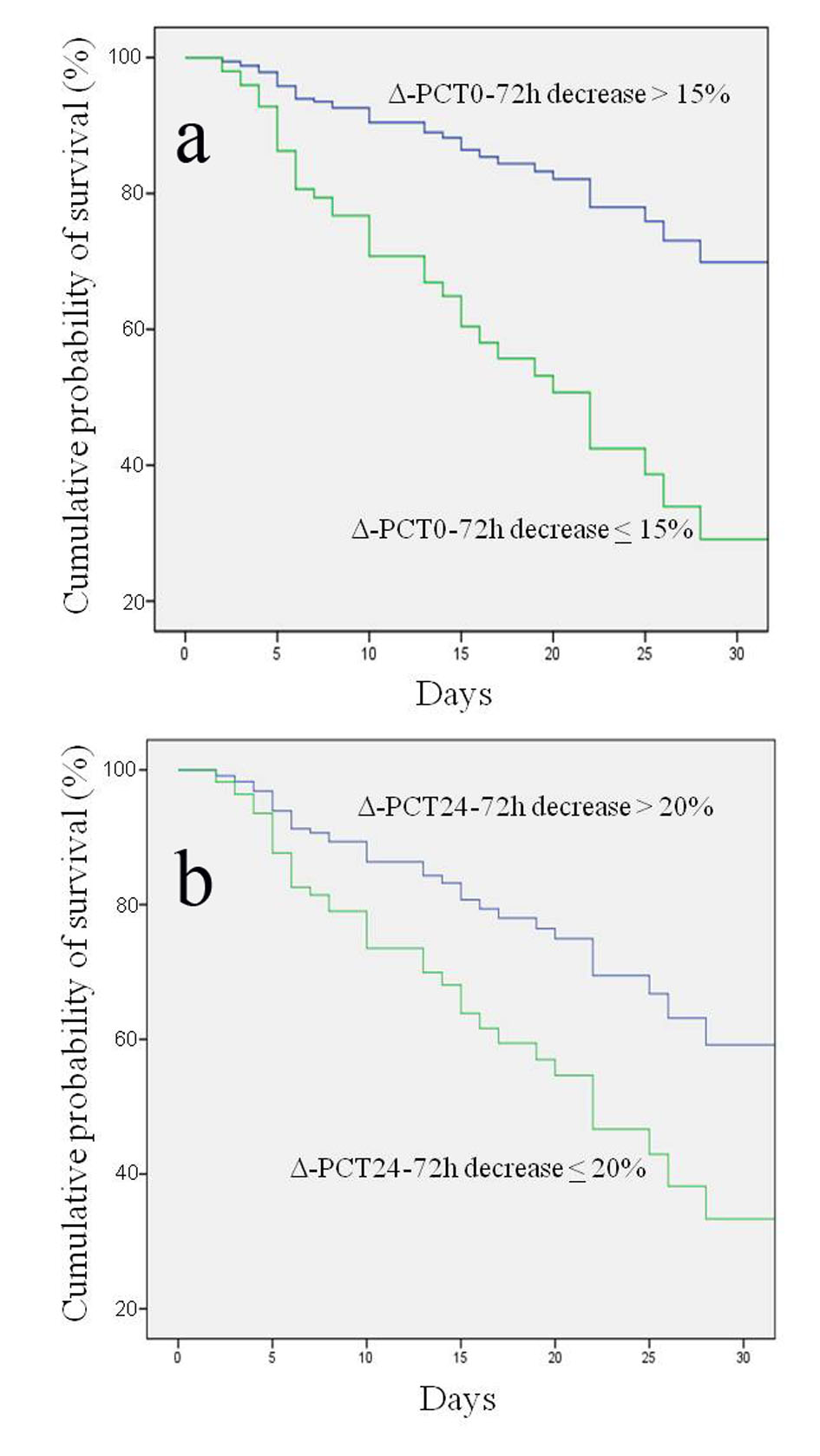
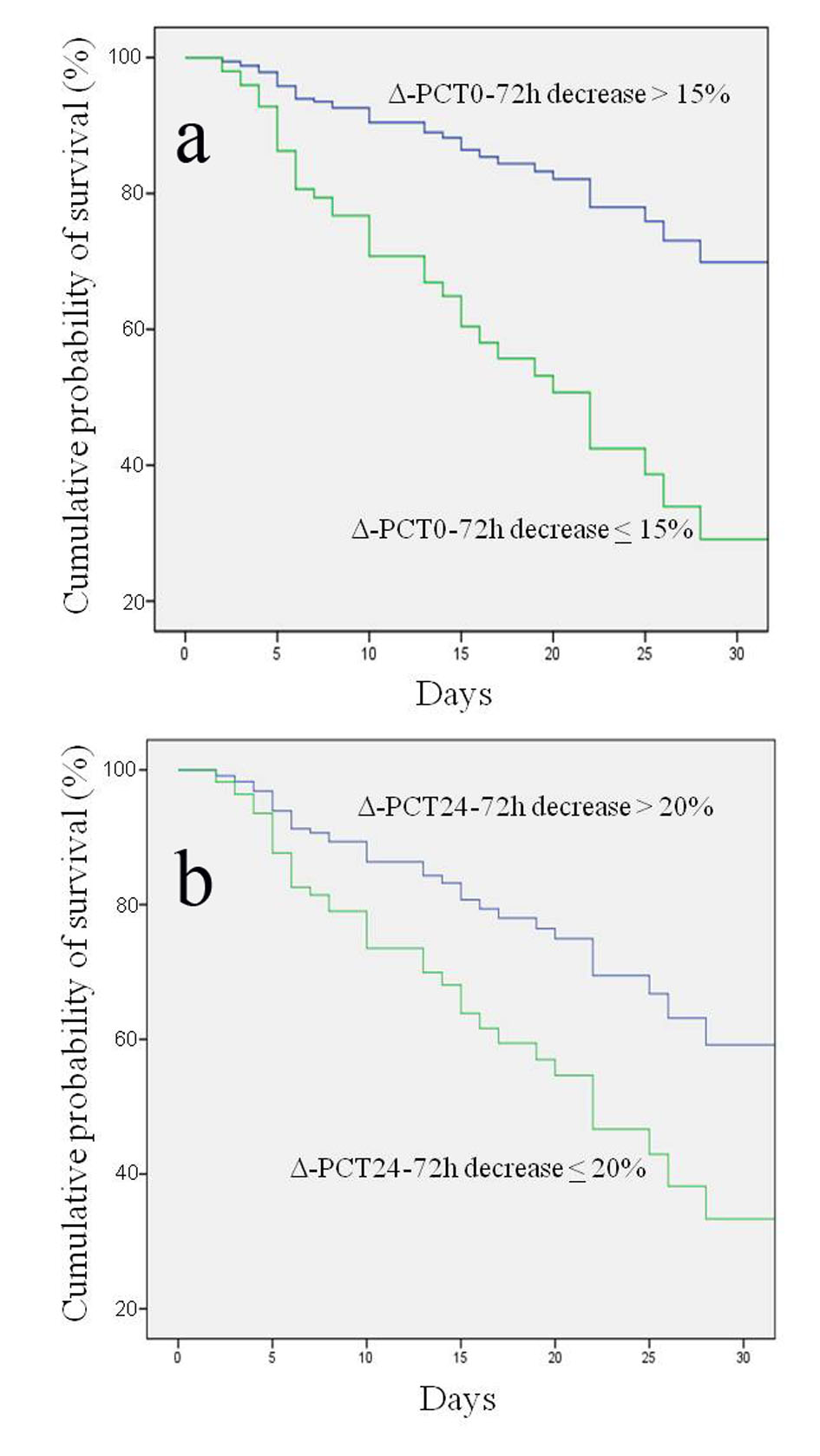
Figure 2. Kaplan-Meier estimation of probability of survival curves for different procalcitonin percentage variations (Δ-PCT) at different time intervals. (a) Δ-PCT percentage decrease between day 0 and 72 h greater or less than 15% in predicting survival; log rank test P < 0.000; 95% CI: 29.8 - 41.3. (b) Δ-PCT percentage decrease between 24 and 72 h greater or less than 20% in predicting survival; log rank test P < 0.0001; 95% CI: 11.4 - 27.8.