| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 10, Number 4, April 2018, pages 314-320
Using Time-Driven Activity-Based Costing as a Key Component of the Value Platform: A Pilot Analysis of Colonoscopy, Aortic Valve Replacement and Carpal Tunnel Release Procedures
Jacob A. Martina, Christopher R. Mayhewa, Amanda J. Morrisb, Angela M. Baderc, Mitchell H. Tsaia, Richard D. Urmanc, d
aDepartment of Anesthesiology, Larner College of Medicine, University of Vermont, Burlington, VT, USA
bDepartment of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, USA
cDepartment of Anesthesiology, Perioperative and Pain Medicine, Harvard Medical School, Brigham and Women’s Hospital, Boston, MA, USA
dCorresponding Author: Richard D. Urman, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital, Boston, MA 02115, USA
Manuscript submitted December 31, 2017, accepted January 18, 2018
Short title: Time-Driven Activity-Based Costing
doi: https://doi.org/10.14740/jocmr3350w
| Abstract | ▴Top |
Background: Time-driven activity-based costing (TDABC) is a methodology that calculates the costs of healthcare resources consumed as a patient moves along a care process. Limited data exist on the application of TDABC from the perspective of an anesthesia provider. We describe the use of TDABC, a bottom-up costing strategy and financial outcomes for three different medical-surgical procedures.
Methods: In each case, a multi-disciplinary team created process maps describing the care delivery cycle for a patient encounter using the TDABC methodology. Each step in a process map delineated an activity required for delivery of patient care. The resources (personnel, equipment and supplies) associated with each step were identified. A per minute cost for each resource expended was generated, known as the capacity cost rate, and multiplied by its time requirement. The total cost for an episode of care was obtained by adding the cost of each individual resource consumed as the patient moved along a clinical pathway.
Results: We built process maps for colonoscopy in the gastroenterology suite, calculated costs of an aortic valve replacement by comparing surgical aortic valve replacement (SAVR) versus transcatheter aortic valve replacement (TAVR) techniques, and determined the cost of carpal tunnel release in an operating room versus an ambulatory procedure room.
Conclusions: TDABC is central to the value-based healthcare platform. Application of TDABC provides a framework to identify process improvements for health care delivery. The first case demonstrates cost-savings and improved wait times by shifting some of the colonoscopies scheduled with an anesthesiologist from the main hospital to the ambulatory facility. In the second case, we show that the deployment of an aortic valve via the transcatheter route front loads the costs compared to traditional, surgical replacement. The last case demonstrates significant cost savings to the healthcare system associated with re-organization of staff required to execute a carpal tunnel release.
Keywords: Costs; Value; Carpal tunnel release; TDABC; TAVR; Colonoscopy
| Introduction | ▴Top |
The high level of spending on healthcare in the United States has been the subject of increasing scrutiny for quite some time. According to the Organization for Economic Co-operation and Development (OECD), an international economic group of 34 member nations, the United States spent 16.9% of its gross domestic product (GDP) on healthcare in 2015, approximately one and a half times more than the next highest country and nearly twice the OECD average [1]. The realization that growth in health care spending in the US has outpaced growth in population, inflation and GDP has intensified the concern of the federal government, healthcare consumers, providers, and payers. While it is true that an investment of such magnitude may reflect public priority, few would argue that this growth in healthcare spending is sustainable.
Central to the problem of escalating health care expenditure is the lack of understanding of how much it costs to deliver patient care. Indeed, most administrators and providers have a managerial accounting understanding of what the cost to the institution or the patient is for medications, reusables, disposables and staffing necessary for a given procedure. In order to transform the American healthcare delivery system, all participants, including patients, physicians, employers, insurance companies, and the government need to recognize that value should be defined as “a given health outcome per dollar of cost expended” [2]. The underlying foundation of this value-based framework is time-driven activity-based costing (TDABC) [3], a methodology that calculates the costs of resources consumed as a patient moves along a care process. Here, we explore the application of TDABC from the perspective of an anesthesiologist.
In fact, at the American Society of Anesthesiologists Annual Meeting in 2016, keynote speaker Michael Porter, a Harvard Business School professor laid out a framework that could transform the health care system in America [4] (Fig. 1). Further, he noted that implementation would require the measurement of clinical outcomes and the associated health care costs beyond the patient-physician encounter. For instance, for patients with osteoarthritis of a hip joint, the value-based framework extends beyond the actual surgical replacement of a patient’s hip and whether or not the anesthesiologist administered an antibiotic at the appropriate time interval.
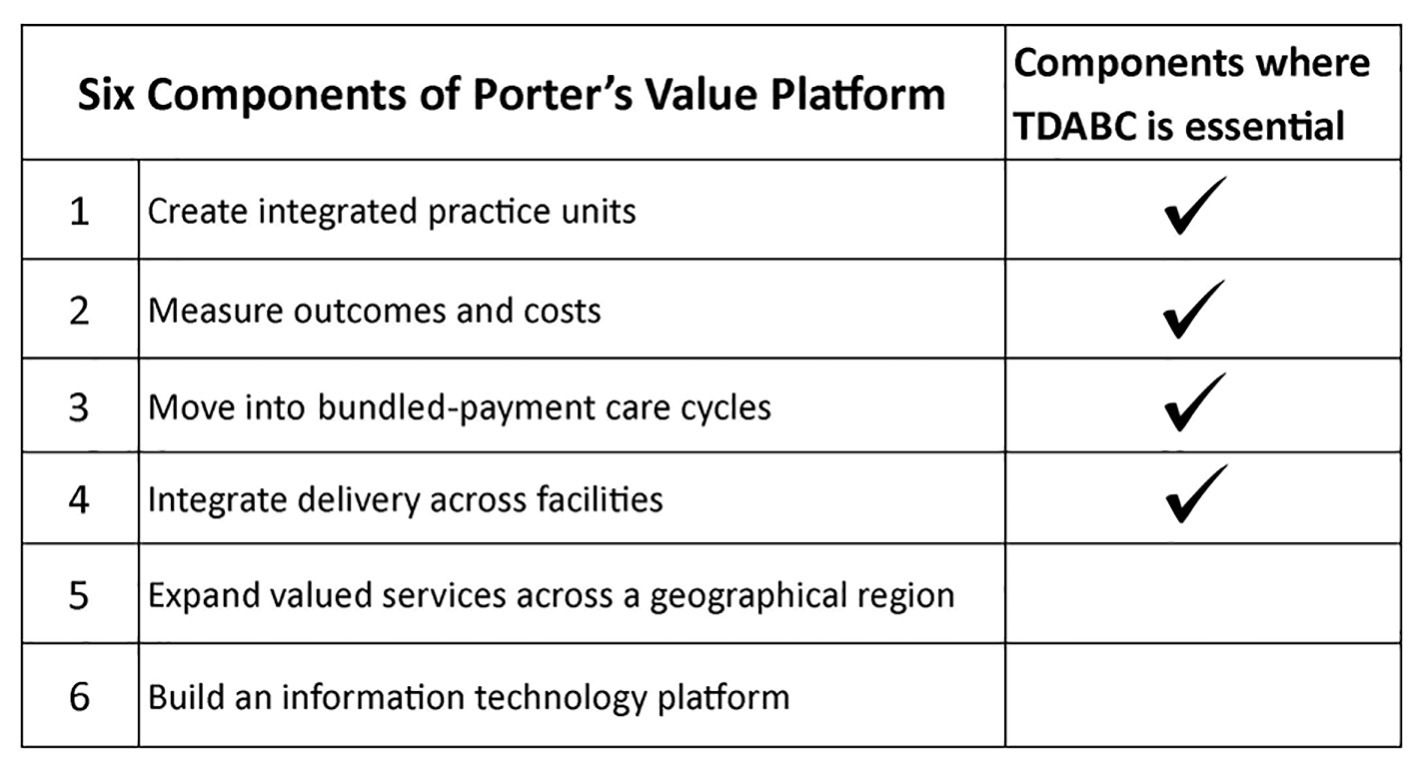 Click for large image | Figure 1. The six components of Michael Porter’s value platform delivered at the American Society of Anesthesiologists Annual Meeting in 2016. TDABC is essential to creating integrated practice units, measuring costs and outcomes, moving into bundled payment care cycles and integrating delivery across facilities. TDABC: time-driven activity-based costing. |
The majority of healthcare systems employ either a “top-down” or less commonly “bottom-up” approach to cost accounting. Top-down approaches use a predetermined metric (e.g. relative value units (RVUs)) to assign the total costs of a healthcare system to its individual services. Bottom-up costing tallies the resources used to produce an individual activity or service and aggregates costs for a clinical pathway in a healthcare system [5]. Bottom-up costing may be more accurate because it identifies individual cost contributors and accounts for indirect costs required to support patient care [6]. In this pilot study, we describe the use of bottom-up costing, specifically the TDABC methodology and financial outcomes for three different medical-surgical procedures.
| Materials and Methods | ▴Top |
Central to the value-based platform is the concept of TDABC initially described by Kaplan [3]. TDABC is a bottom-up costing methodology that calculates the costs of resources consumed as a patient moves along a care process. A multi-disciplinary team creates process maps which describe the care delivery cycle for a patient encounter. Each step in a process map delineates an activity required for the delivery of patient care. The resources (personnel, equipment and supplies) associated with each step are identified. A per minute cost for each resource expended is generated, which is known as the capacity cost rate [7] and multiplied by its time requirement. The total cost for an episode of care is obtained by adding the cost of each individual resource consumed as the patient moves along a clinical pathway. The result is a transparent picture of all expenses incurred during a patient care episode.
The University of Vermont Medical Center (UVMMC) uses a “top-down”, RVU-based methodology where costs of producing services are grouped into categories related to billable events. The RVU method was established at the national level to approximate the relative work and expertise required to deliver a patient service. The American Medical Association generates RVUs for each current procedural terminology (CPT) code. CPT codes exist for any interaction between a patient and healthcare provider. RVUs are modified by the level of service, practice expenses, malpractice insurance costs and geographic location. Reimbursement for services rendered by the Centers for Medicare and Medicaid (CMS) are based on the CPT codes generated and their associated RVUs.
UVMMC generates a charge master for each episode of care which identifies all billable items. Certain costs not identified in this system include the fixed costs of wages, rents and administration, as well as commonly used supplies. These indirect costs are estimated and divided among departments, providing treatment associated with an episode of care. Each unit of service and its associated costs (direct and indirect) for a billable episode are summed to determine the total cost of a patient encounter.
| Results | ▴Top |
The results of three different pilot studies are described below. These include building process maps for colonoscopy in the gastroenterology suite, calculating costs of replacing an aortic valve by comparing surgical aortic valve replacement (SAVR) versus transcatheter aortic valve replacement (TAVR) techniques, and determining the cost of carpal tunnel release (CTR) in an operating room (OR) versus a procedure room.
Case 1: Building process maps for colonoscopy
There is a growing demand for anesthesia service use to help facilitate gastroenterology procedures [8, 9]. At the Brigham and Women’s Hospital, Morris et al [10] used TDABC to elucidate the causes of long patient waiting times for a colonoscopy procedure, to understand scheduling and triage processes, and to reallocate clinical resources. Prior to implementation of a redesigned process, patient waiting times for a colonoscopy with anesthesiologist-administered sedation was 14 days at the ambulatory facility and up to 3 months at the main hospital. Using the TDABC model, the authors created detailed process maps encompassing the primary care physician referral (Fig. 2), scheduling, the preoperative clinic visit, the procedure check-in, the procedure itself, and recovery and discharge. The authors entered the costs of staff, equipment, and consumables into their TDABC model.
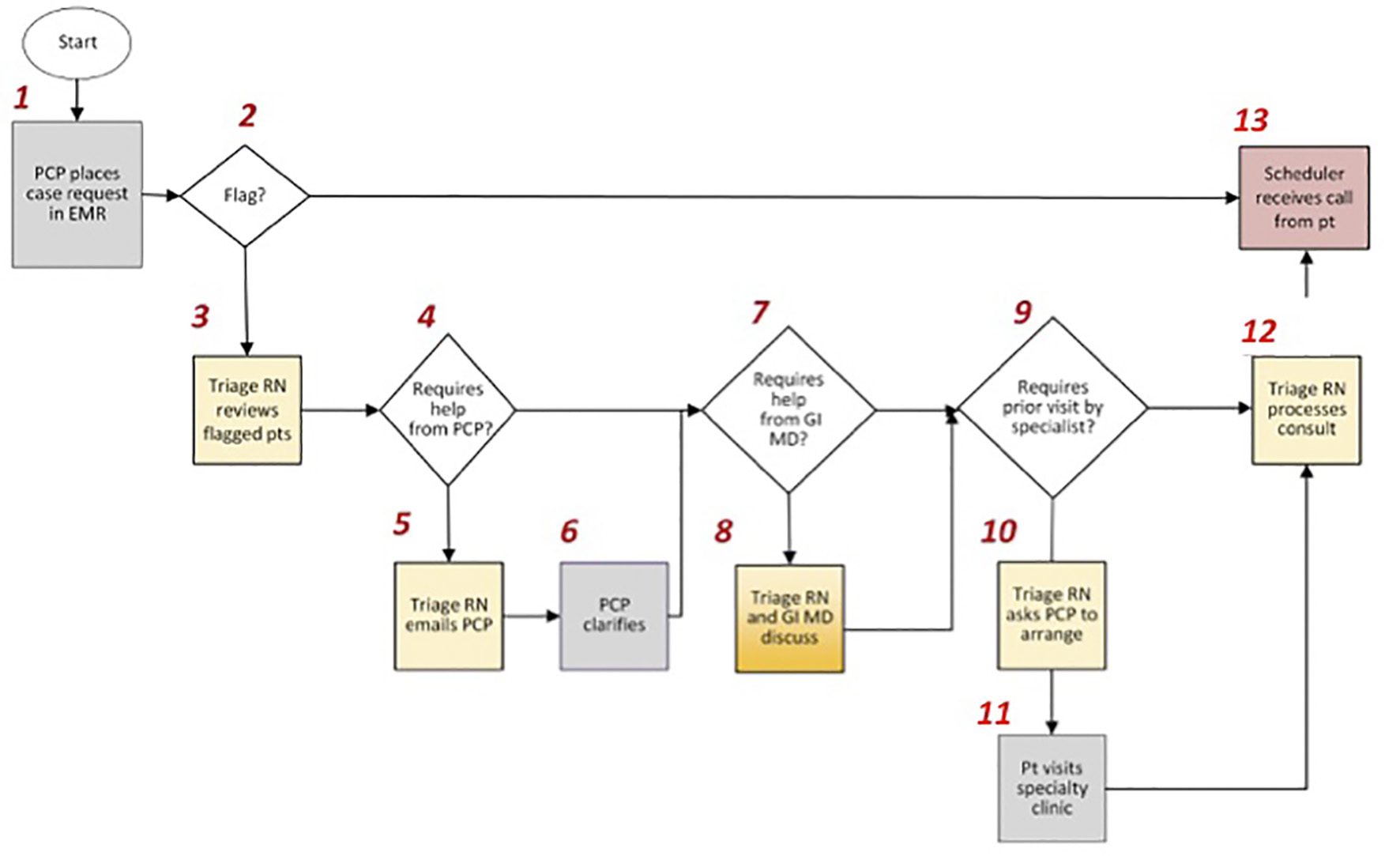 Click for large image | Figure 2. Referral process for patients requiring a gastroenterology procedure at Brigham and Women’s Hospital. After a request is made by the patient’s primary care provider, it is determined whether or not the patient’s medical history includes any of the following flag criteria: anticoagulation, pacemaker or defibrillator, cardiac disease, supplemental oxygen, obstructive sleep apnea, body mass index > 40, renal disease, insulin dependent diabetes mellitus, difficulty with sedation, airway issues, and chronic opioid use. Those patients not meeting flag criteria are eligible to bypass the pre-operative evaluation clinic and proceed to scheduling at the ambulatory facility. PCP: primary care provider; EMR: electronic medical record; RN: registered nurse; pts: patients; GI: gastrointestinal; MD: Medical Doctor. |
The study investigators discovered that patients who were scheduled in the ambulatory facility were most often seen by the anesthesiologist on the day of the procedure. By contrast, a majority of patients (95%) scheduled at the main hospital were seen in the preoperative evaluation clinic, accounting for 79% of pre-procedure costs in this patient group. Further, many of these patients did not meet flag criteria necessitating a preoperative evaluation and could be scheduled at the ambulatory facility rather than the main hospital. Historically, patients with significant co-morbidities were scheduled at the main hospital and required an evaluation in the preoperative assessment clinic prior to the procedure. The application of TDABC helped reveal the opportunity to decrease operating costs in the preoperative evaluation clinic and procedure wait times by shifting more volume to the ambulatory facility. In fact, shifting 50-75% of colonoscopy volume from the hospital to the ambulatory facility could produce annual savings of $68,000 or $102,000, respectively, and reduce the wait times from 3 months to 6 or 3 weeks, respectively.
Depending on the reimbursement model used, this cost savings to healthcare consumers and payers may not be passed on to the institution or care providers. In the current fee for service system, it is common for facility fees and therefore reimbursement to be highest at the main hospital campus. Fortunately for Brigham and Women’s Hospital, there was no difference in facility fees between the two sites allowing them to capture the additional savings. As CMS rolls out the bundled payment care initiative, compensation will be determined primarily by the quality of care administered, providing incentive for those institutions implementing efficiencies. Using TDABC, this multidisciplinary effort involving proceduralists, hospital administrators, nurses and anesthesiologists demonstrated how to streamline operational processes, decrease overall costs, and improve patient access to care.
Case 2: What are the costs of replacing an aortic valve? A comparison of SAVR versus TAVR techniques
TAVR is a minimally invasive modality, initially developed to treat high risk patients with severe symptomatic aortic stenosis. Continuous improvement in technology and the development of regional and institutional expertise has expanded the use of TAVR to include patients who are at high and intermediate risk for SAVR [11, 12]. TAVR has been shown to be equivalent to SAVR with respect to mortality and symptom reduction at 2 years [13]. Assuming this trend continues, the avoidance of a sternotomy associated with a TAVR clearly makes it the procedure of choice for most patients.
As the scientific community awaits the results of long-term outcomes, it may be prudent to consider the cost associated with each procedure. Osnabrugge et al [14] compared the costs of TAVR and SAVR in intermediate risk patients, but did not elaborate on the methods employed to determine the personnel costs. Reynolds et al [15] calculated the cost effectiveness of TAVR versus SAVR and found that the initial additional cost to deploy a valve via the transcatheter approach ($24,000) was greatly reduced at 1 year ($9,000). Avoidance of a short-term rehabilitation stay for some TAVR recipients accounted for most of the cost reduction over time.
At UVMMC, we used TDABC to compare the costs associated with a surgical versus a transcatheter approach for aortic valve replacements. In the model, we accounted for all the personnel staffing and supply costs for the TAVR and SAVR procedures. The model considered the following key variables: 1) the cost per clinical hour for each staff member, 2) the amount of time required of each staff member, 3) the number of staff members present during the procedure, 4) the cost for each supply used, and 5) the quantity of supplies used. Costing data are shown in Table 1. The total cost of deploying a transcatheter aortic valve was $38,250. Personnel and durable costs associated with the TAVR procedure totaled $2,831 and $35,419, respectively. In fact, the single largest contributor was the transcatheter valve itself, costing $32,000 and representing 83.7% of the total procedural costs. By comparison, the total cost of SAVR was $11,147. Personnel costs associated with SAVR totaled $2,473. The cost of supplies, including sterilization of reusable items and disposables totaled $8,674. The cost of the surgical bioprosthetic aortic valve was $5,600, representing 50.2% of the total procedural costs. As technology improves, heart team staffing is streamlined and efficiencies are implemented, it will be interesting to see if the cost difference between SAVR and TAVR becomes insignificant, further justifying the initial investment required for the transcatheter approach.
 Click to view | Table 1. Cost per Case for SAVR and TAVR |
Case 3: The cost of CTR in an OR versus a procedure room
CTR is a common procedure performed over 400,000 times per year in the United States. Open CTR can be performed in an OR or an outpatient procedure room with considerable differences in time, labor and supplies for each setting. Once again, at UVMMC, we developed a TDABC model which considered the following key variables: 1) the cost per clinical hour for each staff member, 2) the amount of time required of each staff member, 3) the number of staff members present during the procedure, 4) the cost for each supply used, and 5) the quantity of supplies used. Time and supply costs were determined using one orthopedic surgeon’s CTR cases in 2015. Costing data are shown in Table 2. A total of 91 cases were performed in the OR, while 51 cases were performed in the outpatient procedure room. The cost of performing CTR in the OR was $564 per case compared to $386 per case in the procedure room, representing an absolute cost difference of $178. Labor costs were $386 in the OR compared to $208 in the procedure room, while supply costs were $178 in both settings. The average time required to perform CTR in the OR was 52:30 min versus 48:06 min in the procedure room. Using a TDABC model, we found that open CTR performed in the procedure room costs 31.6% less per case than open CTR in the OR. This did not include the additional savings generated by bypassing a pre-operative assessment, a pre-operative admission and a post-operative recovery stay. A recent Canadian study found that the use of the procedure room was more than twice as time efficient and cost 73.4% less per CTR case than the OR [16]. Patients undergoing CTR in the procedure room have similar postoperative pain control, satisfaction scores and the same incidence of deep and superficial wound infection complications [17, 18]. In this case study, it should be noted that the potential effects on reimbursement to providers or the institution based on staff deployed and procedure location were not considered. However, based on our analysis and the findings of others [19], open CTR provides superior value when performed in an outpatient procedure room setting.
 Click to view | Table 2. Cost per Case for Carpal Tunnel Release (CTR) in the OR and the Procedure Room |
| Discussion | ▴Top |
In this pilot study, we describe successful use of TDABC methodology, a bottom-up costing approach to compare the costs of three different medical-surgical procedures: colonoscopy, aortic valve replacement and CTR. The application of TDABC provides a framework to identify process improvements for health care delivery. The first case demonstrates cost-savings and improved wait times by shifting some of colonoscopies scheduled with an anesthesiologist from the main hospital to the ambulatory facility. In the second case, we show that the deployment of an aortic valve via the transcatheter route front loads the costs compared to traditional, surgical replacement. The last case demonstrates significant cost savings to the healthcare system associated with re-organization of staff required to execute a CTR.
At present, a majority of hospitals continue to employ top-down costing methodologies because of the simplistic format, ease of data input and less labor-intensive accounting. Disadvantages to top-down costing strategies include an inability to anticipate how a change in practice affects cost, a failure to identify all cost contributors, and the misalignment of cost with health care reimbursement. Specifically, cost (the expense incurred to provide a particular service) may have a weak correlation with reimbursement (the payment received for services rendered). Ultimately, the lack of transparent costing systems encourages healthcare institutions to average effects across health care services, undermine collegiality among providers, and cloud the ability to identify bottlenecks and implement efficiencies.
TDABC coupled with the analysis of process maps identifies rate-limiting steps, reduces redundancy, and ensures that all the employees work within the maximum scope of their practice and degree. Further, it facilitates the redesign of care pathways and is essential to four of the six components identified in Porter’s value platform (Fig. 1). The applications of TDABC have been readily shown outside the traditional OR. Recently, Haas et al [20] demonstrated that expanding a nephrology clinic visit from 10 to 30 min allowed additional time to counsel end-stage renal disease (ESRD) patients transitioning to dialysis. These patients were much more likely to undergo arteriovenous fistula creation and avoid initiating dialysis via a centrally accessed catheter. The cost of the additional 20 min to the institution was $200; however, the total cost savings per patient totaled $200,000. This simple re-allocation of physician time improved patient education and management of ESRD, minimized potential complications and resulted in significant cost savings.
Admittedly, there is no “gold standard” or validated tool for measuring value in healthcare. From an economic perspective, the value of a good or service to an individual is equal to what that person would be willing to pay for it or give up in terms of time or resources to receive it. Health care in the United States is executed through a complex set of interrelationships between three distinct parties: payers, providers and consumers (i.e. patients). Despite their different frames of reference, all three components of our health care system are likely to gain when value is considered while deciding where and how to best utilize resources for the purpose of health [19].
Institutions implementing the TDABC methodology are likely to encounter some challenges. It requires an extensive information technology platform that can be expensive to install and maintain. It generates vast amounts of data which require a significant time investment to analyze. Finally, there may be some resistance at the institutional or provider level to implementing a costing methodology that is completely transparent. Given these challenges, institutions are likely to benefit from a focused roll out, targeting small pathway-oriented procedures from a particular service line. For example, Cleveland Clinic’s cardiac surgery team implemented TDABC with mixed results, finding small but significant differences in cost calculations compared to RVU costing [21]. In addition, TDABC has been applied to pediatric appendectomies and the pre-operative assessment process, demonstrating reduced cost in each setting without affecting outcomes, thereby increasing value [22, 23].
The application of TDABC to a patient care episode identifies rate-limiting steps, minimizes redundancy, and may generate cost savings. These cost savings are a direct result of improved efficiency and the alignment of provider skill set with a given task. Health care institutions, government, and insurance companies should view these costs savings as an opportunity to reinvest in current health care processes. Until the cost savings are shared—thus providing incentive for healthcare institutions and providers to implement TDABC—it is less likely to attain widespread adoption as a costing methodology.
Conclusions
As the healthcare systems in this country transition toward a bundled payment system, anesthesiologists need to appreciate this fundamental shift. Under the new paradigm, financial risk moves from the payer side to those providers and institutions delivering care. TDABC, by establishing a capacity cost rate for each resource consumed in a care process provides a blueprint to assist providers in making cost-conscious decisions and implement efficiencies. At the institutional level, it facilitates the analysis of alternative treatments and provides transparency required for further cost reduction. A multi-disciplinary, value-based care framework incorporating TDABC provides anesthesiologists and practice managers the tools to demonstrate “value” at the institutional level and beyond.
Conflict of Interest
The author(s) declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Funding
There was no funding for the work completed at the University of Vermont. The work performed at Brigham and Women’s Hospital was supported by the BWH President’s Award and Harvard Business School.
| References | ▴Top |
- Organization for economic co-operation and development. OECD. Stat: Health Status. http://stats.oecd.org/Index.aspx?DatasetCode=HEALTH_STAT. Accessed June 19, 2017. Updated June 30, 2017.
- Porter ME. A strategy for health care reform—toward a value-based system. N Engl J Med. 2009;361(2):109-112.
doi pubmed - Kaplan RS, Anderson SR. Time-driven activity-based costing: a simpler and more powerful path to higher profits. Boston, MA: Harvard Business School Publishing; 2007.
- Harvard Business School. Porter, ME. Value-based healthcare delivery: an agenda for transforming anesthesiology. American society of Anesthesiologists Annual Meeting, October 22, 2016.
- Chapko MK, Liu CF, Perkins M, Li YF, Fortney JC, Maciejewski ML. Equivalence of two healthcare costing methods: bottom-up and top-down. Health Econ. 2009;18(10):1188-1201.
doi pubmed - Berlin MF, Smith TH. Evaluation of activity-based costing versus resource-based relative value costing. J Med Pract Manage. 2004;19(4):219-227.
pubmed - Najjar PA, Strickland M, Kaplan RS. Time-driven activity-based costing for surgical episodes. JAMA Surg. 2017;152(1):96-97.
doi pubmed - Predmore Z, Nie X, Main R, Mattke S, Liu H. Anesthesia service use during outpatient gastroenterology procedures continued to increase from 2010 to 2013 and potentially discretionary spending remained high. Am J Gastroenterol. 2017;112(2):297-302.
doi pubmed - Nagrebetsky A, Gabriel RA, Dutton RP, Urman RD. Growth of nonoperating room anesthesia care in the United States: a contemporary trends analysis. Anesth Analg. 2017 Apr;124(4):1261-1267.
doi pubmed - Morris AJ, Feng AY, Nayor J, et al. How a tertiary care academic endoscopy center used time-driven activity-based costing to improve value. NEJM Catalyst. 2017.
- Piazza N, Kalesan B, van Mieghem N, Head S, Wenaweser P, Carrel TP, Bleiziffer S, et al. A 3-center comparison of 1-year mortality outcomes between transcatheter aortic valve implantation and surgical aortic valve replacement on the basis of propensity score matching among intermediate-risk surgical patients. JACC Cardiovasc Interv. 2013;6(5):443-451.
doi pubmed - Wenaweser P, Stortecky S, Schwander S, Heg D, Huber C, Pilgrim T, Gloekler S, et al. Clinical outcomes of patients with estimated low or intermediate surgical risk undergoing transcatheter aortic valve implantation. Eur Heart J. 2013;34(25):1894-1905.
doi pubmed - Kodali SK, Williams MR, Smith CR, Svensson LG, Webb JG, Makkar RR, Fontana GP, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366(18):1686-1695.
doi pubmed - Osnabrugge RL, Head SJ, Genders TS, Van Mieghem NM, De Jaegere PP, van der Boon RM, Kerkvliet JM, et al. Costs of transcatheter versus surgical aortic valve replacement in intermediate-risk patients. Ann Thorac Surg. 2012;94(6):1954-1960.
doi pubmed - Reynolds MR, Lei Y, Wang K, Chinnakondepalli K, Vilain KA, Magnuson EA, Galper BZ, et al. Cost-effectiveness of transcatheter aortic valve replacement with a self-expanding prosthesis versus surgical aortic valve replacement. J Am Coll Cardiol. 2016;67(1):29-38.
doi pubmed - Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2(4):173-178.
doi pubmed - Davison PG, Cobb T, Lalonde DH. The patient’s perspective on carpal tunnel surgery related to the type of anesthesia: a prospective cohort study. Hand (N Y). 2013;8(1):47-53.
doi pubmed - Leblanc MR, Lalonde DH, Thoma A, Bell M, Wells N, Allen M, Chang P, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2011;6(1):60-63.
doi pubmed - Gray ML. Gender, race, and culture in research on UI: sensitivity and screening are integral to adequate patient care. Am J Nurs. 2003;(Suppl):20-25.
doi pubmed - Haas DA, Krosner YC, Mukerji N, et al. Delivering higher value care means spending more time with patients. Harvard Business Review. https://hbr.org/2014/12/delivering-higher-value-care-means-spending-more-time-with-patients. Published December 26, 2014.
- Donovan CJ, Hopkins M, Kimmel BM, Koberna S, Montie CA. How Cleveland Clinic used TDABC to improve value. Healthc Financ Manage. 2014;68(6):84-88.
pubmed - French KE, Albright HW, Frenzel JC, Incalcaterra JR, Rubio AC, Jones JF, Feeley TW. Measuring the value of process improvement initiatives in a preoperative assessment center using time-driven activity-based costing. Healthc (Amst). 2013;1(3-4):136-142.
doi pubmed - Yu YR, Abbas PI, Smith CM, Carberry KE, Ren H, Patel B, Nuchtern JG, et al. Time-driven activity-based costing to identify opportunities for cost reduction in pediatric appendectomy. J Pediatr Surg. 2016;51(12):1962-1966.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











