| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website http://www.jocmr.org |
Original Article
Volume 7, Number 1, January 2015, pages 41-44
Hyaluronic Acid Concentration in Pleural Fluid: Diagnostic Aid for Tuberculous Pleurisy
Yusuke Yoshinoa, b, Yoshitaka Wakabayashia, Kazunori Seoa, Ichiro Kogaa, Takatoshi Kitazawaa, Yasuo Otaa
aDepartment of Internal Medicine, Teikyo University School of Medicine, 2-11-1 Kaga, Itabashi-ku, Tokyo 173-8606, Japan
bCorresponding Author: Yusuke Yoshino, Department of Internal Medicine, Teikyo University School of Medicine, 2-11-1 Kaga, Itabashi-ku, Tokyo 173-8606, Japan
Manuscript accepted for publication September 22, 2014
Short title: Hyaluronic Acid to Diagnose Tuberculous Pleurisy
doi: http://dx.doi.org/10.14740/jocmr1980w
| Abstract | ▴Top |
Background: A high concentration of hyaluronic acid in pleural fluid is suggestive of malignant mesothelioma. However, a relatively high concentration of hyaluronic acid was also seen in the pleural fluid of patients with benign inflammatory diseases. To show the utility of measuring hyaluronic acid levels in pleural fluid to diagnose tuberculous pleurisy, we compared the clinical features and levels of hyaluronic acid in the pleural fluid of patients with and without tuberculous pleurisy.
Methods: We enrolled 27 patients with infective pleurisy admitted at Teikyo University Hospital from January 2010 to December 2013. Ten patients were diagnosed with tuberculous pleurisy, and 17 with non-tuberculous pleurisy. We reviewed the clinical features and data of all 27 patients and compared the two groups. We analyzed and compared the concentration of hyaluronic acid and adenosine deaminase in their pleural fluid.
Results: Patients with tuberculous pleurisy tended to have significantly higher concentrations of hyaluronic acid and adenosine deaminase in their pleural fluid (tuberculous pleurisy patients vs. other infective pleurisy patients: hyaluronic acid (× 103 ng/mL); 42.9 ± 23.3 vs. 16.8 ± 17.9, P = 0.003, adenosine deaminase (IU/L); 89.7 ± 33.3 vs. 74.0 ± 90.9, P = 0.032). Receiver operating characteristic analysis revealed no significant difference in the area under the curve of hyaluronic acid and adenosine deaminase volumes in pleural fluid, suggesting their equivalent value as major diagnostic tools for tuberculosis pleurisy.
Conclusions: Hyaluronic acid concentration in pleural fluid can be a valuable tool for the diagnosis of tuberculous pleurisy.
Keywords: Hyaluronic acid; Adenosine deaminase; Tuberculosis pleurisy; Diagnostic aid
| Introduction | ▴Top |
Hyaluronic acid is an anionic, non-sulfated glycosaminoglycan distributed widely throughout connective, epithelial, and neural tissues [1]. In pleural fluid, it appears to decrease the friction between the lung and the thoracic cavity [1].
A high concentration of hyaluronic acid (> 100 µg/mL) in pleural fluid is suggestive of malignant mesothelioma [2]. In addition, a previous study showed a relatively high concentration of hyaluronic acid in the pleural fluid of patients with benign inflammatory diseases, such as rheumatoid arthritis and complicated parapneumonic effusion [3, 4]. Hyaluronic acid in pleural fluid was suggested to contribute to the early identification of complicated parapneumonic effusion [4].
Tuberculous pleurisy is one of the major manifestations of a tuberculosis infection. It is difficult to diagnose because the positive culture rate for tuberculosis in pleural fluid is usually low [5]. Therefore, measuring adenosine deaminase in pleural fluid is currently the most valuable tool for its diagnosis.
In this study, we analyzed the volume of hyaluronic acid in pleural fluid in patients of tuberculous pleurisy, to determine whether hyaluronic acid can aid in the diagnosis of tuberculous pleurisy.
| Methods | ▴Top |
Study population
In all, 133 patients (> 18 years) with infective pleurisy that were enrolled for the study were admitted to the Teikyo University Hospital, a 1,200-bed teaching hospital in Tokyo, Japan, from January 2010 to December 2013.
Case definition and inclusion/exclusion criteria
Infective pleurisy was diagnosed on the basis of a positive result on culture of pleural fluid and signs and symptoms of pleurisy, such as pleural fluid, fever, chest pain, cough, fatigue, disorientation, hypotension, and respiratory failure.
Patients whose pleural fluid was collected for the analysis of adenosine deaminase, lactate dehydrogenase, and hyaluronic acid were included. In contrast, patients who had a history of respiratory malignancy and rheumatoid arthritis were excluded because previous reports have shown that respiratory malignancy including malignant mesothelioma could increase hyaluronic acid in pleural fluid [2].
Endpoint
The endpoint of this study was to show whether hyaluronic acid in pleural fluid was significantly increased in patients with tuberculous pleurisy. In order to assess the diagnostic value of hyaluronic acid concentration in pleural fluid, it was compared with the level of adenosine deaminase.
Statistical analysis
The results are expressed as mean with standard deviation unless otherwise indicated. For univariate analysis, Student’s t-test and Fisher’s exact test were used to analyze continuous and categorical data where appropriate.
To assess and compare the diagnostic accuracy of hyaluronic acid and adenosine deaminase for discriminating patients with pleurisy from those with tuberculous pleurisy, we plotted receiver operating characteristic (ROC) curves and calculated the areas under the curves (AUC) for comparison. ROC curves were generated by plotting the relationship of the true positivity (sensitivity) and the false positivity (1 - specificity) at various cut-off points in the tests.
All P-values were two-sided, and were considered statistically significant at a value of < 0.05.
Ethics
The Ethics Committee of the University of Teikyo approved this project.
| Results | ▴Top |
Only 33 of 133 met the inclusion criteria. Of them, six patients had histories of respiratory malignant diseases and were excluded. Twenty-seven patients were eventually analyzed: 10 had tuberculous pleurisy and 17 had non-tuberculous infective pleurisy.
We summarized demographic data, clinical features, and pleural fluid laboratory data of all 27 patients in Table 1. There were significant differences in age and levels of hyaluronic acid, and adenosine deaminase in pleural fluid between the two groups.
| Table 1. Clinical Data for Pleurisy Patients Included in the Study Population |
There were no significant differences in AUC between the two groups (Fig. 1). The optimal cut-offs using the ROC curve were 24,950 ng/mL of hyaluronic acid and 51.9 IU/L of adenosine deaminase respectively (Table 2).
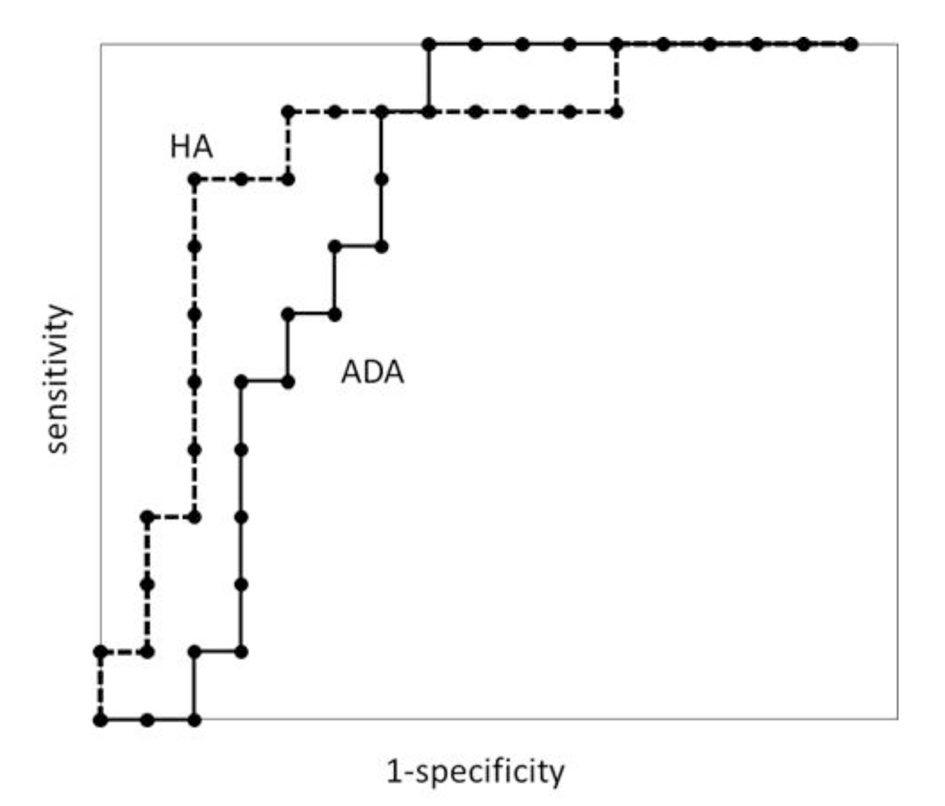 Figure 1. Receiver operating characteristic curves for pleural fluid adenosine deaminase (ADA) and hyaluronic acid (HA) in patients with tuberculous pleurisy. Figure 1. Receiver operating characteristic curves for pleural fluid adenosine deaminase (ADA) and hyaluronic acid (HA) in patients with tuberculous pleurisy. |
| Table 2. The Optimal Cut-Off Level for Hyaluronic Acid and Adenosine Deaminase Concentrations in the Pleural Fluid of Patients With Tuberculous Pleurisy |
| Discussion | ▴Top |
Our study results showed that hyaluronic acid concentration in pleural fluid was significantly increased in patients with tuberculous pleurisy, and that the use of this measurement was non-inferior to that of adenosine deaminase concentration in pleural fluid for the diagnosis of tuberculous pleurisy.
Hyaluronic acid can be produced from alveolar epithelial cells or mesothelial cells following local inflammation [6]. Indeed, a previous report showed that a high concentration of hyaluronic acid was seen in benign inflammatory diseases [2], particularly in those with long-term inflammation such as rheumatoid arthritis and complicated parapneumonic effusion [4]. Normally, tuberculous pleurisy presents with relatively few symptoms; moreover, and there is chronic inflammation [7]. This chronic inflammation may increase the hyaluronic acid concentration in pleural fluid. However, it was extremely difficult to calculate the duration of the inflammation.
Some reports have indicated that the production of hyaluronic acid might be promoted by proinflammatory cytokines such as tumor necrosis factor alpha and interleukin 1 beta [8, 9]. Thus, elevation of these cytokines in the pleural fluid can lead to increased hyaluronic acid concentration in pleural fluid. For example, in patients with complicated parapneumonic effusions, these two cytokines were significantly elevated in pleural fluid as was hyaluronic acid concentration [4]. Tahhan et al also showed that tumor necrosis factor alpha tended to be elevated in cases with tuberculous pleurisy [10], which is probably why, in our study, patients with tuberculous pleurisy had high hyaluronic acid concentrations in pleural fluid. Tahhan et al additionally suggested that tumor necrosis factor alpha level could be used to diagnose tuberculous pleurisy.
Diagnosis of tuberculous pleurisy using pleural fluid is difficult because the positive culture rate of Mycobacterium tuberculosis in pleural fluid is relatively low [5], often necessitating a pleural biopsy. In Japan, however, M. tuberculosis infection is often found in the elderly, in whom performing invasive procedures such as pleural biopsy is difficult; consequently, the measurement of adenosine deaminase concentration in pleural fluid has become a valuable diagnostic tool. Furthermore, some reports have shown that infective pleurisy not associated with tuberculosis, e.g., cryptococcosis and brucellosis pleurisy, could also result in a high concentration of adenosine deaminase in pleural fluid [11, 12]. Therefore, measuring hyaluronic acid in combination with adenosine deaminase in pleural fluid could lead to a more effective diagnosis for tuberculous pleurisy.
The present study has several limitations. First, it was retrospective, single-center study. Second, the sample size was small, because only hospitalized adult patients with infective pleurisy who met the criteria were enrolled. However, the study results demonstrate for the first time that the measurement of hyaluronic acid concentration in pleural fluid might be a diagnostic aid for tuberculous pleurisy. Nevertheless, a larger-scale prospective study is required to confirm our findings.
Conflict of Interest
The authors declare no conflict of interest associated with this manuscript.
| References | ▴Top |
- Fraser JR, Laurent TC, Laurent UB. Hyaluronan: its nature, distribution, functions and turnover. J Intern Med. 1997;242(1):27-33.
doi pubmed - Pettersson T, Froseth B, Riska H, Klockars M. Concentration of hyaluronic acid in pleural fluid as a diagnostic aid for malignant mesothelioma. Chest. 1988;94(5):1037-1039.
doi pubmed - Soderblom T, Pettersson T, Nyberg P, Teppo AM, Linko L, Riska H. High pleural fluid hyaluronan concentrations in rheumatoid arthritis. Eur Respir J. 1999;13(3):519-522.
doi pubmed - Zaga T, Makris D, Tsilioni I, Kiropoulos T, Oikonomidi S, Damianos A, Gourgoulianis KI. Hyaluronic acid levels are increased in complicated parapneumonic pleural effusions. Monaldi Arch Chest Dis. 2011;75(3):167-171.
pubmed - Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med. 2000;161(4 Pt 1):1376-1395.
pubmed - Dentener MA, Vernooy JH, Hendriks S, Wouters EF. Enhanced levels of hyaluronan in lungs of patients with COPD: relationship with lung function and local inflammation. Thorax. 2005;60(2):114-119.
doi pubmed - Morehead RS. Tuberculosis of the pleura. South Med J. 1998;91(7):630-636.
doi pubmed - Davies CW, Gleeson FV, Davies RJ. BTS guidelines for the management of pleural infection. Thorax. 2003;58(Suppl 2):ii18-28.
doi pubmed - Wang PM, Lai-Fook SJ. Pleural tissue hyaluronan produced by postmortem ventilation in rabbits. Lung. 2000;178(1):1-12.
doi pubmed - Tahhan M, Ugurman F, Gozu A, Akkalyoncu B, Samurkasoglu B. Tumour necrosis factor-alpha in comparison to adenosine deaminase in tuberculous pleuritis. Respiration. 2003;70(3):270-274.
doi pubmed - Yoshino Y, Kitazawa T, Tatsuno K, Ota Y, Koike K. Cryptococcal pleuritis containing a high level of adenosine deaminase in a patient with AIDS: a case report. Respiration. 2010;79(2):153-156.
doi pubmed - Dikensoy O, Namiduru M, Hocaoglu S, Ikidag B, Filiz A. Increased pleural fluid adenosine deaminase in brucellosis is difficult to differentiate from tuberculosis. Respiration. 2002;69(6):556-559.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.











